Multiple myeloma is a disease that affects thousands in the U.S. each year and involves the bone marrow. For many, a stem cell transplant is a treatment option that offers a chance at remission or even a cure by replacing damaged marrow with healthy stem cells, often leading to longer remission and improved survival outcomes.
The bone marrow transplant procedure replaces damaged bone marrow with healthy stem cells. These can come from the patient or a donor. This process can save lives but comes with its own set of challenges.
It’s important for patients and their families to understand the stem cell transplant process. It’s more than just the procedure. It includes preparation, recovery, and managing possible complications.
Key Takeaways
- A stem cell transplant is a treatment option for multiple myeloma and other blood disorders.
- The bone marrow transplant procedure involves replacing damaged marrow with healthy stem cells.
- The stem cell transplant process can be complex and challenging.
- Understanding the process is key for patients and their families.
- Preparation, recovery, and managing complications are important parts of the transplant experience.
Understanding Bone Marrow and Stem Cell Transplants
Learning about bone marrow and stem cell transplants is key for those thinking about this treatment. These transplants are a big help in treating many blood diseases and some cancers.
What is a Stem Cell Transplant?
A stem cell transplant replaces a patient’s bad or damaged stem cells with good ones. Stem cells can turn into many types of cells, like blood cells. The goal is to help the body make healthy blood cells and treat the disease.
Types of Transplants: Autologous vs. Allogeneic
There are two main types of stem cell transplants: autologous and allogeneic. An autologous transplant uses the patient’s own stem cells. These cells are taken, stored, and then put back after treatment.
An allogeneic transplant uses stem cells from someone else. This can be a family member, an unrelated donor, or umbilical cord blood. Allogeneic transplants are often for patients with leukemia or other bone marrow problems.
| Transplant Type | Source of Stem Cells | Common Uses |
| Autologous | Patient’s own cells | Multiple myeloma, lymphoma |
| Allogeneic | Donor cells | Leukemia, bone marrow failure syndromes |
When is a Stem Cell Transplant Necessary?
A stem cell transplant is needed for certain diseases, like some cancers and bone marrow failures. The decision to have a transplant depends on the patient’s health, disease type, and how well they’ve responded to treatments.
Choosing between autologous and allogeneic transplant depends on the patient’s condition and disease type. Studies show that the transplant type can greatly affect patient results (Source: US Pharm. 2025;50(7/8):52-58).
The Complete Stem Cell Transplant Process
Stem cell transplantation is a detailed process. It includes checking the patient’s health before the transplant, finding a good donor, and preparing the body for the transplant. This careful approach helps patients with blood diseases get the best treatment.
Pre-Transplant Evaluation and Testing
Patients get checked thoroughly before a stem cell transplant. They have blood tests, imaging, and heart checks. These tests look for any health risks or problems.
Comprehensive testing is key to knowing the patient’s health. It helps doctors plan the transplant and watch for side effects.
Finding a Donor Match
For an allogeneic transplant, finding a matching donor is vital. Histocompatibility testing matches the donor’s HLA type with the patient’s. This reduces the risk of GVHD.
Finding a donor can take a lot of time. It might involve family members, unrelated donors, or umbilical cord blood. The donor matching process is complex and needs careful thought to find the best match.
Timeline of a Typical Transplant
The time needed for a stem cell transplant varies. It depends on the transplant type and the patient’s health. Usually, it takes weeks to months from the first check-up to the transplant.
Knowing the transplant timeline helps patients prepare. It includes getting ready for the transplant and recovery. It’s a series of steps from preparing the body to caring for it after the transplant.
Preparing for Transplant: Conditioning Regimen
A conditioning regimen gets a patient ready for a stem cell transplant by removing diseased cells. This step is key for the transplant’s success. It makes room for new stem cells to grow and produce healthy blood cells.
High-Dose Chemotherapy
High-dose chemotherapy is a big part of the conditioning regimen. It uses strong chemotherapy drugs to kill the old bone marrow and sick cells. This treatment can cause side effects like nausea, hair loss, and tiredness.
Table 1: Common Side Effects of High-Dose Chemotherapy
| Side Effect | Frequency | Management Strategy |
| Nausea | High | Anti-nausea medication |
| Hair Loss | High | Counseling, scalp cooling |
| Fatigue | Very High | Rest, nutritional support |
Radiation Therapy
Some conditioning regimens also include radiation therapy. This uses high-energy rays to kill sick cells. The choice to use radiation therapy depends on the disease type and where it is in the body.
