Last Updated on December 2, 2025 by Bilal Hasdemir
Every year, thousands of people worldwide get diagnosed with brain tumors or AVMs. Treatments like radiosurgery are becoming key in these cases.
Radiation therapy and stereotactic radiosurgery are often mixed up. But they have different uses. The main difference is in how they use radiation and their precision.Learn what is the difference between radiation and stereotactic radiosurgery. Understand the difference in dose and precision clearly.
Radiation therapy treats bigger areas and often needs many sessions. On the other hand, radiosurgery focuses on a small, precise area in just one session.
Key Takeaways
- Radiation therapy and radiosurgery differ in their application and precision.
- Radiosurgery is used for precise treatment of targeted areas like brain tumors or AVMs.
- Radiation therapy is often used for larger areas and may involve multiple sessions.
Understanding Radiation Therapy: Basic Principles and Applications
It’s important for patients and healthcare providers to know about radiation therapy. It’s a key treatment for many medical conditions. Radiation therapy uses high-energy particles or waves to kill or damage cancer cells. It targets a specific area of the body.

How Radiation Therapy Works
Radiation therapy damages the DNA of cancer cells, stopping them from growing. This damage is caused by ionizing radiation, like X-rays and gamma rays. These high-energy particles break the DNA strands, killing the cells.
“Radiation therapy is a critical component in the treatment of cancer,” say medical professionals. It offers a chance for cure or relief to many patients. The success of radiation therapy depends on the cancer type, stage, and treatment dose.
It can be used alone or with other treatments like surgery and chemotherapy. This makes it a versatile option in cancer care.
Types of Radiation Used in Medical Treatments
There are different types of radiation used in treatments. Photon radiation, including X-rays and gamma rays, is the most common. Electron radiation treats superficial tumors. Proton radiation is precise, targeting tumors with less damage to nearby tissues.
The choice of radiation depends on the condition, tumor location and size, and patient health. Knowing about these types helps healthcare providers create personalized treatment plans.
The Evolution of Radiation Therapy in Modern Medicine

Radiation therapy has evolved a lot in modern medicine. Stereotactic radiosurgery was created as a safer option than traditional brain surgery. Now, it’s used to treat many neurological and other conditions.
Historical Development of Radiation as a Treatment Method
Radiation therapy started in the early 20th century with X-rays for cancer treatment. Our knowledge of radiation has grown, leading to better treatments. The 1950s saw the start of cobalt therapy, which could treat tumors deeper and more effectively.
The arrival of linear accelerators improved radiation therapy. They allowed for high-energy beams with great precision. Today’s systems have even more advanced imaging and beam control.
Technological Advancements in Radiation Delivery Systems
New systems like stereotactic radiosurgery and stereotactic radiotherapy have been developed. They deliver precise, high doses to targets, protecting healthy tissue.
| Technological Advancement | Description | Impact on Treatment |
| Linear Accelerators | Devices that accelerate electrons to produce high-energy X-rays | Improved precision and effectiveness in treating tumors |
| Stereotactic Radiosurgery | Technique for delivering precise, high-dose radiation to specific targets | Enhanced ability to treat complex conditions with minimal damage to surrounding tissue |
| Image-Guided Radiation Therapy | Use of imaging technologies to guide radiation delivery | Increased accuracy and reduced risk of complications |
Advanced imaging like MRI and CT scans has made radiation therapy more accurate. These changes have made radiation therapy a precise and effective treatment. It offers hope to those with complex conditions.
