Last Updated on December 1, 2025 by Bilal Hasdemir

stem cell transplant for multiple myeloma
Recent studies show that life expectancy after a stem cell transplant varies. This depends on the type of cancer and the patient’s health.
A stem cell transplant is a lifesaving option for many, like those with multiple myeloma. Knowing what to expect is key for patients and their families.
The time a patient lives after the transplant can differ a lot. This depends on their health, the cancer type, and the survival rate of the transplant.
Key Takeaways
- Life expectancy varies based on the type of cancer and patient health.
- Stem cell transplant is a critical treatment for multiple myeloma.
- Understanding the prognosis is vital for patients and their families.
- Survival rates are influenced by several factors, including overall health.
- Patients should consult their healthcare provider for personalized information.
Understanding Stem Cell Transplants
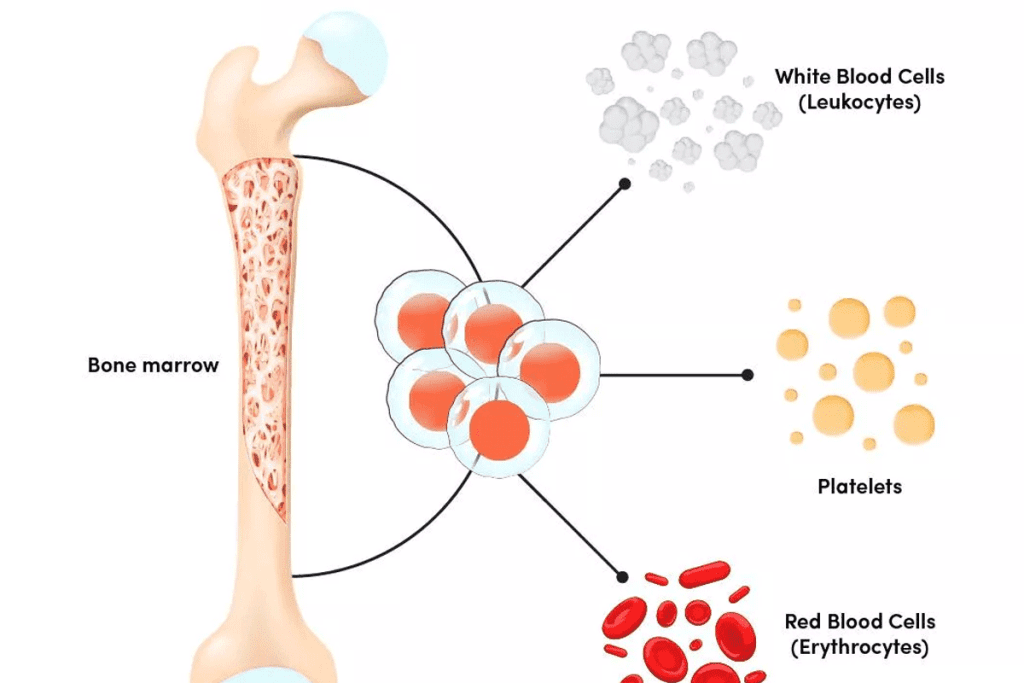
Stem cell transplantation brings new hope to those fighting certain cancers, like multiple myeloma. It replaces damaged bone marrow with healthy stem cells. These can come from the patient (autologous) or a donor (allogeneic).
What are Stem Cell Transplants?
Stem cell transplants, also known as bone marrow transplants, help the body make healthy blood cells. They are a key treatment for patients with multiple myeloma and other blood cancers.
Key aspects of stem cell transplants include:
- The ability to regenerate healthy blood cells
- The use of high-dose chemotherapy followed by stem cell rescue
- The use of either autologous or allogeneic stem cells
Types of Stem Cell Transplants
There are two main types of stem cell transplants: autologous and allogeneic. Autologous stem cell transplants use the patient’s own stem cells. These are collected, stored, and then reinfused after chemotherapy. Allogeneic stem cell transplants use stem cells from a donor. This can offer a graft-versus-myeloma effect.
