Last Updated on December 1, 2025 by Bilal Hasdemir
Nearly 1 in 8 women will get breast cancer in their life. Stereotactic biopsies help find it early. Is a stereotactic biopsy considered major surgery? We reveal the surprising answer. Get the essential facts.
A stereotactic biopsy is a minimally invasive way to check breast issues. But, there’s a big debate about if it’s surgery.
This article will dive into what makes a stereotactic biopsy special. We’ll look at if it’s seen as a diagnostic procedure or surgery.
Key Takeaways
- A stereotactic biopsy is a precise diagnostic tool.
- It’s considered a minimally invasive procedure.
- The classification of a stereotactic biopsy as surgery varies.
- Understanding its nature is key for patient education.
- The procedure is vital for finding breast cancer.
What Defines a Stereotactic Biopsy

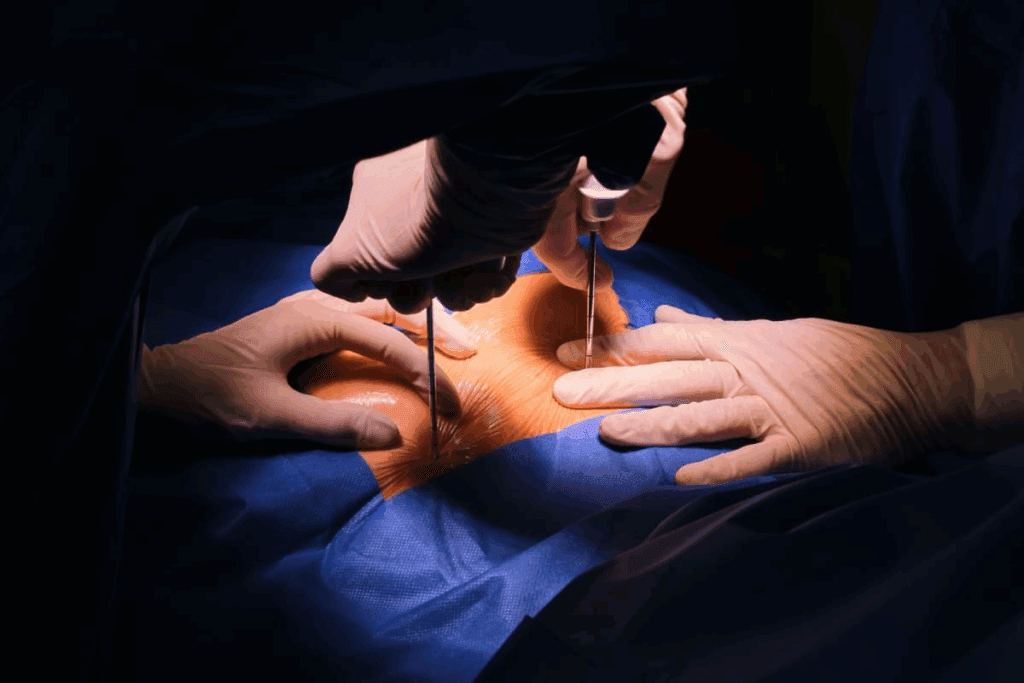
A stereotactic biopsy is a minimally invasive procedure. It uses imaging guidance to get tissue samples accurately. This method has changed medicine by allowing for precise tissue sampling from specific body locations.
Core Principles and Technology
Stereotactic biopsies use three-dimensional localization technology. This technology targets specific areas with the help of advanced imaging like mammography, MRI, or CT scans. It ensures the sample is taken from the right spot for a correct diagnosis.
The technology behind it includes advanced computer systems. These systems use imaging data to guide the biopsy needle. This precision is key for the procedure’s success, even with small or hard-to-reach lesions.
Historical Development of the Procedure
The idea of stereotactic biopsies has grown a lot over time. It started for neurosurgery but now includes the breast. The technology’s history is filled with improvements in imaging and computer navigation. These advancements have made the procedure more accurate and reliable.
As technology keeps improving, we’ll see better core needle designs and sampling methods. This could make stereotactic biopsies even more useful in medicine.
