Last Updated on December 1, 2025 by Bilal Hasdemir
Recent studies have shown that stereotactic radiosurgery (SRS) greatly improves life expectancy for patients with brain metastases.
We are seeing a big change in treating brain tumors and abnormalities. SRS is now a very effective and precise radiation therapy. Knowing the prognosis following SRS is key for both patients and healthcare providers.
We aim to deeply explore life expectancy after SRS. We want to highlight the factors that affect patient outcomes and the big impact on care.
Key Takeaways
- SRS is a precise radiation therapy for brain tumors and abnormalities.
- Improved life expectancy is a significant benefit of SRS.
- Understanding prognosis is key for patient care.
- Factors influencing patient outcomes will be discussed.
- SRS represents a big change in treating brain conditions.
Understanding Stereotactic Radiosurgery (SRS)
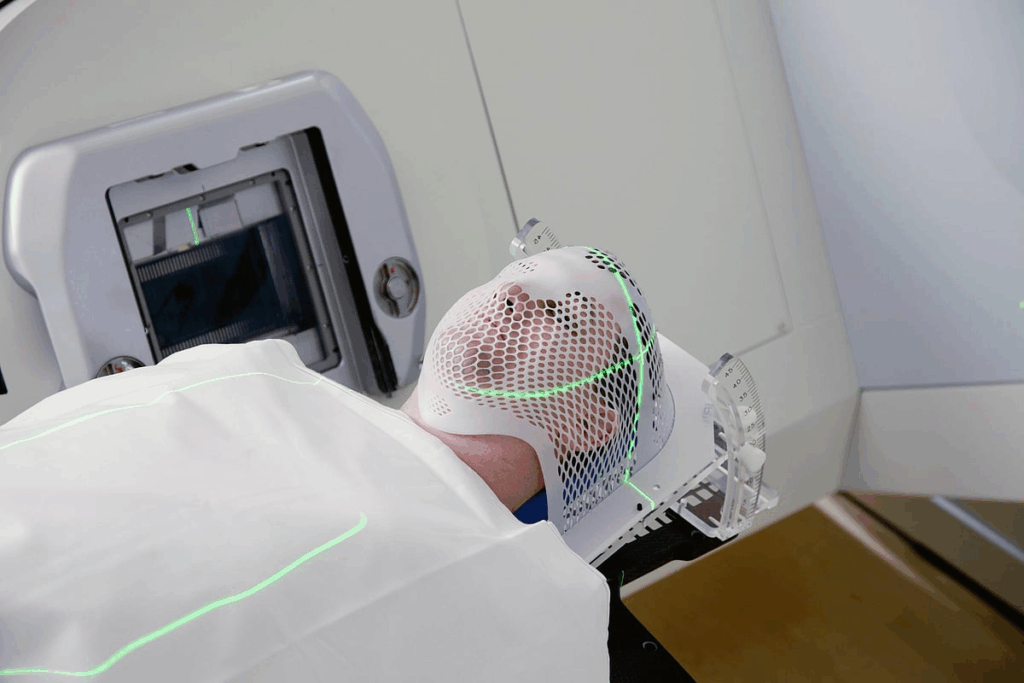
SRS is a non-surgical way to treat the brain. It sends precise, high doses of radiation to specific spots. This method is a big change from old surgery ways, being less invasive and very effective.
Definition and Basic Principles
SRS is a medical method that uses targeted radiation for brain lesions and tumors. It’s not a real surgery because it doesn’t cut you open. Instead, it uses new tech to hit the right spots in the brain.
The goal of SRS is to hit the target hard but not the healthy parts around it. It does this by planning and using special systems to shape the radiation just right.
Common Applications of SRS
SRS helps with many brain problems, like brain metastases, acoustic neuromas, and AVMs. It’s great for hard-to-reach or sensitive areas in the brain. This makes it a top choice for tricky cases.
Condition | Description | SRS Benefits |
Brain Metastases | Metastatic cancer that has spread to the brain | Non-invasive, precise treatment |
Acoustic Neuromas | Benign tumors on the nerve connecting the inner ear to the brain | Preserves hearing, minimizes complications |
Arteriovenous Malformations (AVMs) | Abnormal connections between arteries and veins in the brain | Reduces risk of bleeding, non-surgical |
Knowing how SRS works helps both patients and doctors. It helps them decide if it’s the right choice for brain problems.