| Transplant Type | Stem Cell Source | Primary Use |
| Autologous | Patient’s own cells | Multiple myeloma, lymphoma |
| Allogeneic | Donor cells | Various hematological malignancies |
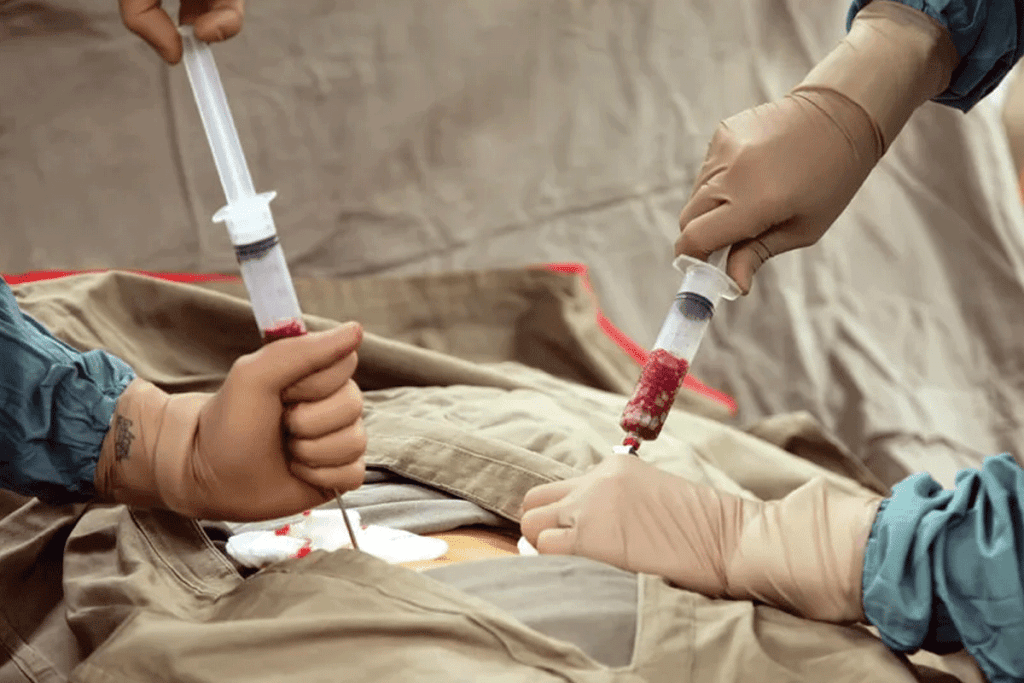
The Transplant Process
The transplant process starts with stem cell mobilization. This is when the patient’s or donor’s stem cells are encouraged to enter the bloodstream. They are then collected and stored.
Next, the patient undergoes conditioning chemotherapy to remove the diseased bone marrow. After that, the stored stem cells are reinfused. They help rebuild the bone marrow.
“Stem cell transplantation has become a cornerstone in the treatment of multiple myeloma, providing a potentially curative option.”
Expert in Hematology
Stem Cell Transplant for Multiple Myeloma
Stem cell transplants are key in treating multiple myeloma. This blood cancer grows in the bone marrow. Multiple myeloma is a type of blood cancer that affects plasma cells.
These transplants help by replacing the bone marrow after chemotherapy. This can lead to a complete remission or longer life.
Why Stem Cell Transplants Are Used for Multiple Myeloma
Stem cell transplants are used for several reasons. They allow for high-dose chemotherapy, which kills more cancer cells. They also replace damaged bone marrow with healthy cells.
The most common transplant is the autologous stem cell transplant. It uses the patient’s own stem cells. This reduces the risk of complications.
Eligibility Criteria for Transplantation
Not all patients with multiple myeloma can get stem cell transplants. The decision depends on age, health, and disease stage. Patients under 65 with few health issues are usually good candidates.
Doctors check the patient’s heart, lungs, and kidneys before the transplant. This ensures they are ready for the process.
Timing of Transplant in Treatment Protocol
The timing of the transplant varies. Some get it early, while others after trying other treatments.