Stereotactic Biopsy vs. Traditional Surgery: Key Differences

The difference between stereotactic biopsy and traditional surgery is big. It’s about how invasive they are and how fast you can get better. Stereotactic biopsy is minimally invasive. It uses advanced imaging to guide it with great precision.
Invasiveness Comparison
One main difference is how invasive they are. Traditional surgery needs big cuts and hurts more tissue. Stereotactic biopsy, on the other hand, uses small, precise incisions or sometimes just needles. This means less damage to the tissue.
Anesthesia Requirements
Another big difference is the anesthesia used. Traditional surgeries often need general anesthesia. This is riskier and takes longer to recover from. Stereotactic biopsies, though, use local anesthesia. This is safer and lets you get better faster.
Recovery Time Distinctions
Recovery time is also a big difference. Traditional surgery means longer hospital stays and recovery times. But, stereotactic biopsies are usually done as an outpatient. Most people can go back to normal in just a day or two.
Knowing these differences helps patients and doctors choose the best option. It depends on what you need and your situation.
The Classification Debate: Surgical vs. Interventional Procedure
The debate on whether stereotactic biopsies are surgical or interventional procedures is big in the medical world. This debate is key because it changes how these procedures are seen, coded, and paid for.
Medical Classification Criteria
To figure out if a stereotactic biopsy is surgical or interventional, doctors look at a few things. They check how invasive it is, if anesthesia is used, and where it’s done. Minimally invasive procedures use small cuts or needles, causing less harm and helping patients heal faster.
As a diagnostic procedure, stereotactic biopsies give vital info for diagnosis and treatment plans. They use needle biopsy methods, which are less invasive than old-school surgical biopsies.
Why It’s Considered Minimally Invasive
Stereotactic biopsies are seen as minimally invasive because they use precise methods and small needles or probes. This method causes less damage to tissues and lowers the chance of problems. Imaging like mammograms or MRIs helps target the biopsy spot accurately, making the procedure even less invasive.
Regulatory and Coding Perspectives
From a regulatory and coding view, how we classify stereotactic biopsies affects billing and payment. Outpatient procedures, like many stereotactic biopsies, have specific coding rules. These rules are different from those for inpatient surgeries.
| Procedure Type | Coding Classification | Typical Setting |
| Stereotactic Biopsy | Interventional Radiology | Outpatient |
| Traditional Surgery | Surgical | Inpatient/Outpatient |
| Needle Biopsy | Diagnostic | Outpatient |
Knowing these classifications is vital for healthcare providers. It helps them deal with the complex world of medical billing and insurance.
The Technology Behind Stereotactic Biopsies
Stereotactic biopsies use advanced technology for precise tissue sampling. This is key for accurate diagnosis, even in hard-to-reach areas.
Three-Dimensional Localization Explained
Three-dimensional localization is key in stereotactic biopsies. It uses advanced imaging to find the target tissue’s exact location. This is done by combining data from mammography, MRI, or CT scans.
This 3D model helps doctors plan the best biopsy path. Accurate localization reduces the chance of sampling errors. This is vital when the abnormality is small or in a sensitive area.
Imaging Guidance Systems
Imaging guidance systems are essential in stereotactic biopsies. They let doctors see the biopsy needle in real-time as it moves towards the target tissue. These systems use digital mammography or CT fluoroscopy for guidance.
Real-time imaging feedback lets doctors adjust the needle’s path as needed. This ensures accurate placement and lowers the risk of complications. This is very important in delicate procedures, like brain biopsies.
Computer Navigation Technology
Computer navigation technology boosts the precision of stereotactic biopsies. It combines imaging data with advanced software to create a detailed 3D model of the biopsy site. This helps doctors plan and perform the biopsy with great accuracy.
Computer navigation also helps with precise needle placement. This reduces the risk of tissue damage or other issues. The technology is very useful in complex cases, where the target tissue is hard to reach.
Types of Stereotactic Biopsy Procedures
Medical technology has improved a lot. Now, stereotactic biopsies are more precise. They are tailored for different parts of the body.
