Last Updated on December 1, 2025 by Bilal Hasdemir
Did you know advanced imaging has changed medical treatments? It now allows for precise interventions that were once impossible. Stereotactic MRI combines stereotaxis with MRI to accurately locate and target body areas.
Medical treatments are changing with MRI guidance. This makes procedures more precise. Stereotactic MRI is key for neurosurgery and radiation therapy, where exact location is critical.
In this article, we’ll dive into stereotactic imaging. We’ll look at its basics, technical sides, and how it’s used in medicine today.
Key Takeaways
- Understanding the basics of stereotactic MRI and its role in medical treatments.
- The significance of 3D localization in precise medical interventions.
- Exploring the applications of stereotactic MRI in neurosurgery and radiation therapy.
- The technical aspects that make stereotactic MRI a valuable tool in modern medicine.
- The future prospects of stereotactic imaging in advancing healthcare.
The Fundamentals of Stereotactic MRI
Stereotactic MRI has changed neurosurgery and imaging. It mixes the exactness of stereotactic methods with MRI’s detailed images. This helps in accurate diagnosis and planning treatments.
Definition and Basic Principles
Stereotactic MRI uses MRI with stereotactic methods for precise body targeting. It uses a coordinate system to pinpoint locations in the brain or body. MRI images and stereotactic frames or markers help in precise targeting.
First, MRI images are taken. Then, a detailed map of the area is made. This map, with a coordinate system, allows for precise targeting. The accuracy of stereotactic MRI depends on MRI image quality and stereotactic equipment precision.
Historical Development of Stereotactic Imaging
Stereotaxis has grown a lot over time. It started in neurosurgery and has improved with new imaging tech. The use of MRI in stereotactic practice was a big step, improving soft tissue contrast and spatial resolution.
Year | Milestone | Significance |
1908 | Introduction of Stereotactic Frame | Enabled precise localization in neurosurgery |
1980s | Incorporation of CT into Stereotactic Procedures | Improved imaging capabilities |
1990s | Introduction of MRI in Stereotactic Procedures | Enhanced soft tissue contrast and spatial resolution |
The history of stereotactic imaging shows ongoing innovation, with MRI being key.
How Stereotactic MRI Differs from Conventional MRI
Stereotactic MRI stands out because it offers higher resolution and precision. It’s designed to give accurate spatial information. This is key for neurosurgical procedures and other precise tasks.
Technical Distinctions and Capabilities
Stereotactic MRI has several key differences from conventional MRI. Firstly, it uses stereotactic frames or fiducial markers for precise targeting in the brain. This is vital in neurosurgery for finding tumors or other areas of interest. It also uses advanced imaging sequences and techniques to improve image quality.
“The integration of stereotactic principles into MRI technology has revolutionized the field of neurosurgery, enabling more precise and effective treatments.” This quote shows how much stereotactic MRI has changed clinical practice.
Resolution and Precision Advantages
Stereotactic MRI’s main advantage is its ability to provide high-resolution images. This is thanks to advanced coil designs, imaging sequences, and algorithms. It gives a detailed and accurate view of the brain’s anatomy. This is essential for complex neurosurgical procedures.
- Enhanced image resolution for better tissue differentiation
- Precise spatial information for accurate targeting
- Advanced imaging sequences for improved contrast and detail
By combining these technical advancements, stereotactic MRI is a powerful tool for neurosurgical planning. It leads to better patient outcomes.
The Science Behind 3D Localization in MRI
Exploring the science of 3D localization in MRI shows its power in medical imaging. We use advanced tech for precise localization. This is key for accurate diagnoses.
Coordinate Mapping Systems
Coordinate mapping systems are key for 3D localization in MRI. They help us map the body’s inside with high precision. This uses a three-dimensional coordinate system.
We assign coordinates to body landmarks as reference points. This creates a detailed map of the area we’re interested in. Such mapping is vital for precise procedures like neurosurgery or finding tumors.
Coordinate System | Description | Application |
Cartesian | Uses x, y, z coordinates | General MRI localization |
Polar | Uses radius and angles | Specific anatomical regions |
Cylindrical | Combines Cartesian and polar coordinates | Complex anatomical structures |
Spatial Registration Techniques
Spatial registration techniques are vital for 3D localization in MRI. They ensure MRI images match the patient’s anatomy. This is essential for both diagnosis and treatment planning.