The choice depends on how well the patient responds to initial treatments. Disease characteristics and risk factors also play a role.
| Factor | Influence on Transplant Timing |
| Disease Stage | Early-stage patients may benefit from early transplant, while late-stage patients might require multiple therapies before transplant. |
| Response to Initial Therapy | Patients with a good response may delay transplant, whereas those with a suboptimal response might proceed with transplant sooner. |
| Patient’s Overall Health | Fitness for transplant is a critical determinant of timing. |
Overall Survival Rates After Stem Cell Transplant
Stem cell transplant has shown great promise in treating multiple myeloma. It has become a key part of cancer treatment. The short and long-term survival rates give us insights into its success.
Short-term Survival Statistics
Short-term survival rates are measured at 1-3 years after the transplant. Most patients make it through this period. Some studies show a survival rate of over 80% at three years.
A study in the Journal of Clinical Oncology found an 85% 3-year survival rate for patients with multiple myeloma. This shows the procedure’s short-term success.
Long-term Survival Statistics
Long-term survival rates are measured at 5-10 years after the transplant. Studies show that many patients survive for a long time. Some studies report 5-year survival rates from 50% to over 70%.
A report in Blood found a 65% 5-year survival rate for multiple myeloma patients. This gives a positive outlook for long-term survival.
Factors Affecting General Survival Rates
Many factors affect survival rates after stem cell transplant. These include the patient’s age, health, and disease stage. Also, donor compatibility and response to pre-transplant treatments matter.
| Factor | Impact on Survival |
| Age | Younger patients tend to have better survival rates. |
| Disease Stage | Patients with earlier-stage disease generally have better outcomes. |
| Donor Compatibility | Better donor compatibility improves survival chances in allogeneic transplants. |
A renowned oncologist noted, “The success of stem cell transplantation depends on many factors. It’s not just the procedure itself but also the patient and the disease.”
“The integration of stem cell transplantation into the treatment paradigm for multiple myeloma has significantly improved patient outcomes, making it a potentially curative option for some.”
An Oncologist
Knowing these factors helps patients and doctors make better treatment choices.
Life Expectancy After Stem Cell Transplant for Multiple Myeloma
Multiple Myeloma Survival Statistics
The life expectancy of patients with multiple myeloma after a stem cell transplant depends on several factors. These include the disease stage and the patient’s age. Knowing these factors is key for both patients and healthcare providers to choose the best treatment.
Survival Statistics Specific to Multiple Myeloma
Thanks to new treatments, including stem cell transplants, survival rates for multiple myeloma have improved. The survival rate can change a lot based on the disease stage and the patient’s health.
Progression-Free Survival
Progression-free survival (PFS) is very important for patients with multiple myeloma after a transplant. It means the disease hasn’t gotten worse during a certain time after treatment. Getting a complete or very good partial response after transplant can greatly improve PFS, which means a longer life.
Overall Survival Rates by Stage and Age
Survival rates after a stem cell transplant for multiple myeloma differ based on the disease stage and age. Generally, those diagnosed early and who are younger tend to live longer. For example, patients under 65 with stage I or II multiple myeloma usually do better than older patients or those with more advanced disease.
Key factors influencing overall survival include:
- Disease stage at diagnosis
- Patient age and overall health
- Response to pre-transplant treatments
- Type of stem cell transplant (autologous vs. allogeneic)
Understanding these factors and their effect on life expectancy after a stem cell transplant for multiple myeloma is vital. It helps in creating treatment plans that fit each patient’s needs, which can lead to better outcomes.
Factors Affecting Life Expectancy Post-Transplant
It’s important to know what affects life expectancy after a stem cell transplant. This knowledge helps both patients and doctors. Several things can change how long a person lives after this treatment.
Age and Overall Health
The age and overall health of a patient are key. Older people or those with health issues might face higher risks. A study found that older age increases the risk of death after a transplant.
Disease Stage and Characteristics
The stage and characteristics of the disease matter a lot. Patients with aggressive disease or who have relapsed might do differently than those treated early. This shows how important the disease’s stage is.
Donor Compatibility (for Allogeneic Transplants)
For allogeneic transplants, matching the donor and recipient is vital. Better matches can lead to better results and longer life. Doctors say choosing the right donor is key to success.
Response to Pre-Transplant Treatments
How well a patient does before the transplant also matters. Those who respond well to treatments before the transplant might do better after it. This shows the importance of pre-transplant care.
