Last Updated on December 1, 2025 by Bilal Hasdemir
Did you know that nearly 70,000 brain biopsies are done every year in the U.S.? A lot of these use the stereotactic brain biopsy method. This method is a big deal in neurosurgery because it lets doctors take precise samples from the brain.
We use stereotactic neurosurgery to find and treat brain problems with great accuracy. It has changed neurosurgery a lot. Now, we can treat brain issues without hurting too much of the brain around it.
Stereotactic biopsy uses the latest in imaging and surgery. It’s a key part in finding and treating brain diseases.
Key Takeaways
- Understanding the stereotactic method and its application in brain biopsy procedures.
- The importance of precision in neurosurgery for diagnosing brain lesions.
- How stereotactic neurosurgery enhances treatment outcomes.
- The role of advanced imaging in stereotactic brain biopsy.
- Benefits of minimally invasive diagnostic tools in neurosurgery.
Understanding Stereotactic Methodology in Neurosurgery

Stereotactic neurosurgery has changed brain surgery a lot. It helps find and target specific brain areas with great accuracy. This method is now key in modern brain surgery.
Definition and Basic Principles
Stereotactic neurosurgery uses a three-dimensional system to find targets in the brain. It lets neurosurgeons do precise surgeries, reducing harm to other brain parts.
The stereotactic device is very important. It helps place surgical tools exactly where they need to be. This is done by attaching a frame to the patient’s head.
Historical Development of Stereotactic Techniques
The start of stereotactic techniques was in the early 20th century. They were first used in animals for research.
In the 1940s, the first human stereotactic device was made. This was a big step for neurosurgery. Later, stealth MRI and other imaging tech made these surgeries even better.
The Technology Behind Stereotactic Brain Procedures
The precision of stereotactic brain procedures comes from advanced technology. We use many tools and techniques to ensure these surgeries are accurate and effective.
Stereotactic Frames and Frameless Systems
Older methods used frame-based systems, attaching a rigid frame to the patient’s head. But now, we have frameless systems for more comfort and flexibility. These systems use imaging and registration to match the accuracy of the old frames without the need for a fixed frame.
Frameless systems are great for complex procedures or when comfort is key. The choice between the two depends on the procedure and the patient’s needs.
Imaging Technologies in Stereotactic Navigation
Imaging technologies are key in stereotactic navigation. We use MRI and CT scans for detailed images. MRI’s soft-tissue contrast is unmatched for brain imaging.
Advanced imaging like MRI brain stealth helps us navigate the brain with great accuracy. This is vital for procedures near critical brain areas.
Imaging Modality | Advantages | Applications in Stereotactic Surgery |
MRI | Excellent soft-tissue contrast, high resolution | Brain tumor biopsies, deep brain stimulation |
CT | Fast acquisition, good for bony structures | Stereotactic frame registration, certain tumor localizations |
Computer-Assisted Planning Software
Computer-assisted planning software is vital in modern stereotactic surgery. It uses algorithms to plan the best path and execute the procedure with precision. This software lets us simulate the procedure and make adjustments before surgery.
The mix of advanced imaging, stereotactic frames or frameless systems, and planning software has made stereotactic brain procedures safer and more accurate. As technology improves, we’ll see better patient outcomes and more uses for stereotactic techniques.
Types of Stereotactic Brain Procedures
Stereotactic brain procedures are key in neurosurgery. They help diagnose and treat various conditions. These methods target specific brain areas with great care, reducing damage to other tissues.
Diagnostic Procedures
Diagnostic stereotactic procedures help get tissue samples for tests. Stereotactic needle biopsy is a main tool for this. It uses a frame or system to guide a needle to the right spot.
- Precise targeting of lesions
- Minimally invasive, reducing recovery time
- High diagnostic yield
Therapeutic Interventions
Therapeutic stereotactic procedures treat brain conditions. Stereotactic radiosurgery is a non-invasive method that uses precise radiation. We also use these methods for deep brain stimulation.