We employ various registration algorithms for this alignment. These can be rigid or non-rigid, based on anatomical changes. For example, rigid registration works when structures are not deformed much. Non-rigid registration is used for significant changes, like tumors or after surgery.
Key benefits of accurate spatial registration include better diagnosis and treatment outcomes. By aligning MRI images with the patient’s anatomy, we can plan and execute treatments more effectively.
Stereotactic Frame Systems in MRI
Stereotactic frame systems are key in MRI-guided neurosurgery. They ensure precision and accuracy. These systems keep the head steady and help target specific brain areas.
Types of Stereotactic Frames
There are many types of stereotactic frames for MRI. Traditional frames are metal and attach to the skull with pins or screws. They offer high accuracy and are used for precise procedures.
Adjustable frames are more flexible, allowing for changes during surgery. This is useful in complex cases where flexibility is important.
Some frames are made for MRI use, using materials that don’t affect the magnetic fields. These MRI-compatible frames ensure the imaging process goes smoothly.
Frame-Based vs. Frameless Navigation
The choice between frame-based and frameless systems depends on the procedure’s needs and the team’s preference. Frame-based systems are very accurate and used for precise targeting.
Frameless navigation systems are more flexible and used in various procedures. They use advanced imaging and tracking for real-time guidance.
Frame-based systems are more accurate but frameless systems are gaining popularity. They offer versatility and don’t need rigid fixation. The choice depends on the patient’s needs and the team’s preference.
Fiducial Markers and Their Role in Stereotactic MRI
Fiducial markers are key in stereotactic MRI. They help with accurate registration and targeting. These markers are vital for precise procedures, allowing for accurate brain navigation.
Types of Fiducial Markers
There are different types of fiducial markers for stereotactic MRI. Skin fiducial markers are on the skin and used for initial registration. Bone fiducial markers are implanted in the bone for a stable reference. Implantable fiducial markers are in the tissue for high-precision procedures.
The right marker depends on the procedure’s needs. This includes the accuracy needed and the location in the body.
Marker Placement and Registration
Putting fiducial markers in the right place is essential for success in stereotactic MRI. Marker placement means putting them where they’re seen in MRI images. Registration aligns these markers with MRI images for a precise coordinate system.
Good registration means the stereotactic coordinates match the MRI images. This makes precise targeting and navigation possible during the procedure.
Image Guidance and Trajectory Planning
Advanced software systems are key in guiding images and planning paths for MRI in neurosurgery. They give neurosurgeons the tools they need for precise and safe operations.
Software Systems for Stereotactic Planning
Software for planning stereotactic procedures is very advanced. It has many features that make MRI-guided surgeries more accurate. Some important features include:
- 3D Visualization: It lets surgeons see the target area in three dimensions. This helps them understand the anatomy better.
- Multiplanar Reconstruction: Surgeons can see the anatomy in different planes. This makes planning more accurate.
- Registration and Fusion: The software can combine images from different sources. This gives a clearer view of the target area.
These systems are vital for planning complex neurosurgical procedures. They help surgeons plan their approach before surgery.
Trajectory Optimization Techniques
Optimizing the path for MRI surgery is very important. It makes sure the surgery is safe and effective. Techniques for optimizing the path include:
- Risk Assessment: Software can check the risks of different paths. This helps surgeons choose the safest one.
- Entry Point Selection: The software helps find the best starting point for the surgical tool. This reduces damage to nearby tissue.
- Real-Time Adjustments: Some systems let surgeons make changes during the surgery. This helps them adapt to any surprises.
Using these techniques, neurosurgeons can greatly improve MRI surgery outcomes. This makes the surgery safer and more effective.
Applications of Stereotactic MRI in Neurosurgery
Stereotactic MRI has changed neurosurgery by giving precise images for surgeries. It helps neurosurgeons do complex operations more accurately and safely.
Brain Tumor Resection
In brain tumor surgery, stereotactic MRI is key. It helps find the tumor’s exact spot and size. This info lets surgeons plan the best way to remove it, keeping healthy tissue safe.
Studies show using stereotactic MRI in brain tumor surgery leads to better results. It means more tumors are fully removed.
Clinical Evidence: A study in the Journal of Neurosurgery found that MRI-guided tumor removal cut down on post-op problems.