“Radiation therapy is often used with chemotherapy to make sure all sick cells are killed before the transplant.”
Pain Management During Conditioning
Managing pain well is very important during the conditioning phase. Patients might feel pain from the chemotherapy, radiation, or their disease. To manage pain, doctors use medicine, relaxation methods, and nutrition.
Pain management is a complex process that needs constant monitoring and adjusting of treatment plans.
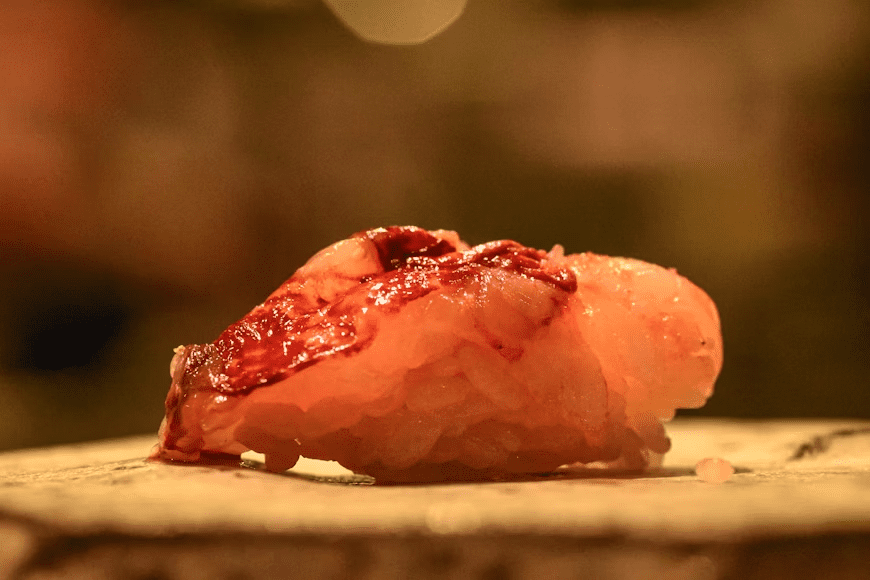
How Are Stem Cells Harvested? Collection Methods
Stem cells can be taken in several ways, each with its own steps and thoughts. The method picked depends on the patient’s health, the transplant type, and where the stem cells come from.
Bone Marrow Harvesting Procedure
Bone marrow harvesting takes stem cells from the bone marrow. This is done under general anesthesia to reduce pain. A needle is put into the hipbone or sternum to get the bone marrow.
The bone marrow is then processed to get the stem cells ready for transplant.
Peripheral Blood Stem Cell Collection
Peripheral blood stem cell collection is another way to get stem cells. It uses drugs to make stem cells move from the bone marrow to the blood. Then, apheresis is used to take the stem cells from the blood and put them back in the body.
Umbilical Cord Blood Collection
Umbilical cord blood collection takes stem cells from the umbilical cord after a baby is born. It’s safe and painless because it uses blood that would be thrown away. The cord blood is full of stem cells and can be used for transplants in related or unrelated people.
Each method has its benefits and is chosen based on the patient’s needs and the transplant type. Knowing about these ways to get stem cells is key for patients getting stem cell transplants.
Pain Levels During Stem Cell Harvesting for Donors
Stem cell harvesting is key in transplantation, but donors worry about pain. Knowing what to expect can ease their fears.
Donor Experience During Bone Marrow Extraction
Bone marrow extraction is a surgery to take marrow from the hip bone. Donors are usually under anesthesia, so they don’t feel pain during the procedure. But, post-operative pain is common and can be treated with medicine.
Pain levels differ, but most donors report temporary soreness or stiffness in the lower back or hip region.
Discomfort During PBSC Collection
Peripheral Blood Stem Cell (PBSC) collection is a non-surgical method. It involves taking stem cells from the blood. Donors might feel some discomfort from the needles.
They might also get temporary side effects like fatigue, headache, or dizziness from the stem cell mobilizing drugs.
Recovery Time for Donors
The recovery time depends on the method used. Bone marrow extraction takes a few weeks to fully recover. Donors need to rest and limit activities.
PBSC collection recovery is faster, usually a few days. Knowing the recovery process helps donors prepare for what comes next.