Stereotactic Radiosurgery: Definition and Fundamental Concepts
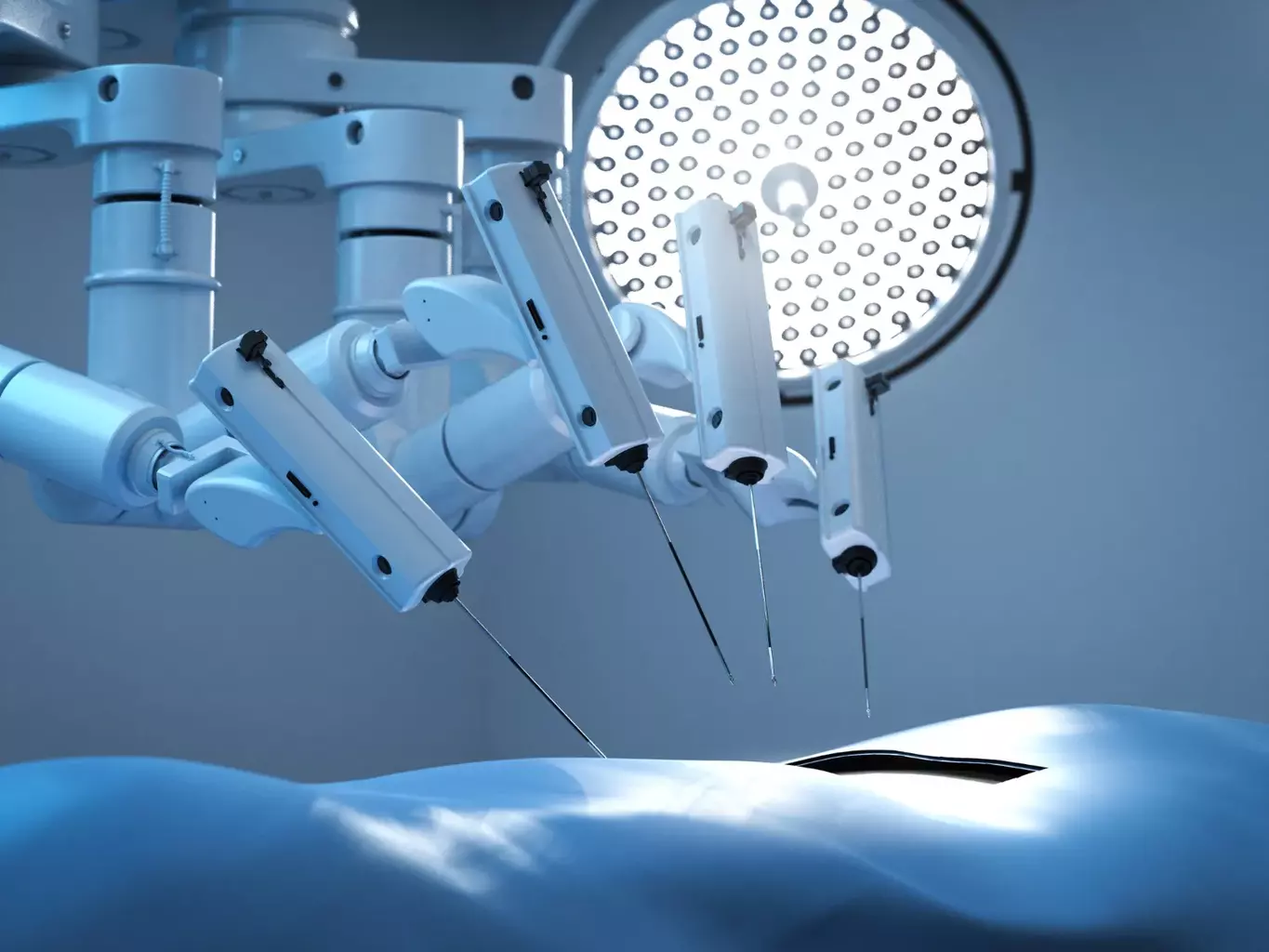
Stereotactic radiosurgery is a big step forward in medical tech. It lets doctors treat many conditions without cutting the skin. This method has changed how we treat tumors and other problems.
The key idea behind stereotactic radiosurgery is sending focused radiation beams to a specific spot. This means a high dose of radiation goes to the tumor, but not to healthy tissue nearby.
The “Surgery Without a Knife” Approach
Stereotactic radiosurgery is called “surgery without a knife” because it’s like surgery but without cutting. This way, it avoids the risks of regular surgery, like infections and anesthesia problems.
Doctors use top-notch imaging and software to pinpoint the area to treat. This lets them give a strong dose of radiation right to the tumor, protecting the rest of the tissue.
Precision Targeting and High-Dose Delivery
The success of stereotactic radiosurgery comes from its ability to target exactly. Doctors use MRI and CT scans to find the target with great accuracy. Then, they plan how to give the best dose of radiation.
The high dose needed for stereotactic radiosurgery comes from focusing many radiation beams at the target. This focused dose is strong enough to kill tumor cells or fix other problems. But, the tissue around gets much less radiation, which means fewer side effects.
Conventional Radiation Therapy vs. Radiosurgery: Key Differences
Conventional radiation therapy and radiosurgery are two different ways to treat diseases. They are used for various conditions, like cancer. But they have different methods and results.
Delivery Methods and Precision Targeting
Conventional radiation therapy uses beams from many angles to hit a tumor. This can sometimes harm nearby healthy tissues because of the larger beam size. On the other hand, stereotactic radiosurgery, or surgical radiation, focuses a strong dose of radiation on a small area. This reduces damage to nearby tissues.
