
Many people with coronary artery disease get more than one cardiac stent. A surprising fact is that almost 40% of patients who get one stent will need more later. Answering the limit for how many stents can you have put in your stent in heart at one time (no fixed limit, based on need).
Having more stents in the heart raises the risk of serious problems. It’s important to know how stents work and the heart’s structure. This knowledge helps ensure it’s safe to have multiple heart stent operations.

It’s key to know the heart’s layout, focusing on the coronary arteries, to understand stents. The heart is a muscle that needs blood vessels to work right.
The coronary arteries carry oxygen-rich blood to the heart muscle. This is vital because the heart, like any muscle, needs oxygen to work. These arteries branch from the aorta and circle the heart, giving it the blood it needs.
The coronary arteries have a complex structure. They have many branches that feed different heart parts. The main arteries are the left main coronary and the right coronary artery, with smaller branches off them.
The heart gets blood from three main arteries: the left anterior descending, the left circumflex, and the right coronary artery. These arteries and their branches make sure the heart muscle gets enough oxygen-rich blood.
Blockages often happen at specific spots in the coronary arteries, like where they curve or branch. These blockages are usually because of plaque buildup, or atherosclerosis. The left anterior descending artery and the right coronary artery are common places for blockages.
Knowing about heart anatomy and coronary arteries is important for diagnosing and treating heart disease. This often involves putting stents in to improve blood flow.
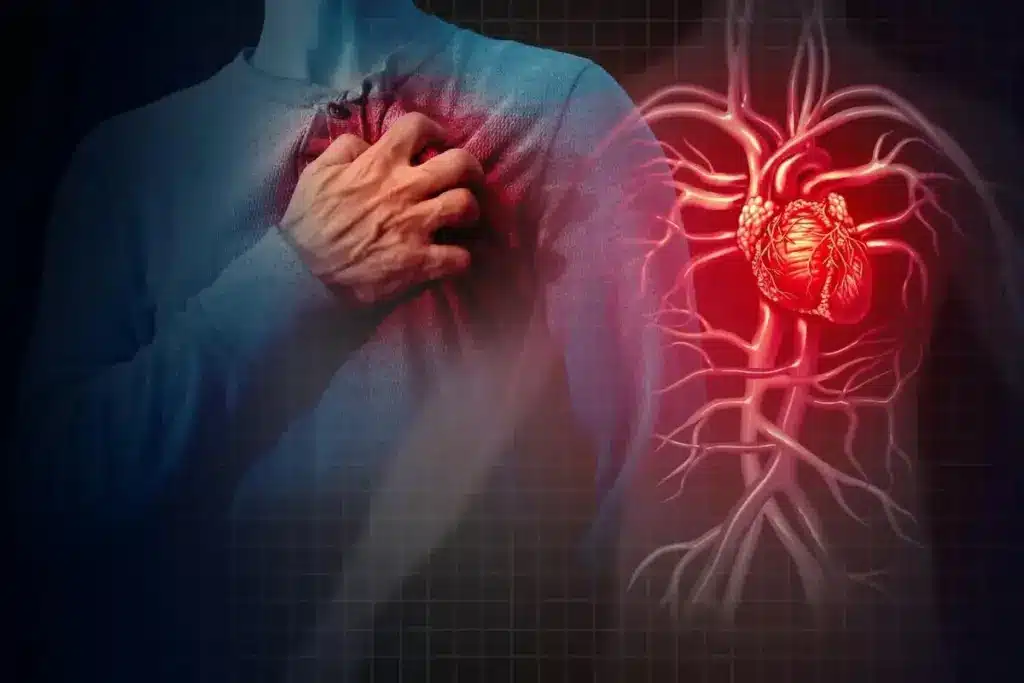
It’s important for people with coronary artery disease to know about stents. A heart stent is a small, mesh-like tube. It keeps the arteries open, improving blood flow to the heart.
Cardiac stents help treat coronary artery disease by keeping arteries open. Their main goal is to:
Stents are used in angioplasty to treat blocked arteries. This procedure uses a balloon to expand the artery and a stent to keep it open. It’s a minimally invasive method that has changed how we treat coronary artery disease.