Deep Brain Stimulation
Deep brain stimulation (DBS) treats movement disorders like Parkinson’s. Stereotactic MRI is vital for placing DBS electrodes precisely. It shows the brain’s details, helping surgeons aim for the right spots.
Precision is key in DBS. Small mistakes in electrode placement can affect treatment success. Stereotactic MRI makes sure electrodes are in the right place, improving treatment results.
Epilepsy Surgery
In epilepsy surgery, stereotactic MRI finds the seizure source and maps the brain. This info is key for removing the seizure area without harming other brain parts.
Using stereotactic MRI in epilepsy surgery has shown better results. A study in Epilepsia found MRI-guided surgery led to more people being seizure-free than other methods.
Stereotactic Radiosurgery and MRI Integration
Stereotactic radiosurgery, when paired with MRI, brings unmatched precision to treating brain disorders. This combo has greatly improved neurosurgery, giving patients better treatment options.
Gamma Knife Procedures
Gamma Knife radiosurgery is a top-notch radiation therapy. It uses MRI integration to target specific brain areas with precision. It’s great for treating brain tumors, vascular malformations, and some neurological issues.
With MRI, Gamma Knife procedures get a clear view of the target area. This lets doctors plan and execute treatment with great accuracy. MRI data helps create a detailed plan, ensuring the right dose goes to the target and sparing healthy tissue.
Linear Accelerator-Based Treatments
Linear accelerator (LINAC)-based stereotactic radiosurgery also benefits from MRI integration. LINAC systems send radiation beams from different angles to hit the target. MRI’s high-resolution images are key in defining the target and planning the treatment.
Combining LINAC radiosurgery with MRI leads to high precision in treatment. This method is ideal for treating bigger or irregular tumors that Gamma Knife can’t handle.
MRI integration with stereotactic radiosurgery marks a big leap in treating neurological conditions. It boosts the precision and success of these treatments, leading to better patient results.
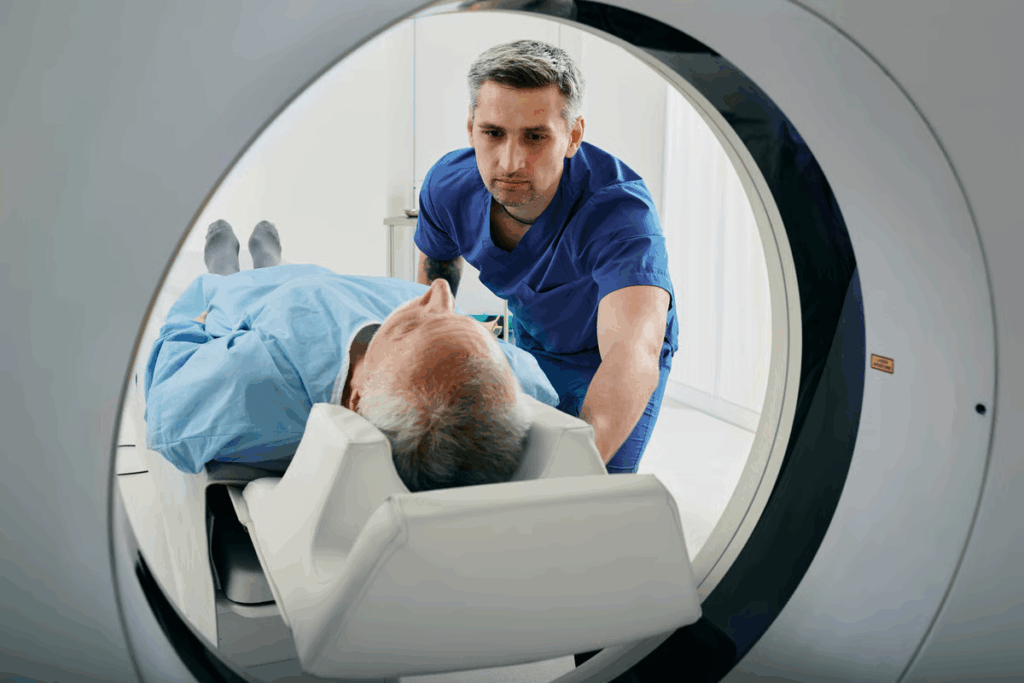
Intraoperative MRI and Real-Time Navigation
Real-time navigation through intraoperative MRI is changing surgery. It lets surgeons see the surgical area live. They can make changes to keep the surgery precise and safe.