In summary, life expectancy after a stem cell transplant depends on many things. These include the patient’s age, disease, donor match, and how well they respond to treatments before the transplant. Knowing these factors helps in making better treatment choices.
Autologous vs. Allogeneic Transplants: Survival Differences
autologous vs allogeneic stem cell transplant survival rates
It’s key to know the difference between autologous and allogeneic stem cell transplants for treating multiple myeloma. The choice depends on the patient’s health and the myeloma’s specifics.
Comparing Survival Rates Between Transplant Types
Autologous transplants use the patient’s own stem cells. Allogeneic transplants use a donor’s stem cells. Survival rates vary greatly between these two methods.
A study in the Journal of Clinical Oncology found a 5-year survival rate of about 55% for autologous transplants. Allogeneic transplants had a rate of around 40% for multiple myeloma patients.
Risk-Benefit Analysis for Each Approach
Autologous transplants have a lower risk of GVHD but might have a higher relapse risk. This is because the graft could contain malignant cells.
Allogeneic transplants have a higher GVHD risk but might offer a graft-versus-myeloma effect. This could lower the relapse risk.
| Transplant Type | Risk of GVHD | Relapse Risk | Treatment-Related Mortality |
| Autologous | Low | Higher | Lower |
| Allogeneic | Higher | Lower | Higher |
When Each Type is Recommended for Multiple Myeloma
The choice between autologous and allogeneic transplants depends on several factors. These include the patient’s age, health, and disease stage.
Autologous transplants are often recommended for those who can handle high-dose chemotherapy and have responsive disease. Allogeneic transplants are considered for younger patients with aggressive disease or those who have relapsed after an autologous transplant.
The decision should be made based on the patient’s unique situation. It’s about weighing the benefits and risks of each transplant type.
Preparing for Transplant: Impact on Outcomes
Getting ready for a stem cell transplant is key to its success. The right preparation, like conditioning and mobilizing stem cells, greatly affects how well a patient does.
Pre-transplant Conditioning Regimens
Before the transplant, treatments aim to kill cancer cells and weaken the immune system. This makes it easier for the new stem cells to take hold. These treatments often include chemotherapy and radiation.
Key components of pre-transplant conditioning regimens include:
- Chemotherapy to kill cancer cells
- Immunosuppression to prevent graft rejection
- Assessment of organ function to ensure the patient can tolerate the treatment
A top hematologist, says, “The goal of pre-transplant conditioning is to create an environment where the transplanted stem cells can engraft and produce healthy blood cells.”
“The conditioning regimen is a critical step in the transplant process, as it directly impacts the patient’s ability to recover and achieve long-term remission.” – An Expert Hematologist
Stem Cell Mobilization Techniques
Mobilizing stem cells means getting them to move from the bone marrow into the blood. This makes it easier to collect them for the transplant. Good mobilization techniques are vital for getting enough stem cells.
Common stem cell mobilization techniques include:
- Growth factor administration to stimulate stem cell production
- Chemotherapy to mobilize stem cells
- Combination regimens for enhanced mobilization
Patient Preparation and Its Effect on Survival
Preparing a patient for transplant involves more than just medical treatment. It also includes getting them physically fit, nutritionally sound, and mentally ready. Good preparation can greatly improve survival chances by lowering the risk of complications and boosting overall health.
Key aspects of patient preparation include:
- Nutritional counseling to optimize the patient’s diet
- Physical conditioning to improve overall health
- Psychological support to address anxiety and stress
By focusing on these important areas, healthcare teams can help patients do better after a stem cell transplant.
Complications That Can Impact Life Expectancy
The time after a stem cell transplant is very important. Several complications can happen and affect how long a person lives. Stem cell transplants can cure many diseases, but they also have risks that can shorten a patient’s life.
Graft-Versus-Host Disease
Graft-versus-host disease (GVHD) is a big problem after an allogeneic stem cell transplant. The donated stem cells see the recipient’s body as foreign and attack it. GVHD can be acute or chronic, with chronic GVHD affecting quality of life and survival more.
Managing GVHD is key to avoid damage to organs like the liver, skin, and gut.
Infections and Immune System Recovery
Infections are a big worry after stem cell transplantation. The treatments used before the transplant weaken the immune system. It takes time for the immune system to recover, leaving patients open to infections.