Stereotactic Breast Biopsies
Stereotactic breast biopsies use mammography guided images. They help find and sample breast tissue. This is great for checking out spots that are hard to feel or see.
- Uses mammographic images to guide the biopsy needle
- Good for checking lesions found during mammograms
- Reduces the need for open surgery
Stereotactic Brain Biopsies
Stereotactic brain biopsies take precise samples of brain tissue. They use three-dimensional localization to do this. This is key for finding and diagnosing brain tumors.
- Frame-based or frameless stereotaxy is used for precise localization
- Helps diagnose brain lesions with less harm
- Makes it easier to plan treatments
Other Applications of Stereotactic Techniques
Stereotactic techniques are used in many areas, not just breast and brain. They help sample lesions in different parts of the body.
Stereotactic biopsy procedures are very important today. They offer accurate, minimally invasive ways to diagnose. This is great for patients.
The Outpatient Nature of Stereotactic Procedures
Medical technology has made big strides, leading to more stereotactic biopsies being done on an outpatient basis. This change is great for patients. It shows how these procedures are less invasive and how modern medicine works efficiently.
Benefits of Same-Day Procedures
Outpatient stereotactic biopsies have many perks. They mean less time recovering at home, lower chances of getting sick in the hospital, and the comfort of being in a place you know. Often, patients can get back to their daily lives quickly, sometimes even the same day.
Key benefits of same-day stereotactic biopsy procedures include:
- Minimally invasive with less tissue damage
- Local anesthesia used, reducing risks associated with general anesthesia
- Shorter recovery times compared to traditional surgical biopsies
- Cost-effective, reducing the need for hospital stays
Facility Requirements
Places where outpatient stereotactic biopsies happen have the latest imaging tech, like mammography or MRI machines. They’re staffed by skilled radiologists and technicians. These spots must follow strict safety and quality rules to keep patients safe and get accurate results.
Comparison to Hospital-Based Surgeries
Outpatient stereotactic biopsies are a big difference from surgeries done in hospitals. Hospital surgeries need general anesthesia and keep you there longer. But, stereotactic biopsies use local anesthesia, leading to quicker healing and lower costs.
| Procedure Characteristics | Stereotactic Biopsy | Hospital-Based Surgery |
| Anesthesia Type | Local | General |
| Recovery Time | Short, often same day | Longer, may require hospital stay |
| Cost | Generally lower | Higher due to hospital stay and general anesthesia |
The Complete Stereotactic Biopsy Process
The stereotactic biopsy process includes getting ready, doing the biopsy, and taking care of yourself after. It’s a minimally invasive way to get accurate results. This is thanks to advanced technology.
Pre-Procedure Preparation
Before a stereotactic biopsy, you’ll go through some steps. You might have imaging tests to find the exact spot. You’ll also learn about diet and meds.
Choosing between core needle or vacuum-assisted devices depends on the biopsy type and where it is.
It’s key to follow the prep steps well. This helps make the biopsy a success. Arrive on time, bring someone, and ask questions.
During the Procedure: What to Expect
During the biopsy, you’ll be positioned for easy access. It’s done under local anesthesia to keep you comfortable. The core needle or vacuum-assisted device will take tissue samples.
Advanced imaging, like mammography or MRI, helps find the right spot. This makes sure the samples are from the right area. It boosts biopsy accuracy.
Post-Procedure Care and Monitoring
Right after, you’ll be watched for any immediate issues. Some soreness or bruising is normal but usually goes away. You’ll get tips on caring for the site and what to expect while you recover.
The samples go to a lab for analysis. The results will guide what happens next, like more tests, treatment, or watching and waiting.
Knowing the whole biopsy process helps you prepare better. It reduces anxiety and makes the experience smoother.
Medical Professionals Who Perform Stereotactic Biopsies
Stereotactic biopsies need a team with different skills and knowledge. This method is not very invasive but requires great precision and understanding of the patient’s health.
The Role of Radiologists
Radiologists are key in doing stereotactic biopsies. They use imaging like mammography, MRI, and CT scans to find the exact spot for the biopsy. Radiologists are often the main doctors doing these procedures, like for breast or brain biopsies.