Mobile MRI Systems
Mobile MRI systems are key in intraoperative MRI. They let imaging happen right in the operating room. This means no need to move patients to a different MRI room.
Real-Time Image Updates During Surgery
Intraoperative MRI also gives real-time image updates. This lets surgeons check the surgery’s progress and adjust as needed.
Adding real-time images to navigation systems makes surgeries more accurate. This is very important in surgeries like brain tumor removals or deep brain stimulation.
Using intraoperative MRI and real-time navigation leads to better surgery results. It also lowers the chance of problems. As this tech gets better, we’ll see even more new uses in surgery.
Functional Mapping with Stereotactic MRI
In neurosurgery, stereotactic MRI is key for mapping brain functions. It helps keep important brain areas safe during surgery. This is vital for preserving brain functions.
Motor and Sensory Mapping
Motor and sensory mapping are key in neurosurgery. Stereotactic MRI helps find motor and sensory areas. This is important for planning surgery.
Surgeons use it to spot areas for movement and touch. This helps them plan surgery carefully.
The table below shows how motor and sensory mapping differ in stereotactic MRI:
Mapping Technique | Description | Clinical Application |
Motor Mapping | Identifies motor cortices with fMRI or electrical stimulation | Keeps motor functions safe during surgery |
Sensory Mapping | Finds sensory cortices with fMRI or evoked potentials | Protects sensory functions during surgery |
Language and Cognitive Function Mapping
Mapping language and cognitive functions is also important. Stereotactic MRI helps pinpoint language and cognitive areas. This is essential for planning and doing surgery.
This method has greatly improved surgery results. It helps avoid harming important brain parts. This leads to better outcomes for patients.
Accuracy and Precision in Stereotactic MRI
Getting high accuracy in stereotactic MRI is key for successful brain surgeries. The precision of these MRI systems is what makes complex surgeries work.
Factors Affecting Navigation Accuracy
Many things can change how accurate a stereotactic MRI system is. Technical considerations like the MRI machine’s quality, the type of frame used, and the navigation software matter a lot.
Also, how different each patient’s brain is can affect the system’s accuracy. Brain changes during surgery can make it harder to get precise.
Error Measurement and Correction
It’s important to measure and fix errors in stereotactic MRI navigation to keep it accurate. Using markers and updating images in real-time during surgery helps reduce mistakes.
The table below shows some common ways to fix errors in stereotactic MRI.
Error Correction Technique | Description | Application |
Fiducial Marker Registration | Using markers to align the patient’s anatomy with the MRI images | Pre-operative planning |
Real-Time Image Updates | Updating MRI images in real-time during surgery to account for brain shift | Intraoperative navigation |
Stereotactic Frame Adjustment | Adjusting the stereotactic frame to ensure precise alignment with the planned trajectory | Intraoperative adjustment |
By knowing what affects accuracy and using good error correction, we can make stereotactic MRI systems more precise.
Patient Experience and Clinical Outcomes
The success of stereotactic MRI procedures depends a lot on how well patients are prepared and feel. This affects the results of the treatment. As we move forward in neurosurgery, making sure patients have a good experience is key to the best results.
Patient Preparation and Comfort
Starting with comfort, we need to prepare patients well. This means telling them about the procedure and why they need to stay very quiet. Good preparation helps lower anxiety and makes patients happier with their treatment.
During the procedure, we use things like padding to make them comfortable. Sometimes, we give them a little sedation to help them relax. “By focusing on patient comfort, we can significantly improve the accuracy and success of stereotactic MRI procedures,” say top neurosurgeons.
Outcome Measures and Success Rates
We check how well stereotactic MRI works by looking at several things. These include how precise the procedure is, how quickly patients recover, and if the treatment works well. Success rates are usually very high for these MRI-guided procedures, which are great for treating brain tumors and other neurosurgical issues.
Research shows that stereotactic MRI leads to better results because it gives very clear images and is very precise. For example, a study found that using MRI for brain tumor surgeries led to more tumors being completely removed. This helped patients live longer.
To keep improving, we need to keep working on our techniques and focus more on the patient. This means always checking how well the treatment is working and listening to what patients say. This helps us give better care.
Cost-Effectiveness and Healthcare Implementation
The cost-effectiveness of stereotactic MRI is complex. It involves equipment costs, operational expenses, and how insurance pays for it. As more healthcare systems use this technology, knowing its economic impact is key for successful use.