The process is simple:
Stent technology has come a long way, thanks to new materials and designs. Today’s stents are made from biocompatible materials. They are designed to lower the risk of complications.
Key advancements include:
Heart stents are key in fighting coronary artery disease. There are many types, each suited for different needs. The right stent depends on the patient’s health, the blockage’s size, and past treatments.
Bare metal stents are made of metal mesh. They keep the artery open. But, they might not work as well as newer stents because of a higher chance of restenosis.
Drug-eluting stents have a special coating. This coating helps prevent the artery from getting narrower. They are popular because they lower the risk of restenosis.
Bioresorbable vascular scaffolds are the newest stent type. They support the artery while it heals and then dissolve. This could mean fewer long-term problems.
Choosing the right stent is complex. It involves the patient’s health, the blockage’s location and size, and any past stent use.
|
Stent Type |
Characteristics |
Advantages |
|---|---|---|
|
Bare Metal Stents |
Made from metal mesh |
Traditional option, widely available |
|
Drug-Eluting Stents |
Coated with medication |
Reduces restenosis rates |
|
Bioresorbable Vascular Scaffolds |
Dissolves over time |
Potential reduction in long-term complications |
The table above shows the main heart stent types, their features, and benefits. Knowing these differences helps in choosing the best treatment for coronary artery disease.
Learning about the heart stent procedure can ease worries for those with coronary artery disease. The main goal is to widen a blocked artery. This is usually done under local anesthesia.
Before a stent placement procedure, several steps are taken. These include:
The stent insertion process has several important steps:
The time needed for a stent procedure varies. It can last from 30 minutes to several hours. This depends on the case’s complexity and if multiple stents are used.
After the procedure, patients are closely watched for any immediate issues. This includes:
By knowing about the heart stent procedure and what to expect, patients can better prepare for treatment and recovery.
Understanding the reasons behind using multiple stents is key for those with heart issues. Doctors decide on multiple stents based on the heart disease’s severity, the patient’s health, and the blockage’s details.
Several factors decide if a patient can get multiple stents. These include:
Clinical judgment plays a key role in choosing multiple stent placements. Cardiologists must balance the benefits and risks for each patient.
Usually, one or two stents are used in a single procedure. But, the number can change based on the disease’s complexity.
|
Number of Stents |
Frequency |
Clinical Context |
|---|---|---|
|
1 |
Common |
Single significant blockage |
|
2 |
Frequent |
Multiple blockages in different arteries |
|
3 or more |
Less common |
Complex disease, often requiring staged procedures |
Some patients have had many stents over their lives. These cases often involve complex heart disease and are handled individually.
Studies on multiple stent safety show mixed results. While more stents can raise risks, careful patient choice and new stent tech can help reduce these risks.
A 2021 guideline update said there’s no set limit on stent numbers. It emphasizes the need for personalized treatment plans.
Using multiple stents needs a detailed approach. It must consider the latest research and the patient’s unique situation.
Getting a stent in the heart can be scary for many. But knowing what to expect can help ease worries. The stent procedure is a big deal and needs careful thought and prep.
During the stent procedure, patients are usually awake. They might feel some discomfort, but it’s usually mild thanks to local anesthesia. Some feel a pinch when the catheter goes in or pressure when the stent is placed. After it’s done, most feel relieved. Some might feel a bit sore or bruised where the catheter was.
How long you stay in the hospital after a stent procedure varies. Often, patients go home the same day or after a short stay. Most stay less than 24 hours, while doctors watch for any immediate problems. Your health, the procedure’s complexity, and any issues can affect how long you stay.
Patients often wonder about recovery time, risks, and lifestyle changes. They might ask, “How long will it take to recover?” “Can I be active?” and “Do I need meds?”
Knowing when you might need a stent is key. Look out for symptoms like chest pain, shortness of breath, or feeling tired. If you notice these, see a doctor right away.
Understanding the stent procedure can help patients prepare. It reduces anxiety and improves results.
The choice between stents and coronary artery bypass grafting (CABG) depends on several factors. These include the severity of coronary artery disease, the patient’s overall health, and other medical conditions.
When comparing stents and bypass surgery, the disease’s complexity matters. For example, patients with single-vessel disease might do well with stenting. On the other hand, those with multi-vessel disease often need CABG.