The benefits include:
- Minimally invasive, reducing the risk of complications
- High precision in targeting the affected area
- Effective in treating conditions that are difficult to manage with traditional surgery
Stereotactic Biopsy: A Minimally Invasive Diagnostic Tool
Stereotactic biopsy is a key tool in neurosurgery. It’s a way to look at brain lesions without open surgery. This method cuts down the risk of problems.
When Is a Stereotactic Biopsy Necessary?
This biopsy is great for hard-to-reach brain areas. It’s safe and precise for getting tissue samples. This helps find tumors, infections, or inflammation.
It’s a good choice when MRI or CT scans show lesions that are hard to get to. Or when a patient can’t handle more invasive surgery.
Types of Brain Lesions Suitable for Stereotactic Biopsy
Stereotactic biopsy works on many brain lesions. It’s best for small, deep, or in hard-to-reach areas. It’s used for gliomas, metastatic tumors, and some infections or inflammation.
Advantages Over Traditional Open Biopsies
This method is less invasive. It means less harm to the patient and faster recovery. It also aims more precisely, avoiding damage to other brain areas.
Pre-Procedure Preparation for Stereotactic Brain Procedures
Stereotactic brain procedures need careful preparation to reduce risks and improve care. This includes a detailed patient evaluation, precise imaging, and clear instructions for the patient.
Patient Evaluation and Selection
Checking the patient’s health and medical history is key. We look at the brain lesions or conditions too. This helps us decide if the patient is right for the procedure and if there are any risks.
Imaging Requirements and Protocols
Good imaging is vital for success. We use MRI and CT scans to get clear images of the brain. These images help us plan the procedure carefully, aiming for accuracy and avoiding damage to other brain areas.
Patient Instructions and Expectations
Talking clearly with the patient is important. We tell them about what to do before the procedure, like managing medications and following dietary rules. We also explain what they can expect during and after the procedure, including possible side effects and the recovery process.
Pre-Procedure Preparation | Description |
Patient Evaluation | Assessment of overall health and medical history |
Imaging Protocols | Use of MRI and CT scans for precise targeting |
Patient Instructions | Guidance on pre-procedure preparations and expectations |
Step-by-Step Process of a Stereotactic Brain Biopsy
Learning about the steps of a stereotactic brain biopsy can ease worries for both patients and doctors. We’ll explore the key steps in this precise, non-invasive test.
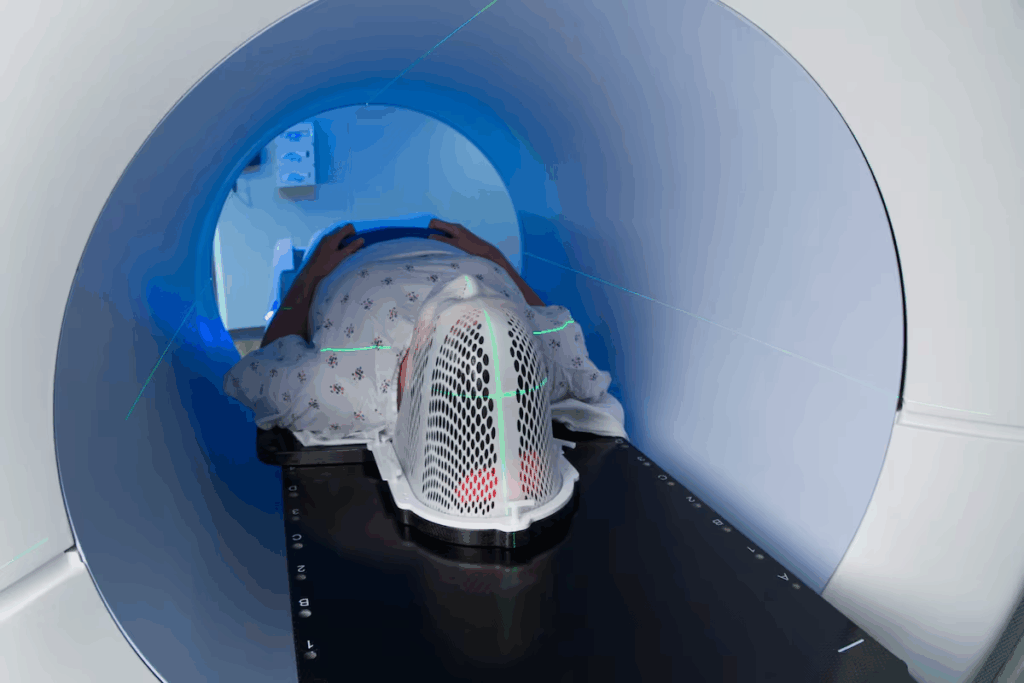
Frame Placement and Imaging
The first step is putting a stereotactic frame on the patient’s head. This frame is fixed to the skull to keep it steady during the procedure. Next, we use MRI or CT scans to see the brain and the target lesion. These images help us plan the best path for the biopsy needle.