Thanks to advanced imaging, radiologists can guide the needle to the right spot. This reduces risks and makes sure the sample is from the right area.
When Surgeons Are Involved
While radiologists lead in stereotactic biopsies, surgeons might join in some cases. If the biopsy shows a need for surgery, surgeons will help plan the treatment with the patient and other doctors.
In some cases, surgeons might do the biopsy too, if the spot is tricky or if surgery might follow right after.
The Multidisciplinary Team Approach
The success of stereotactic biopsies depends on a multidisciplinary team. This team includes radiologists, surgeons, pathologists, nurses, and more. They work together to take care of the patient from start to finish.
| Medical Professional | Role in Stereotactic Biopsy |
| Radiologist | Performs the biopsy, interprets imaging |
| Surgeon | Provides surgical intervention when necessary |
| Pathologist | Analyzes biopsy samples for diagnosis |
Having different specialties work together makes stereotactic biopsies more accurate and safe. This leads to better results for patients.
Frame-Based vs. Frameless Stereotaxy Techniques
Stereotactic biopsies have evolved into two main types: frame-based and frameless. Each has its own benefits and uses. The choice depends on the patient’s situation, their health, and the doctor’s preference.
Traditional Frame-Based Guidance
Frame-based stereotaxy is the traditional method. It uses a rigid frame attached to the patient’s head or body. This frame helps guide the biopsy needle with great precision.
Advantages of Frame-Based Guidance:
- High accuracy due to the rigid frame’s stability
- Well-established technique with a long history of use
- Effective for complex or deep-seated lesions
But, this method can be uncomfortable for patients because of the rigid frame.
Modern Frameless Techniques
Frameless stereotaxy is a newer method. It uses advanced imaging and computer navigation without a rigid frame. This approach tracks the biopsy needle’s position in real-time.
Key Benefits of Frameless Stereotaxy:
- Greater flexibility and comfort for the patient
- Less invasive, potentially reducing recovery time
- Allows for more complex trajectories and approaches
A study found that frameless stereotactic biopsy systems are as accurate as traditional methods. They also offer more comfort and flexibility for patients.
“Frameless stereotactic biopsy systems offer a viable alternative to traditional frame-based methods, enriching patient comfort without sacrificing precision.”
Clinical Considerations for Each Approach
Choosing between frame-based and frameless stereotaxy depends on several factors. These include the type of lesion, the patient’s health, and the biopsy’s goals. Computer navigation is key in frameless techniques, allowing for precise targeting and monitoring.
Factors Influencing the Choice of Technique:
- The location and characteristics of the target lesion
- The patient’s medical history and current condition
- The experience and preference of the medical team
In conclusion, both frame-based and frameless stereotaxy have their roles in medicine. Knowing their strengths and weaknesses is vital for the best patient care.
Biopsy Tools and Sampling Methods
Biopsy tools have changed a lot, making stereotactic procedures more precise. The success of these biopsies depends on the technology and methods for sampling tissue.
Core Needle and Vacuum-Assisted Devices
Core needle biopsy devices are key in stereotactic biopsies. They can get bigger tissue samples. They’re great for small or hard-to-reach areas.
Vacuum-assisted biopsy devices use suction to get tissue samples. They often get more tissue for analysis.
“The use of vacuum-assisted devices has changed the biopsy field,” says a top expert. “It helps get more accurate diagnoses.” This shows how important the right tool is for each biopsy.
Tissue Sampling Techniques
The method for sampling tissue greatly affects the diagnosis. Stereotactic biopsies use different methods to get a good sample. They use imaging to find the exact spot.
- Imaging guidance for precise localization
- Multiple sampling to ensure representativeness
- Minimally invasive techniques to reduce patient discomfort
Advances in Biopsy Technology
New biopsy technology aims to make core needle and vacuum-assisted devices better. It includes better imaging and more precise needle systems. This makes the diagnostic process better.