The Transplant Day: What Happens During Stem Cell Transplant
The stem cell transplant procedure is a complex process. It involves putting harvested stem cells into the patient’s body. This day is a big milestone in the treatment journey, filled with hope and careful medical attention.
The Actual Transplant Procedure
The transplant procedure is medically straightforward, though the overall journey is complex. The stem cells are put into the patient’s bloodstream through a special catheter. This can take from 30 minutes to several hours, depending on the amount of stem cells.
Key aspects of the transplant procedure include:
- Monitoring of vital signs throughout the infusion
- Administration of pre-medications to prevent reactions
- Close observation for any signs of infusion-related complications
Pain and Discomfort During Infusion
While most people can handle the infusion, some might feel mild discomfort or pain. Common issues include:
- Chills or fever
- Nausea or vomiting
- Aching or pain at the infusion site
These symptoms are usually managed with medication and close monitoring.
Immediate Post-Infusion Effects
After the infusion, patients are watched closely for any immediate reactions. Some common effects may include:
- Fatigue
- Dizziness
- Mild allergic reactions
These effects are usually short-lived and managed with medical care. The healthcare team gives detailed guidance on what to expect and how to manage symptoms.
In conclusion, while the stem cell transplant procedure is a critical step in treatment, knowing what to expect can help ease concerns. It prepares patients for the journey ahead.
The First 30 Days After Stem Cell Transplant
The first 30 days after a stem cell transplant are key for recovery. They mark the start of the engraftment process. Patients are watched closely for signs of engraftment and managed for side effects. They also get support through the tough recovery time.
Engraftment Process
Engraftment is when the new stem cells start making blood cells. This includes white blood cells, red blood cells, and platelets. It usually starts 2-4 weeks after the transplant. If engraftment is successful, it means the transplant is working right.
Key signs of engraftment include:
- An increase in white blood cell count
- Improved energy levels
- Reduced need for blood transfusions
Common Side Effects and Pain Points
In the first 30 days, patients face many side effects. These come from the conditioning regimen and the transplant itself. Common issues are:
- Mucositis: inflammation of the mucous membranes
- Graft-versus-host disease (GVHD): a complication where the donated stem cells attack the recipient’s body
- Fatigue: persistent tiredness
- Infections: due to a weakened immune system
It’s important to manage these side effects for the patient’s comfort and recovery. The medical team keeps a close eye on the patient and makes changes to treatment plans as needed.
Hospital Stay Duration
The time spent in the hospital varies. It depends on the patient’s condition, the type of transplant, and any complications. On average, patients stay 3-4 weeks after the transplant. They get constant care and support during this time.
| Aspect | Typical Duration or Experience | Notes |
| Engraftment | 2-4 weeks | Variable depending on the transplant type |
| Hospital Stay | 3-4 weeks | Can be longer if complications arise |
| Common Side Effects | Varies | Includes mucositis, GVHD, fatigue, and infections |
Knowing about the first 30 days after a stem cell transplant helps patients and their caregivers. It prepares them for the challenges ahead and helps them see the progress made during recovery.
Managing Pain Throughout the Transplant Journey
Learning to manage pain is key for a better transplant experience. The transplant journey has different stages, each with its own pain challenges.
Medication Options for Pain Control
Managing pain often means using a mix of medicines. Opioids are for severe pain, and nonsteroidal anti-inflammatory drugs (NSAIDs) are for milder pain. The right medicine depends on the patient’s situation, the transplant stage, and how bad the pain is.
| Medication Type | Use Case | Examples |
| Opioids | Severe pain | Morphine, Fentanyl |
| NSAIDs | Mild to moderate pain | Ibuprofen, Acetaminophen |
Non-Pharmaceutical Pain Management Techniques
There are also non-medical ways to manage pain. Relaxation techniques like deep breathing, meditation, and muscle relaxation help. Physical therapy keeps you moving and can lessen pain.
- Relaxation techniques: deep breathing, meditation, progressive muscle relaxation
- Physical therapy: maintaining mobility, reducing pain
- Cognitive behavioral therapy: changing pain perception
When to Alert Your Medical Team About Pain
Telling your medical team about your pain is very important. Severe pain that doesn’t get better with medicine, new or worsening pain, and pain with fever or swelling needs to be told right away.
Knowing about pain management options and talking openly with your healthcare team helps you deal with transplant challenges.