Target Calculation and Trajectory Planning
We use special computer software to find the exact spot in the brain we need to reach. We figure out the best spot on the skull and the path to the lesion without harming nearby brain tissue. The path is carefully planned to avoid important structures and ensure safe access.
Anesthesia Considerations
Most brain biopsies are done under local anesthesia, with the patient awake. Sometimes, we use sedation to help the patient relax. The choice of anesthesia depends on the patient’s health and the procedure’s needs.
“The precision and accuracy of stereotactic brain biopsy make it an invaluable tool for diagnosing brain lesions and tumors.”
Expert Opinion
Biopsy Execution and Specimen Collection
After planning the path and preparing the patient, we do the biopsy. We insert a biopsy needle through a small hole in the skull. The needle is guided to the target lesion using the frame and imaging. We then take tissue samples for examination to find out the diagnosis.
Step | Description |
Frame Placement | Fixing a stereotactic frame to the patient’s head |
Imaging | Conducting MRI or CT scans to visualize the brain |
Target Calculation | Determining the precise coordinates of the target lesion |
Biopsy Execution | Inserting a biopsy needle to collect tissue samples |
By following these steps, we ensure the biopsy is done safely and accurately. This gives us the information we need to plan the next steps in treatment.
Frame-Based vs. Frameless Stereotactic Techniques
Stereotactic techniques have changed a lot, moving from old frame-based systems to new frameless ones. This change came from better imaging and computers. Now, neurosurgery is more precise and flexible.
Traditional Frame-Based Systems
For years, traditional frame-based systems were key in neurosurgery. They use a fixed frame on the patient’s head for precise navigation. This frame is attached with pins or screws, keeping everything steady during surgery.
These systems are trusted for many neurosurgical tasks, like biopsies and removing tumors. They are known for their accuracy and reliability.
Modern Frameless Navigation
Frameless stereotactic navigation is a big step forward in neurosurgery. It doesn’t need a fixed frame. Instead, it uses advanced imaging and tracking to guide tools.
This method uses pre-surgery images matched to the patient’s body. It’s more comfortable for patients and surgeons, allowing for more movement during surgery.
Comparative Accuracy and Applications
Frame-based and frameless systems each have their own benefits and drawbacks. Frame-based systems are very accurate and have been the top choice in neurosurgery. But, they can be hard to use and uncomfortable for patients.
Frameless systems are more flexible and comfortable for patients. They are as accurate as frame-based systems in many cases. The choice between them depends on the surgery, the patient, and the surgeon’s preference.
Post-Procedure Care and Monitoring
After a brain procedure, careful care is key. We watch for problems and help with recovery. Our goal is to make sure patients do well.
Immediate Post-Operative Care
Right after surgery, we keep a close eye on patients. We check their brain function, heart rate, and overall health. They usually stay in a special area for a few hours to a whole night.
Our team looks for any signs of trouble. This includes changes in brain function, bleeding, or other bad reactions. We also make sure patients are comfortable by giving them the right pain medicine.
Potential Early Complications to Monitor
Even though brain procedures are usually safe, we need to watch for some early problems. These can be:
- Changes in brain function or thinking
- Bleeding or hemorrhage at the surgery site
- Infection, though rare
- Seizures, in some cases
We are ready to handle these issues quickly. This way, we can stop any big problems before they start.