Preventive measures and close monitoring are vital to fight off and manage infections well.
Organ Damage and Secondary Cancers
Organ damage can happen from the treatments before the transplant and GVHD. There’s also a risk of secondary cancers because the treatments can harm the patient’s cells’ DNA. It’s important to keep an eye on these risks and manage them over time.
Relapse Risks
Relapse is a big worry after stem cell transplantation for multiple myeloma. The chance of relapse depends on several things, like the disease stage at transplant and the type of transplant. Monitoring and maintenance therapy after transplant are key to lowering relapse risk and improving survival.
In summary, while stem cell transplants are a valuable treatment for multiple myeloma, they come with risks that can affect life expectancy. It’s important to understand these risks and manage them well to improve patient outcomes.
Multiple Myeloma Relapse After Stem Cell Transplant
Multiple myeloma relapse after a stem cell transplant is a big worry. It needs close watching and handling. Relapse can happen for many reasons, like leftover disease or treatment resistance.
Relapse Rates and Timeframes
Research shows that relapse rates for multiple myeloma patients after transplant vary. The disease stage at diagnosis, how well the patient responds to treatment before transplant, and the transplant type all play a role.
- Early Relapse: This happens in the first year after transplant. It usually means a worse outlook.
- Late Relapse: This occurs after the first year. It might suggest a less aggressive disease.
Treatment Options After Relapse
When relapse happens, treatment plans are made just for that person. They take into account past treatments and how aggressive the relapse is.
- Salvage Therapies: These include new drugs and combos aimed at keeping the disease in check.
- Clinical Trials: They offer new treatments that aren’t available yet.
Second Transplants and Their Outcomes
Some patients might get a second stem cell transplant. This is for those who did well with the first transplant and had a long break without disease.
Impact on Overall Survival
Relapse affects how long a patient can live. Outcomes depend on when and how aggressive the relapse is, and how well treatments work after that.
It’s key to understand relapse and treatment options to manage multiple myeloma well.
Post-Transplant Care and Monitoring
post-transplant care and monitoring
Good care after a stem cell transplant is key to managing problems and boosting survival chances. This care phase is vital to ensure the transplant works well and to catch any issues early.
Follow-up Schedule and Testing
Patients must stick to a strict follow-up plan after a stem cell transplant. They need regular doctor visits, blood tests, and other tests to check the transplant’s success and their health. Regular monitoring helps spot problems early, so they can be fixed quickly.
Maintenance Therapy Approaches
Maintenance therapy is used after a transplant to keep the treatment working and prevent the disease from coming back. The type of therapy depends on the patient’s situation and the transplant type. Tailored maintenance therapy can greatly improve outcomes by lowering relapse risk and managing side effects.
Managing Long-term Complications
Long-term issues can happen after a stem cell transplant, like graft-versus-host disease, infections, and organ damage. It’s important to manage these problems well to improve life expectancy after BMT. This involves using medicine, making lifestyle changes, and keeping a close eye on the patient’s health.
Impact of Post-Transplant Care on Survival
The quality of care after a transplant greatly affects survival rates. By following a detailed follow-up plan, getting the right maintenance therapy, and handling complications well, patients can greatly boost their survival chances. Comprehensive post-transplant care is vital for getting the most out of the transplant.
Recent Advances Improving Survival Outcomes
New developments in stem cell therapy are leading to better survival rates and quality of life for patients. The field of stem cell transplantation is growing fast. This is thanks to new medical technologies and treatment methods.
New Conditioning Regimens
One big improvement is in conditioning regimens before stem cell transplant. These new regimens aim to cut down on harmful side effects. At the same time, they keep or boost the treatment’s effectiveness.
Studies show these regimens are helping patients by reducing complications.
Maintenance Therapies
Maintenance therapies after transplant are key in managing multiple myeloma. Treatments like lenalidomide have been shown to help patients live longer and avoid disease progression. The right maintenance therapy depends on the patient’s risk and how they respond to the initial transplant.
Combination Approaches
Using combination approaches is another big step forward. This means combining stem cell transplant with other treatments. These can include proteasome inhibitors, immunomodulatory drugs, or monoclonal antibodies.