Both stenting and CABG can treat coronary artery disease effectively. Yet, the choice between them depends on the disease’s specifics.
|
Procedure |
Single-Vessel Disease |
Multi-Vessel Disease |
|---|---|---|
|
Stenting |
Effective for simple lesions |
May be used, but CABG often preferred |
|
CABG |
Generally reserved for complex cases |
Often recommended for extensive disease |
Recovery times vary between stenting and CABG. Stenting is usually an outpatient procedure with quick recovery. CABG, on the other hand, requires a longer hospital stay and recovery.
Recovery Time Comparison:
Long-term outcomes and survival rates are key in choosing between stenting and CABG. Both procedures can offer good long-term results. The choice depends on individual patient factors.
The decision between stenting and CABG should be made with a healthcare provider. It should consider the patient’s specific condition, preferences, and lifestyle.
Recovering after getting multiple stents in your heart takes several steps and lifestyle changes. Knowing these is key for a smooth recovery and getting back to normal.
Right after the procedure, you’ll be watched in the hospital for a few hours. This is to make sure there are no problems right away. The early recovery usually includes:
After the stents, you’ll need to follow some rules about what you can do. You should:
Medicine is very important for getting better after stent placement. You’ll likely get:
Getting better long-term means making big changes to keep your heart healthy. This includes:
Seeing your doctor regularly is key to keeping an eye on your stent and heart. This might mean:
By following these tips, you can make the most of your recovery after stent placement. This will help you stay healthy in the long run.
It’s key for patients to know the risks and benefits of heart stents. This knowledge helps them make smart choices about their health. Heart stents are a common treatment for heart disease. There are different types, like bare metal stents and drug-eluting stents.
When thinking about heart stents, talking to doctors is a must. They can help figure out the best treatment for you. Things like how many stents you need and the risks of the procedure matter a lot.
Knowing your options and what might happen can help you take charge of your health. Heart stents can really improve life for people with heart disease. Making informed choices can lead to the best health outcomes.
The heart has three main arteries. These are the left anterior descending artery, the left circumflex artery, and the right coronary artery. They supply blood to the heart muscle.
A heart stent is a small, mesh-like device. It is inserted into a blocked or narrowed artery. This improves blood flow to the heart.
The number of stents varies. It depends on the individual’s situation. Sometimes, multiple stents are placed during one procedure.
There are several types of heart stents. These include bare metal stents, drug-eluting stents, and bioresorbable vascular scaffolds. Each type has its own benefits.
A stent is inserted through a minimally invasive procedure called PCI. A catheter is guided through an artery to the blocked artery. The stent is then deployed to expand the artery.
Recovery time varies. Most people can return to normal activities in a few days to a week. Some activity restrictions may apply, and medication may be prescribed.
Stents can improve blood flow and reduce heart attack risk. But, they are not a guarantee against heart attack. Lifestyle changes and medication may also be needed.
Risks include bleeding, blood clots, and reaction to the stent material. These are possible complications of the procedure.
Stent lifespan varies. It depends on the type of stent, individual health, and lifestyle. Some stents can last many years, while others may need additional procedures.
Yes, multiple stent procedures are possible. The decision to have more stents depends on individual circumstances and the severity of coronary artery disease.
A stent is a minimally invasive procedure to improve blood flow. Bypass surgery involves surgically rerouting blood flow around blocked or narrowed arteries.
There are three main coronary arteries. These are the left anterior descending artery, the left circumflex artery, and the right coronary artery.
Signs include chest pain or discomfort, shortness of breath, and abnormal stress test results. These may indicate the need for a stent procedure.
Check frequency varies. It depends on individual circumstances and the type of stent. Regular follow-up appointments with a healthcare provider are necessary.
Common causes include blood clots, in-stent restenosis, and stent fracture. These can lead to stent failure.
After heart cath with stents, patients may need to avoid heavy lifting, bending, or strenuous activities. This is for a period of time.
National Center for Biotechnology Information. Evidence-Based Medical Insight. Retrieved from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6981347/
Subscribe to our e-newsletter to stay informed about the latest innovations in the world of health and exclusive offers!