Discharge Instructions and Follow-Up
Before leaving the hospital, patients and their families get clear instructions. They learn about caring for the wound, taking medicine, and watching for signs of trouble. We also plan follow-up visits to check on their recovery.
We care for our patients long after the surgery. Our focus is on helping them recover and stay healthy in the long run.
Care Aspect | Immediate Post-Operative | Home Care |
Monitoring | Close observation in recovery or ICU | Family/caregiver observation for complications |
Pain Management | Medications as needed | Prescribed pain management regimen |
Follow-Up | Before discharge, schedule follow-up | Attend scheduled follow-up appointments |
We offer full care and monitoring after a brain procedure. This helps our patients get through a tough time. We aim for the best results and a smooth recovery.
Recovery Timeline After Stereotactic Brain Procedures
Recovery after stereotactic brain procedures has a general timeline. But, it can vary from person to person. Knowing this timeline helps manage expectations and ensures a smooth recovery.
First 24-48 Hours After Procedure
The first 24-48 hours are critical. Patients are closely watched for any immediate issues. During this time, they might feel mild discomfort, headache, or nausea. These symptoms can be managed with medication.
Rest is key, and patients should avoid hard activities.
First Week of Recovery
As the procedure’s effects lessen, patients start to feel better. By the first week, most can slowly get back to their usual activities. But, it’s important to follow their healthcare provider’s specific instructions.
During this time, some fatigue or mild cognitive changes are common. These usually go away on their own.
Long-Term Follow-Up and Outcomes
Long-term follow-up care is key to check the procedure’s success and manage long-term effects. Follow-up appointments are set based on the patient’s needs and the procedure’s nature. These visits help healthcare providers track long-term outcomes and address any concerns or complications.
By understanding the recovery timeline and following care instructions, patients can improve their recovery and outcomes after stereotactic brain procedures.
Potential Risks and Complications
It’s important to know the risks of stereotactic brain biopsies before making a decision. We aim to give accurate diagnoses and effective treatments. But, like any surgery, there are risks involved.
Common Side Effects
After a brain biopsy, you might feel a headache, nausea, or be tired. These symptoms are usually mild and go away in a few days. Sometimes, patients might have seizures or problems with their nerves, but this is rare.
We watch our patients closely to help manage these side effects.
Hemorrhage and Neurological Complications
Bleeding at the biopsy site is a serious risk, though it’s rare. We do everything we can to avoid this, like choosing the right patients and being very careful during the procedure. Problems with the nerves can also happen, either from the biopsy or the frame used.
We look at each case carefully to understand these risks.
Infection and Other Risks
Infection is a risk, but we use clean techniques and antibiotics to lower it. Rarely, patients might have a reaction to the anesthesia. There’s also a chance of not finding the right spot during the biopsy, which might mean doing it again.
We use the latest imaging and navigation to try to avoid these problems.
Even with these risks, the chance of complications from a brain biopsy is low. We talk openly with our patients about these risks so they can make the best choice for their treatment.
Accuracy and Diagnostic Yield of Stereotactic Biopsies
It’s important for doctors to know what affects the accuracy of stereotactic biopsies. The success of these tests depends on many technical and procedural factors.
Factors Affecting Accuracy
Several factors influence the accuracy of these biopsies. These include the precision of the equipment used, the quality of the images, and the neurosurgeon’s skill.
Imaging quality is key. High-quality images help target the lesion more accurately. Also, the registration process between images and the patient’s body must be precise for correct targeting.
Interpreting Biopsy Results
Doctors from different fields must work together to understand biopsy results. The histopathological diagnosis is vital for deciding what to do next for the patient.
Sometimes, the results may be inconclusive or not match the clinical and radiological findings. This might mean more tests or samples are needed.
When Additional Sampling May Be Needed
More samples might be needed if the first results are unclear or don’t match the expected findings. We look at several factors to decide this.
These include the patient’s symptoms, the appearance of the lesion on scans, and the initial biopsy results.