The stereotactic radiosurgery method is precise thanks to advanced imaging and location techniques. This precision is key for treating tumors or conditions in sensitive areas, like the brain.
Treatment Duration and Session Requirements
Another big difference is in how long treatment takes and how many sessions are needed. Conventional radiation therapy usually requires many sessions over weeks. This way, the total dose is effective against the tumor but also reduces side effects.
Stereotactic radiosurgery often needs just one session or a few, depending on the condition and dose needed. Its high precision and focused delivery make it a good option for some patients, as it can treat in fewer sessions.
It’s important for patients and doctors to understand these differences when choosing a treatment. The type, size, and location of the tumor, along with the patient’s health, help decide between conventional radiation therapy or stereotactic radiosurgery.
Types of Stereotactic Radiosurgery Systems
The field of stereotactic radiosurgery includes Gamma Knife, LINAC, and proton beam therapy. These systems meet different needs and conditions. They offer various treatment options for patients.
Gamma Knife Technology
Gamma Knife radiosurgery uses Cobalt60-based photons for precise radiation. It’s great for treating brain tumors and vascular malformations. The system converges multiple gamma beams on the target, protecting nearby tissue.
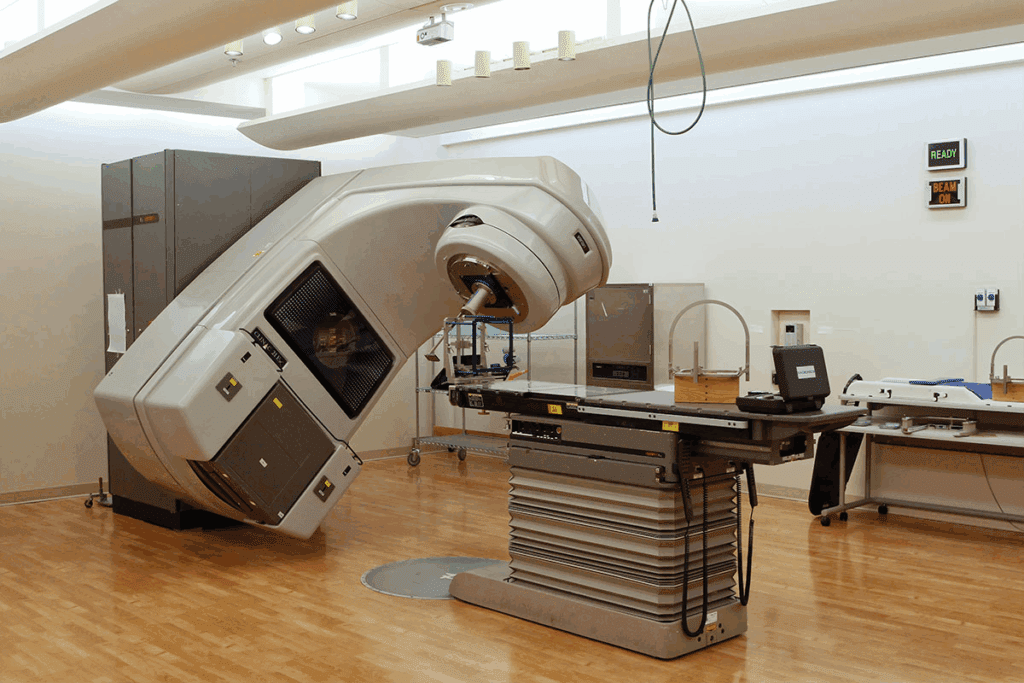
Linear Accelerator (LINAC) Systems
LINAC-based radiosurgery uses high-energy X-rays to kill cancer cells. These systems are versatile and treat many conditions. LINAC systems deliver precise, high-dose radiation with little harm to healthy tissue.
Proton Beam Therapy
Proton beam therapy uses protons to kill cancer cells. It’s precise, reducing damage to surrounding tissue. This therapy is good for tumors near critical structures.
| Technology | Description | Applications |
| Gamma Knife | Cobalt60-based photon technology | Brain tumors, vascular malformations |
| LINAC | High-energy X-rays | Various tumors, body parts |
| Proton Beam Therapy | Particle beam using protons | Tumors near critical structures |
In conclusion, the right stereotactic radiosurgery system depends on the condition and patient needs. Knowing the different technologies helps in making informed treatment choices.