Potential Complications and Their Impact on Pain
The journey after a stem cell transplant can be tough. Some complications can make pain worse. It’s important to know about these complications to manage pain well.
Graft-Versus-Host Disease
Graft-versus-host disease (GVHD) is a big risk after an allogeneic stem cell transplant. Here, the donated stem cells attack the body. GVHD can be acute or chronic, with acute happening in the first 100 days.
Symptoms of GVHD include skin rash, liver problems, and stomach issues. These can all make pain worse.
Key symptoms of GVHD include:
- Skin rash or itching
- Diarrhea or abdominal pain
- Jaundice or liver enzyme elevation
Infections and Immune System Recovery
Infections are a big worry after a stem cell transplant. This is because the treatment weakens the immune system. It takes time for the new immune system to grow strong.
Factors increasing the risk of infection include:
- Prolonged neutropenia
- Immunosuppressive therapy for GVHD
- Central venous catheter presence
Organ Damage and Related Pain
Organ damage is another risk after a stem cell transplant. This can happen due to the treatment, GVHD, or infections. Organs like the liver, lungs, and kidneys can get damaged.
For example, liver damage can cause belly pain and jaundice. Lung problems can lead to breathing issues and chest pain. It’s key to manage these complications to reduce pain and improve life quality.
Long-Term Recovery and Pain Management
Recovering from a stem cell transplant is a big challenge. It involves getting physically better, managing pain, and slowly getting back to normal. These steps are key to a successful recovery.
Timeline for Physical Recovery
The time it takes to recover can differ for everyone. Most people need several months to a year or more to feel fully back. The type of transplant, your health, and any complications can affect your recovery.
Key milestones in physical recovery include:
- Initial recovery phase (0-3 months): Focus on managing immediate post-transplant side effects and beginning to regain strength.
- Intermediate recovery phase (3-6 months): Gradual improvement in energy levels and reduction in pain.
- Advanced recovery phase (6-12 months and beyond): Continued improvement, with many patients returning to their normal activities.
Chronic Pain After Transplant
Chronic pain is a common issue after a stem cell transplant. It can come from GVHD, nerve damage, or other complications. Managing this pain is vital for a better quality of life.
Strategies for managing chronic pain may include:
- Medications: Including pain relievers, anti-inflammatory drugs, and other adjuvant therapies.
- Non-pharmacological interventions: Such as physical therapy, acupuncture, and cognitive-behavioral therapy.
Returning to Normal Activities
Getting back to normal is a big part of recovery. Patients should slowly start doing daily activities based on their energy and health. It’s important to balance activity with rest to avoid exhaustion.
Tips for returning to normal activities:
- Start with low-intensity activities and gradually increase the intensity and duration.
- Listen to your body and rest when needed.
- Follow your healthcare provider’s guidance on safe activities and any necessary precautions.
Psychological Aspects of Transplant Pain
Going through a stem cell transplant is tough, both physically and emotionally. It can really affect a person’s mental health and overall well-being.
Emotional Impact of Physical Pain
Stem cell transplant pain can really get to a patient’s emotions. Chronic pain can make people feel frustrated, anxious, and even depressed. It’s key for doctors to treat both the pain and its emotional side to help fully.
The emotional weight of pain can be too much. So, it’s very important for patients to get mental health support during their transplant.
Coping Strategies for Patients
It’s important for patients to find ways to deal with transplant pain’s emotional side. Mindfulness, meditation, and cognitive-behavioral therapy can help. Also, support groups offer a place to share and find support.
| Coping Strategy | Description | Benefits |
| Mindfulness | Practice being present in the moment | Reduces stress and anxiety |
| Meditation | Focus on calming the mind | Improves emotional regulation |
| Cognitive-Behavioral Therapy | Change negative thought patterns | Enhances coping skills |
Support Resources for Transplant Recipients
Transplant patients need the right support to deal with their emotional pain. This includes mental health help, support groups, online forums, and educational materials. Having all-around support can really help patients cope with their transplant journey.
By understanding the emotional side of transplant pain and providing the right support, doctors can help patients through this tough time.
Advances in Making Stem Cell Transplants Less Painful
New methods for collecting stem cells and better pain management are making transplants easier for patients. Studies show these changes greatly reduce transplant pain (US Pharm. 2025;50(7/8):52-58).