Advanced Applications of Stereotactic Methods
Stereotactic neurosurgery has made big strides, bringing new hope with deep brain stimulation, radiosurgery, and thermal therapy. These methods have changed how we treat neurological issues. They offer precise and less invasive options.
Deep Brain Stimulation
Deep Brain Stimulation (DBS) is a revolutionary treatment for movement disorders like Parkinson’s disease, dystonia, and essential tremor. It involves putting electrodes in specific brain areas to control abnormal activity.
DBS greatly improves symptoms and life quality for those who don’t respond to other treatments. The process needs exact stereotactic planning to hit the right brain spots.
Stereotactic Radiosurgery
Stereotactic Radiosurgery (SRS) is a non-invasive technique that beams high doses of radiation to brain targets with great accuracy. It treats conditions like brain metastases, arteriovenous malformations, and some benign tumors.
SRS has big benefits, like low risk of complications and treating hard-to-reach brain areas.
Laser Interstitial Thermal Therapy
Laser Interstitial Thermal Therapy (LITT) is a minimally invasive ablative technique that uses laser energy to heat and kill targeted brain tissue. It’s used for treating epilepsy, brain tumors, and other lesions.
LITT uses real-time MRI thermometry to watch the ablation process. This ensures precise control over the heat damage.
Conclusion: The Evolving Role of Stereotactic Methods in Neurosurgery
Neurosurgery is making big strides, and the future of stereotactic neurosurgery is bright. Stereotactic methods are changing how we find and fix complex brain problems.
New technology and techniques are making these procedures more accurate and less invasive. Now, treatments are more focused on each patient’s needs.
These advances are not just helping patients get better faster. They’re also opening up new possibilities for treating more conditions. As we keep pushing forward, we’ll see even more improvements in how we care for patients everywhere.
FAQ
What is a stereotactic brain biopsy?
A stereotactic brain biopsy is a minimally invasive surgery. It uses a three-dimensional system to target specific brain areas. This is often to diagnose brain lesions or tumors.
How is a stereotactic brain biopsy performed?
First, a frame is attached to the patient’s head. Then, MRI or CT scans are used to find the target area. The surgeon plans the needle’s path using computer software.
The needle is inserted through a small skull hole to collect tissue samples.
What are the advantages of stereotactic brain biopsy over traditional open biopsies?
Stereotactic biopsies are less invasive. They have smaller incisions and less tissue damage. This reduces the risk of complications.They also allow for precise targeting, lowering the chance of sampling errors.
What are the possible risks and complications of stereotactic brain biopsy?
Risks include bleeding, infection, and neurological issues. There’s also a risk of reaction to anesthesia. But, the procedure is generally safe when done by skilled neurosurgeons.
How long does it take to recover from a stereotactic brain biopsy?
Recovery time varies. Most people can get back to normal in a few days to a week. Some might feel tired or uncomfortable for longer.
What is the accuracy of stereotactic brain biopsy?
This procedure is very accurate. Studies show a diagnostic yield of 90% to over 95%. Accuracy depends on the system’s precision, imaging quality, and the neurosurgeon’s skill.
Can stereotactic methods be used for therapeutic interventions?
Yes, they are used for treatments too. This includes tumor treatments, deep brain stimulation, and more.
What is the difference between frame-based and frameless stereotactic techniques?
Frame-based methods use a rigid frame on the head. Frameless systems use imaging and navigation without a fixed frame. The choice depends on the procedure and patient needs.
How are biopsy results interpreted?
A pathologist examines the tissue samples. They provide a diagnosis, including the type of lesion and its grade. This guides further treatment.
When is additional sampling needed after a stereotactic brain biopsy?
More sampling might be needed if the first results are unclear. Or if there’s a mismatch between biopsy and imaging findings. It’s also needed for suspected heterogeneous lesions.
References
National Center for Biotechnology Information. Stereotactic brain biopsy neurosurgical applications and impact. Retrieved from https://pubmed.ncbi.nlm.nih.gov/35063671/