Stereotactic Radiotherapy vs. Stereotactic Radiosurgery
It’s important to know the difference between stereotactic radiotherapy and stereotactic radiosurgery. Both use precise radiation, but they differ in how they deliver the dose. This affects the treatment’s success and side effects.
Fractionation Schedules and Dose Delivery
Stereotactic radiosurgery gives a high dose of radiation all at once to a small area. Stereotactic radiotherapy, on the other hand, gives lower doses over time to larger areas. This difference affects how well the treatment works and its side effects.
The way stereotactic radiotherapy is given allows for treating bigger tumors or those in sensitive spots. It lets healthy tissues recover between doses. Stereotactic radiosurgery is better for smaller, more precise targets.
- Stereotactic radiosurgery is used for small, well-defined tumors or lesions.
- Stereotactic radiotherapy is more flexible and can treat a wider range of tumor sizes and locations.
Clinical Applications and Selection Criteria
Choosing between stereotactic radiotherapy and stereotactic radiosurgery depends on several factors. These include the tumor’s size, location, and the patient’s health. Stereotactic radiosurgery is often used for certain brain conditions or small brain tumors.
Stereotactic radiotherapy is preferred for larger tumors or those near important structures. A team of healthcare professionals decides the best treatment based on the patient’s needs.
- Tumor size and location are key in choosing between the two treatments.
- The patient’s health and history also play a role in the decision.
- A team of healthcare professionals chooses the best treatment option for each patient.
Targeted Radiotherapy for Brain Conditions
Stereotactic radiosurgery is a new way to treat brain conditions. It’s a non-invasive method that uses precise radiation. This helps avoid damage to healthy brain tissue.
Primary and Metastatic Brain Tumors
Stereotactic radiosurgery is great for treating brain tumors. It works well on both benign and malignant tumors. This method helps control tumor growth and keeps brain function intact.
The size and location of the tumor matter. Tumors near important brain areas need very precise treatment to avoid harm.
Ar Page teriovenous Malformations and Vascular Disorders
Arteriovenous malformations (AVMs) can be treated with stereotactic radiosurgery. AVMs are abnormal brain connections that can cause bleeding. Radiosurgery aims to close off these malformations to stop future bleeding.
“Stereotactic radiosurgery has revolutionized the treatment of cerebral AVMs, providing a safe and effective option compared to surgery or embolization.”
Expert Opinion
telef ulnar disorder
Functional Disorders and Neurological Conditions
Stereotactic radiosurgery is also used for functional disorders like trigeminal neuralgia. It’s precise, which means less risk of complications.
Page tr>
| Condition | Treatment Approach | Benefits |
| Primary Brain Tumors | Stereotactic Radiosurgery | Precision targeting, minimal damage to healthy tissue |
| Arteriovenous Malformations | Stereotactic Radiosurgery | Non-invasive, effective in preventing hemorrhage |
| Functional Disorders | Stereotactic Radiosurgery | Minimally invasive, reduces risk of complications |
In conclusion, stereotactic radiosurgery is a big step forward in treating brain conditions. It’s precise and effective, tailored to each patient’s needs.
Applications of Radiosurgery Beyond the Brain
Stereotactic radiosurgery is a precise tool for treating tumors in various parts of the body. It’s not just for brain conditions anymore. Thanks to technology, it’s now used for different cancers and conditions.
First, it was used for brain tumors. Now, it’s also for tumors in other key areas. This is a non-invasive option compared to traditional surgery.
Spine and Spinal Cord Treatments
Stereotactic radiosurgery is used for spine and spinal cord tumors. It’s great for those who can’t have surgery or have tumors that come back. It delivers precise radiation to the tumor, protecting the spinal cord.
Many patients see pain relief and better function after treatment. Detailed imaging helps target the tumor without harming nearby tissue.
Lung, Liver, and Prostate Applications
Radiosurgery is also used for lung, liver, and prostate tumors. For lung cancer, it’s known as SBRT. It’s good for early-stage disease or when surgery isn’t possible.
In liver cancer, SBRT is a non-invasive option for inoperable tumors. For prostate cancer, it’s precise and can reduce side effects compared to traditional radiation.
Emerging Applications in Other Body Regions
Technology keeps improving, and radiosurgery is being used in more areas. It’s being looked at for tumors in the pancreas and kidney. Its precision makes it a promising option for many cancers.