As biopsy tech keeps getting better, so will the accuracy of stereotactic biopsies. This will help patients get better treatment plans faster.
From Biopsy to Diagnosis: The Pathology Process
The pathology process after a stereotactic biopsy is very detailed. It looks at the tissue samples to give a diagnosis. This step is key to figuring out what’s wrong.
How Samples Are Processed
After the biopsy, the tissue goes to the pathology lab. There, it goes through several steps:
- Fixation: The samples are fixed in a solution to keep the tissue intact.
- Embedding: The fixed samples are embedded in paraffin wax to keep their shape.
- Sectioning: Thin slices of the tissue are cut using a microtome.
- Staining: The slices are stained with dyes to show cell details.
- Examination: A pathologist looks at the stained slices under a microscope.
Getting the sample right is very important for the pathology process. A pathology expert said, “The quality of the biopsy sample directly impacts the accuracy of the diagnosis.”
“The diagnostic accuracy of a biopsy is heavily reliant on the quality of the sample obtained,” said Medical Expert, a renowned pathologist.
Timeframe for Results
How long it takes to get the results depends on the case and the lab’s work. Usually, it’s a few days to a week.
| Procedure | Typical Turnaround Time |
| Simple Biopsy | 2-3 days |
| Complex Biopsy | 5-7 days |
Understanding Pathology Reports
Pathology reports give detailed info about the tissue, including the diagnosis. They include:
- Clinical history and biopsy details
- Macroscopic and microscopic findings
- Diagnosis or conclusion
It’s important for patients and doctors to understand these reports. They help make treatment decisions.
Accuracy and Reliability of Stereotactic Biopsies
Stereotactic biopsy procedures are very accurate in diagnosing medical conditions. This is thanks to advanced imaging technologies that guide the sampling process.
Diagnostic Accuracy Rates
Research shows that stereotactic biopsies are over 95% accurate. This high accuracy is key for planning effective treatments.
The precision of these biopsies comes from three-dimensional imaging. It helps pinpoint the exact area to take the tissue sample from.
| Biopsy Type | Accuracy Rate | Common Applications |
| Stereotactic Breast Biopsy | 95-98% | Diagnosing breast lesions |
| Stereotactic Brain Biopsy | 90-95% | Diagnosing brain tumors and lesions |
Factors Affecting Biopsy Success
Several factors can impact the success of a stereotactic biopsy. These include the practitioner’s skill, the imaging equipment’s quality, and the lesion’s characteristics.
Key factors that can affect biopsy success include:
- The size and location of the lesion
- The type of imaging guidance used
- The experience of the radiologist or surgeon performing the biopsy
When Additional Sampling May Be Needed
Sometimes, more tissue sampling is needed if the first sample is unclear or the diagnosis is uncertain. This might mean repeating the biopsy or trying a different method.
Deciding on additional samples depends on the clinical situation and the first biopsy’s results. Effective communication among the radiologist, pathologist, and healthcare team is vital in these cases.
Potential Risks and Complications
Stereotactic biopsies, like any surgical intervention, have their own risks. The procedure is safe and minimally invasive. But knowing the possible risks is key for making informed choices.
Common Minor Complications
Most people who get a stereotactic biopsy face little side effects. Some minor issues include:
- Temporary bruising or swelling at the biopsy site
- Mild discomfort or pain, which can be managed with over-the-counter pain relievers
- Minor bleeding, which usually stops on its own
Local anesthesia is used to reduce discomfort during the procedure. This greatly lowers the risk of complications from general anesthesia.
Rare Serious Complications
Though rare, serious complications can happen with stereotactic biopsies. These include:
- Infection at the biopsy site, which might need antibiotic treatment
- Significant bleeding or hematoma formation
- Nerve damage, leading to numbness or tingling
The risk of serious complications with needle biopsy procedures is low. But it’s important to know about these risks.
Risk Factors and Prevention
Some factors can raise the risk of complications during or after a stereotactic biopsy. These include:
| Risk Factor | Prevention Strategy |
| Bleeding disorders | Careful patient screening and management of anticoagulant medications |
| Previous allergic reactions to anesthesia | Thorough medical history and selection of appropriate anesthesia |
| Poor overall health | Pre-procedure assessment and optimization of health status |
By knowing these risk factors and using prevention strategies, we can lower the chance of complications.