This combination has shown to improve survival chances.
Benefits of Combination Therapies
- Enhanced disease control
- Improved survival rates
- Potential for reduced relapse rates
CAR T-cell Therapy Integration
CAR T-cell therapy, a type of immunotherapy, is showing great promise in treating multiple myeloma. It’s most promising for patients who have not responded well to other treatments. Research into combining CAR T-cell therapy with stem cell transplant is ongoing.
Early results are very encouraging, suggesting better outcomes for patients.
“The integration of CAR T-cell therapy with stem cell transplant represents a promising frontier in the treatment of multiple myeloma, promising better survival chances.”
As research keeps moving forward, the future of stem cell transplantation looks bright. There’s hope for even better survival rates and quality of life for patients.
Conclusion
Life expectancy after a stem cell transplant depends on many things. These include the type of transplant, the patient’s health, and the disease itself. For those with multiple myeloma, getting a stem cell transplant is a key treatment. It can greatly increase their life expectancy.
The survival rate after a stem cell transplant can vary. It’s important for both patients and doctors to understand what affects it. Thanks to recent advances, people with multiple myeloma are living longer. More research aims to make stem cell transplant even more effective.
As medical science keeps moving forward, we can expect better outcomes from stem cell transplants. This brings hope to those with multiple myeloma and others who might need this treatment.
FAQ
What is the life expectancy after a stem cell transplant for multiple myeloma?
Life expectancy after a stem cell transplant for multiple myeloma depends on several factors. These include the disease stage, overall health, and treatment response. Studies show that the median survival rate is about 5-7 years. Some patients may live up to 10-15 years or more.
What are the different types of stem cell transplants used for multiple myeloma?
There are two main types of stem cell transplants for multiple myeloma. Autologous transplants use the patient’s own stem cells. Allogeneic transplants use stem cells from a donor. Autologous transplants are more common for multiple myeloma.
What is the success rate of stem cell transplants for multiple myeloma?
The success rate of stem cell transplants for multiple myeloma varies. It depends on the disease stage and overall health. Autologous transplants can achieve complete remission in 30-50% of patients. The median time without disease progression is about 2-3 years.
What are the possible complications of stem cell transplants for multiple myeloma?
Stem cell transplants for multiple myeloma can have complications. These include graft-versus-host disease, infections, organ damage, and secondary cancers. Around 50-70% of patients experience relapse after autologous transplant.
How does age affect life expectancy after stem cell transplant for multiple myeloma?
Age is a big factor in life expectancy after stem cell transplant for multiple myeloma. Older patients generally have lower survival rates and higher risks of complications. But, advances in transplant techniques and care have improved outcomes for older patients.
What is the role of maintenance therapy after stem cell transplant for multiple myeloma?
Maintenance therapy is used after stem cell transplant to keep the disease in remission. It helps prevent relapse. Lenalidomide and bortezomib are common maintenance therapies. They have been shown to improve survival in multiple myeloma patients.
Can multiple myeloma relapse after stem cell transplant?
Yes, multiple myeloma can relapse after stem cell transplant. The relapse rate depends on the disease stage and treatment response. Treatment options for relapse include salvage therapies, second transplants, and CAR T-cell therapy.
What is the impact of post-transplant care on survival outcomes for multiple myeloma patients?
Post-transplant care is key to maintaining remission and preventing complications. Regular follow-up, maintenance therapy, and managing long-term complications can improve survival for multiple myeloma patients.
How does CAR T-cell therapy compare to stem cell transplant for multiple myeloma?
CAR T-cell therapy is a new approach that genetically modifies T-cells to target cancer cells. It has shown promising results in multiple myeloma. But, its role in treatment is evolving. Stem cell transplant remains a standard treatment for eligible patients.
What are the recent advances in stem cell transplant that are improving survival outcomes for multiple myeloma patients?
Recent advances in stem cell transplant are improving survival outcomes for multiple myeloma patients. These include new conditioning regimens, maintenance therapies, and combination approaches. The integration of CAR T-cell therapy is also being explored.
References
- Perrot, A., et al. (2025). Survival, years of life lost and attrition rates in multiple myeloma patients. Leukemia & Lymphoma, [Advance Publication].