Clinical trials are showing promising results. Radiosurgery could soon be a key treatment for more patients.
| Treatment Area | Application | Benefits |
| Spine and Spinal Cord | Treatment of tumors | High precision, minimal damage to surrounding tissue |
| Lung | SBRT for lung cancer | Non-invasive, effective for early-stage disease |
| Liver | SBRT for liver cancer | Non-invasive, effective for inoperable tumors |
| Prostate | Stereotactic radiosurgery | High precision, fewer side effects |
The Stereotactic Radiosurgery Procedure: Patient Experience
Stereotactic radiosurgery is a key treatment option. It’s a safe and effective way to treat conditions without traditional surgery. This method is precise, delivering high doses of radiation to specific areas. It helps avoid damage to healthy tissue nearby.
Pre-Treatment Planning and Imaging
The journey to stereotactic radiosurgery starts with detailed planning and imaging. This step is vital to pinpoint the exact location and size of the target area. Advanced imaging like MRI, CT scans, or angiography are used to gather the needed information.
During this phase, the patient undergoes simulation to find the best treatment position. Immobilization devices may be used to keep the patient steady during the procedure. A team of experts, including radiation oncologists and neurosurgeons, creates a treatment plan that fits the patient’s needs.
Key aspects of pre-treatment planning include:
- Detailed imaging to identify the target area
- Simulation to determine the optimal treatment position
- Creation of a customized treatment plan
The Treatment Experience and Immobilization
On the day of the procedure, patients are placed on a treatment table. Immobilization devices are used to ensure accuracy. The treatment is painless and non-invasive, with the patient lying quietly while the radiation is delivered.
The treatment time varies based on the case’s complexity and technology used. Gamma Knife radiosurgery can take several hours, while LINAC-based treatments are quicker. The treatment team closely monitors the process to ensure everything goes smoothly.
The treatment experience is designed to be as comfortable as possible, with the goal of delivering precise radiation therapy.
Post-Treatment Care and Monitoring
After treatment, patients are watched for a short time before being sent home. Follow-up care is essential to check the treatment’s success and manage side effects. Patients are given instructions on when to start normal activities again.
Follow-up appointments are set to track the patient’s progress and adjust the treatment plan if needed. The frequency of these appointments depends on the patient’s condition and treatment specifics.
Post-treatment care includes:
- Monitoring for immediate side effects
- Scheduling follow-up appointments
- Adjusting the treatment plan as necessary
Benefits and Advantages of Radiosurgery Over Traditional Radiation
Stereotactic radiosurgery has many benefits that make it better than traditional radiation therapy. It can give precise doses of radiation to specific areas. This reduces harm to healthy tissue nearby. A leading expert says, “Radiosurgery has changed how we treat some medical conditions. It’s a non-invasive, effective way instead of traditional surgery.” This precision is a big step forward in radiation therapy.
Precision and Reduced Damage to Healthy Tissue
Radiosurgery’s precision is a key advantage. It uses advanced imaging and delivery systems for sub-millimeter accuracy. This means less harm to healthy tissue, unlike traditional radiation therapy. This leads to a more effective treatment with fewer side effects.
Outpatient Procedure with Minimal Recovery Time
Radiosurgery is often done on an outpatient basis, so patients can go home the same day. It’s non-invasive, causing little discomfort during and after. Recovery time is much shorter than traditional surgery, allowing patients to get back to normal quickly. This makes radiosurgery a convenient and efficient option for many.
Quality of Life Considerations
Patients undergoing radiosurgery usually have a better quality of life than those with traditional radiation therapy. The precision of radiosurgery lowers the risk of side effects. Plus, the quick recovery time lets patients get back to their lives fast. This is very important for those with busy lives or other health issues. Overall, radiosurgery is a valuable option that balances effectiveness with quality of life.
Potential Risks and Side Effects of Both Treatment Modalities
Radiation therapy and radiosurgery have big benefits. But, knowing their side effects is key for making smart choices about surgical radiation.
Short-Term Side Effects
People getting stereotactic rt might feel tired, swollen, and have other quick reactions. These effects usually go away with the right care. Common short-term side effects include:
- Skin reactions
- Fatigue
- Nausea and vomiting
- Hair loss
Long-Term Considerations and Radiation Necrosis
Radiation necrosis is a big worry with surgical radiation. It happens when healthy tissue gets damaged by radiation, which can cause serious problems. Other long-term issues include:
| Long-Term Effect | Description |
| Radiation Necrosis | Damage to healthy tissue due to radiation |
| Secondary Cancers | Risk of developing new cancers due to radiation exposure |
| Organ Dysfunction | Potential damage to organs depending on the radiation site |
Risk Factors and Patient Selection
Choosing the right patient is key to lowering risks with stereotactic rt. Health, the condition being treated, and past treatments are all considered. Knowing these factors helps make better choices.