Equipment and Operational Costs
Buying stereotactic MRI equipment is expensive. This includes the cost of MRI machines, frames or systems, and software. Running the equipment also has costs, like maintenance, training staff, and supplies.
Reimbursement and Access Challenges
How insurance pays for stereotactic MRI affects its cost-effectiveness. Different healthcare systems and insurance plans have different rates. Getting enough money from insurance is important for the service to stay financially stable.
Getting access to stereotactic MRI is also a big issue. It’s more available in cities than in rural areas. Ways to improve access include using mobile MRI units and partnerships between healthcare providers.
Understanding the cost-effectiveness of stereotactic MRI helps healthcare systems use it better. By tackling the challenges of equipment costs, running expenses, and insurance, they can make this technology more efficient and fair for everyone.
Future Directions in Stereotactic MRI Technology
The future of stereotactic MRI looks bright, thanks to new tech and research. We’re pushing the limits of medical imaging. This will make stereotactic MRI even better for medical use.
Advancements in Imaging Techniques
High-field MRI and advanced coil technologies are key areas of improvement. They aim to make images clearer and more detailed. This is important for precise surgery.
Researchers are also looking into functional MRI and diffusion tensor imaging. These methods will give us more info about the brain. This will help plan surgeries better.
Research Frontiers
There are many new areas to explore in stereotactic MRI. These include:
- Using artificial intelligence and machine learning to analyze images better.
- Creating real-time imaging for better surgery guidance.
- Developing novel contrast agents to see tissues more clearly.
Research Area | Potential Impact | Current Status |
AI in Image Analysis | Enhanced diagnostic accuracy | Ongoing clinical trials |
Real-Time Imaging | Improved intraoperative guidance | Early-stage research |
Novel Contrast Agents | Better tissue characterization | Preclinical studies |
As research moves forward, stereotactic MRI will become more important. New tech and research will lead to better care for patients. This is exciting for the future of medicine.
Conclusion: The Evolving Role of Stereotactic MRI in Modern Medicine
Stereotactic MRI is a key tool in modern medicine. It helps doctors find and treat problems with great accuracy. This is true for surgeries and treatments that use radiation.
This technology has grown stronger by working with new tools. It helps doctors make better diagnoses and treatments. We’ve learned how it’s different from regular MRI scans and its uses in surgery and radiation therapy.
The role of stereotactic MRI is getting better and better. It’s leading to better care for patients. As technology keeps improving, it will keep being a big part of medicine’s future. It will help doctors give care that’s more precise and tailored to each person.
FAQ
What is stereotactic MRI and how does it differ from conventional MRI?
Stereotactic MRI combines MRI with precise targeting. It offers better detail and accuracy than regular MRI.
What are the main applications of stereotactic MRI in neurosurgery?
It’s used for brain tumor removal, deep brain stimulation, and epilepsy surgery. This improves surgery results and patient care.
How do fiducial markers contribute to the accuracy of stereotactic MRI?
Fiducial markers help match MRI images with the patient’s body. This makes precise targeting possible during procedures.
What is the difference between frame-based and frameless navigation systems in stereotactic MRI?
Frame-based systems use a fixed frame on the head. Frameless systems use markers and software for precise targeting without a frame.
How does stereotactic MRI enhance the accuracy of radiosurgery treatments?
It offers precise tumor targeting. This makes radiation therapy more accurate in treatments like Gamma Knife procedures.
What are the benefits of intraoperative MRI in neurosurgical procedures?
It allows for real-time updates during surgery. This leads to safer and more accurate procedures, improving patient results.
How does stereotactic MRI contribute to functional mapping in neurosurgery?
It maps brain functions like motor and sensory. This is key for planning and performing neurosurgery.
What factors affect the accuracy of navigation in stereotactic MRI?
Image quality, marker placement, and patient movement are important. They must be controlled for precise targeting.
What is the cost-effectiveness of stereotactic MRI compared to other medical imaging technologies?
Its cost-effectiveness depends on several factors. These include equipment costs, reimbursement, and clinical results. It’s important to evaluate these in healthcare planning.
What are the future directions in stereotactic MRI technology?
New technologies like advanced image systems and real-time imaging will improve stereotactic MRI. They will also expand its use in neurosurgery and other fields.
References
National Center for Biotechnology Information. Stereotactic MRI technology and applications in medicine. Retrieved from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4428978/