New Collection Methods
Collecting stem cells has become less invasive thanks to new methods. Peripheral Blood Stem Cell (PBSC) collection is now preferred over bone marrow harvesting. It’s less painful and has faster recovery times for donors.
The use of growth factors to mobilize stem cells has made collection more efficient. It’s also less painful for donors.
Reduced-Intensity Conditioning
The use of reduced-intensity conditioning (RIC) regimens is another big step forward. RIC uses lower doses of chemotherapy and radiation. This reduces toxicity and pain, making transplants more bearable for patients, even older adults or those with health issues.
Improved Pain Management Protocols
Pain management has improved with new, more effective protocols. Multimodal pain management strategies combine different pain relief methods. These are now used to manage pain during the transplant process.
These advancements not only make the patient experience better but also lead to better transplant outcomes. Patients can now better tolerate the transplant process.
Conclusion: Weighing the Pain Against the Benefits
Stem cell transplants are complex and can be painful. But for many, the benefits are worth the discomfort. It’s important to understand the pain involved to prepare for the journey ahead.
The pain from stem cell transplants changes throughout the process. It starts with harvesting stem cells and goes through the transplant and recovery. Thanks to new medical tech and pain management, the experience is better now.
Thinking about a stem cell transplant means looking at the pain and the benefits. For many, the chance of a cure or big improvement is worth the challenges of the transplant.
FAQ
What is a stem cell transplant?
A stem cell transplant replaces a patient’s sick or damaged stem cells with healthy ones. This can be done with the patient’s own stem cells or those from a donor.
How are stem cells harvested?
Stem cells are taken from the bone marrow, blood, or umbilical cord. The choice depends on the transplant type and patient’s health. Bone marrow takes stem cells from the hip bone. Peripheral blood stem cell collection uses apheresis to collect stem cells from the bloodstream.
Is stem cell harvesting painful for donors?
Donors might feel some discomfort during harvesting. The pain level changes based on the method. Bone marrow harvesting can cause soreness and tiredness. Peripheral blood stem cell collection may lead to fatigue, bone pain, and headaches due to growth factor injections.
What is the conditioning regimen for a stem cell transplant?
The conditioning regimen prepares the body for the transplant. It uses high-dose chemotherapy and/or radiation to kill diseased stem cells. This also weakens the immune system to prevent transplant rejection.
How long does it take to recover from a stem cell transplant?
Recovery time varies by individual and transplant type. Patients usually stay in the hospital for weeks. It can take months to a year or more to fully recover.
What are the possible complications of a stem cell transplant?
Complications include graft-versus-host disease (GVHD), infections, organ damage, and disease relapse. GVHD happens when donor immune cells attack the patient’s tissues, leading to acute or chronic issues.
How is pain managed during and after a stem cell transplant?
Pain management uses medications like opioids and non-opioids. Techniques like meditation and deep breathing also help manage pain and discomfort.
Can stem cell transplants be painful?
Yes, stem cell transplants can be painful. Pain levels vary by individual and transplant type.
What are the benefits of a stem cell transplant?
Stem cell transplants can cure diseases like leukemia and lymphoma. They also improve quality of life for patients with certain blood disorders.
How do I know if I’m a good candidate for a stem cell transplant?
To see if you’re a good candidate, you’ll need a thorough evaluation. This includes tests to check your health and disease status.
What is the timeline for a typical stem cell transplant?
The timeline varies by individual and transplant type. It includes weeks or months of preparation, the transplant, and recovery.
How does a stem cell transplant work?
A stem cell transplant replaces diseased or damaged stem cells with healthy ones. This allows the body to make healthy blood cells and can cure certain diseases.
What are the differences between autologous and allogeneic transplants?
Autologous transplants use the patient’s own stem cells. Allogeneic transplants use donor stem cells. Autologous transplants are for certain cancers. Allogeneic transplants are for blood disorders or genetic diseases.
Reference
- Almeida, J. S., & Almeida, M. M. (2018). Stem cell transplantation for hematologic malignancies: Challenges and advancements. Journal of Hematology & Oncology, 11(1), 1-13.https://doi.org/10.1186/s13045-018-0635-0
This article discusses the process and challenges of stem cell transplantation, including various treatment regimens and advancements in transplant techniques.
These references provide detailed insights into the stem cell transplant process, from preparation and pain management to complications and recovery strategies.




