Healthcare providers can offer safer, more effective treatments by carefully looking at these factors and understanding side effects.
How Doctors Determine the Right Radiation Approach for Patients
Choosing the right radiation therapy is a detailed process. Doctors look at many factors to find the best treatment for each patient.
Diagnostic Criteria and Tumor Characteristics
The first step is to check the tumor’s type, size, and where it is. This helps doctors decide the best treatment. For example, stereotactic radiosurgery works well for small, clear tumors. But, conventional radiation therapy might be better for bigger or spread-out tumors.
The tumor’s biology is also key. Knowing how the tumor grows helps doctors choose the right radiation therapy.
Patient-Specific Factors in Treatment Selection
Doctors also look at the patient’s health and what they prefer. For instance, some patients might not do well with long treatments. So, stereotactic radiosurgery could be a better choice for them.
They also think about how treatment will affect the patient’s life. Doctors aim to find a balance between treating the tumor and keeping the patient’s quality of life good.
Multidisciplinary Approach to Treatment Planning
A team of experts works together to plan treatment. This team includes radiation oncologists, neurosurgeons, and radiologists. They all come together to decide the best radiation therapy.
They might consider using Gamma Knife or other stereotactic radiosurgery systems. The choice depends on what the patient needs and the tumor’s characteristics.
Conclusion: Making Informed Decisions About Radiation and Radiosurgery Options
It’s important for patients to know the difference between radiation therapy and radiosurgery. Stereotactic radiosurgery is a precise treatment for many conditions, like brain tumors and vascular disorders.
Patients can make better choices by learning about radiation therapy and radiosurgery. They need to understand how each works, including delivery methods and precision.
Medical technology keeps getting better, making radiosurgery more effective and less harmful. Patients should talk to their doctors to find the best treatment for them.
Being well-informed helps patients get the best care. Knowing about radiation therapy and radiosurgery lets them take charge of their health. This leads to better health outcomes.
FAQ
What is the difference between radiation therapy and radiosurgery?
Radiation therapy is a wide term for treatments using radiation to kill or slow cancer cells. Radiosurgery is a precise type of radiation therapy. It gives a strong dose of radiation to a specific area in one session.
What is stereotactic radiosurgery?
Stereotactic radiosurgery is a non-invasive method. It uses targeted radiation to treat tumors and other brain disorders. It’s called “surgery” because it works like traditional surgery but without an incision.
How does radiation therapy work?
Radiation therapy damages cancer cells’ DNA, stopping them from growing. It aims to give enough radiation to the tumor while protecting healthy tissue.
What are the different types of stereotactic radiosurgery systems?
There are three main types: Gamma Knife, Linear Accelerator (LINAC), and proton beam therapy. Each is designed for specific treatments.
What is the difference between stereotactic radiotherapy and stereotactic radiosurgery?
Stereotactic radiotherapy uses radiation in multiple sessions. Stereotactic radiosurgery uses a single session. The choice depends on the condition and the patient’s health.
What are the benefits of radiosurgery compared to traditional radiation therapy?
Radiosurgery is precise, causes less damage to healthy tissue, and has quick recovery times. It’s often done as an outpatient procedure, allowing patients to quickly return to their daily activities.
What are the possible risks and side effects of radiosurgery?
Radiosurgery can have risks like radiation necrosis and swelling. But these are rare. Careful planning helps minimize these risks.
How do doctors determine the right radiation approach for patients?
Doctors look at many factors like tumor characteristics and patient health. A team of healthcare professionals creates a treatment plan tailored to each patient.
Can radiosurgery be used to treat conditions beyond the brain?
Yes, radiosurgery can treat tumors in the spine, lung, liver, and prostate. Specialized equipment and techniques are used for these areas.
What is the role of pre-treatment planning in stereotactic radiosurgery?
Pre-treatment planning is key in stereotactic radiosurgery. It involves detailed imaging and mapping. This ensures the radiation targets the tumor while protecting healthy tissue.
How does targeted radiotherapy work for brain conditions?
Page $one
Targeted radiotherapy for brain conditions delivers precise radiation to specific brain areas. It treats various brain tumors and disorders.
References
Nature. Evidence-Based Medical Insight. Retrieved from https://www.nature.com/articles/nrclinonc.2010.169