Insurance Coverage and Cost Considerations
Insurance and cost are key when deciding on stereotactic biopsies. As an outpatient procedure, they are often cheaper than traditional surgeries. These surgeries need hospital stays.
The costs of stereotactic biopsies include coding, insurance, and what you might pay yourself.
Typical Coding and Classification
Getting the coding right is important for insurance and tracking costs. Stereotactic biopsies are seen as a diagnostic procedure. The exact code depends on the biopsy type and where it’s done.
- The Current Procedural Terminology (CPT) codes describe the procedure.
- ICD-10 codes classify the diagnosis or condition being looked at.
- Healthcare Common Procedure Coding System (HCPCS) codes might also apply.
Insurance Coverage Patterns
Insurance for stereotactic biopsies varies by provider and policy. Most plans cover them as a medically necessary procedure by a qualified doctor.
Several factors affect coverage:
- The type of insurance (e.g., Medicare, Medicaid, private).
- The policy’s terms and conditions.
- The procedure’s medical necessity as decided by the doctor.
Out-of-Pocket Expenses
Even with insurance, patients might face extra costs for stereotactic biopsies. These can include:
- Deductibles and copays.
- Coinsurance payments.
- Any extra services or tests needed for the procedure.
Knowing these costs and talking to your doctor can help you financially prepare for the procedure.
Conclusion: Understanding the Surgical Status of Stereotactic Biopsies
Stereotactic biopsies are a big step forward in medical diagnosis. They offer a minimally invasive way to get tissue samples, unlike old-school surgeries. We’ve looked into how these biopsies work and their place in medicine.
These biopsies are different from traditional surgeries because they’re less invasive. They’re often done on an outpatient basis. This means you get local anesthesia and don’t need to stay in the hospital long.
Whether a stereotactic biopsy is seen as a surgery or not can vary. It depends on who’s doing it and the rules they follow. But one thing is clear: they help doctors get the right tissue samples for tests.
In short, knowing about stereotactic biopsy procedures is key for both patients and doctors. It helps everyone understand the benefits and what to expect. This way, people can make better choices about their health care.
FAQ
What is a stereotactic biopsy?
A stereotactic biopsy is a non-invasive test. It uses images and precise location to take tissue samples. This is often done in places like the breast or brain.
Is a stereotactic biopsy considered a surgical procedure?
There’s debate on whether it’s a surgery. It involves taking tissue samples but is seen as less invasive than traditional surgery.
What are the benefits of stereotactic biopsy over traditional surgery?
It’s less invasive and uses local anesthesia. Recovery time is shorter. It’s usually done as an outpatient procedure.
How does stereotactic biopsy use imaging guidance?
It uses imaging like mammography to locate the target. This helps place the needle accurately for sampling.
What is the role of radiologists in performing stereotactic biopsies?
Radiologists are key. They interpret images, guide the needle, and ensure the tissue is sampled correctly.
What are the possible risks and complications of stereotactic biopsy?
It’s generally safe but can cause minor issues like bleeding. Serious problems like infection or nerve damage are rare. Preventing risks is important.
How is the accuracy of stereotactic biopsy ensured?
Accuracy comes from imaging guidance and three-dimensional localization. Computer navigation also plays a role. This ensures reliable results.
What happens after a stereotactic biopsy?
The tissue sample is sent for examination. Results take time. The report will guide further treatment if needed.
Are stereotactic biopsies covered by insurance?
Coverage varies by provider and procedure. Following coding guidelines is key for reimbursement.
What is the difference between frame-based and frameless stereotaxy techniques?
Frame-based uses a rigid frame for guidance. Frameless uses computer navigation and imaging. Both have their benefits and considerations.
References
National Center for Biotechnology Information. Stereotactic Breast Biopsy Procedure or Surgery?. Retrieved from https://pubmed.ncbi.nlm.nih.gov/17981115/