Stereotactic Radiosurgery Life Expectancy: An Overview
The life expectancy of patients after stereotactic radiosurgery (SRS) varies a lot. It depends on several factors. Knowing these factors helps predict outcomes and make better treatment choices.
Median Survival Rates
Many studies have looked into median survival rates after SRS. The results show a wide range. For example, one study might say a median survival of 12 months. Another might find a longer or shorter survival time, based on the patients and treatment.
Let’s look at some data from recent studies:
Factors Influencing Overall Survival
Many things affect how long a patient lives after SRS. These include the type of cancer, how well the patient is doing, and how much disease is outside the brain. Knowing these factors helps doctors predict how well a patient will do.
For instance, patients who are doing better tend to live longer. Also, having disease outside the brain can make a big difference in life expectancy.
Here’s a table summarizing some key factors and their impact on survival:
Prognostic Factor | Impact on Overall Survival |
Primary Cancer Type | Varies; some cancers have better prognosis than others |
Performance Status | Higher status correlates with better survival |
Extracranial Disease Burden | Presence and extent negatively impact survival |
Tumor Volume and Location | Smaller tumors and favorable locations improve survival |
Understanding these factors helps doctors give more accurate predictions. They can then tailor treatments to meet each patient’s needs.
Brain Metastases and SRS Outcomes
Brain metastases greatly affect the results of Stereotactic Radiosurgery (SRS). This treatment has changed how we manage brain tumors. Brain metastases are common in many cancers and make treatment plans harder.
Single vs. Multiple Brain Metastases
People with one brain metastasis usually do better than those with more. Research shows that how many metastases you have affects your survival after SRS. Those with just one metastasis often have a better chance of survival, with survival times ranging from 9 to 12 months in some cases.
On the other hand, those with many brain metastases face a tougher road. Their survival times are usually lower than those with only one metastasis. But, new SRS methods have helped improve their chances too.
Primary Cancer Type and Its Impact
The type of cancer also affects survival after SRS. Different cancers spread to the brain and react differently to SRS. For example, patients with breast or melanoma brain metastases may have different outcomes than those with lung cancer metastases.
“The primary tumor type is a significant factor in determining the outcome of SRS for brain metastases, highlighting the need for personalized treatment approaches.”
Recursive Partitioning Analysis (RPA) Classification
The Recursive Partitioning Analysis (RPA) classification helps predict patient outcomes. It looks at patient age, how well they can function, and how much cancer is outside the brain. Patients in RPA Class I usually have a better outlook than those in Class III.
Knowing the RPA classification helps doctors sort patients by risk. This guides treatment choices and can lead to better results.
Prognostic Factors Affecting Post-SRS Survival
Many factors influence survival after Stereotactic Radiosurgery (SRS). These include how well the patient can function and the tumor’s characteristics. Knowing these factors helps doctors give better care and predictions to patients.
Patient Performance Status
A patient’s health and daily activity level are key. The Karnofsky Performance Status (KPS) scale measures this. Research shows that patients with higher KPS scores live longer after SRS.
A high performance status means a patient can better handle treatment and recover.
A study in the Journal of Neuro-Oncology found a big difference in survival rates. Patients with a KPS score of 70 or higher lived longer than those with lower scores. This shows how important performance status is for survival after SRS.
Tumor Volume and Location
The size and location of the tumor also matter. Bigger tumors are harder to treat and often have a worse outlook. The tumor’s location in the brain can also affect treatment success, with some areas being harder to reach.
Tumor Characteristic | Impact on Survival |
Tumor Volume | Larger tumors generally have poorer survival outcomes |
Tumor Location | Tumors in critical or hard-to-reach areas may have worse prognosis |
Age and Female Survival Advantage
Age also plays a role in survival after SRS. Younger patients usually do better than older ones. Some studies also suggest that women might live longer than men after SRS, but the reasons are not fully understood.
“The influence of gender on survival after SRS is an area of ongoing research, with some evidence suggesting that female patients may have a survival benefit,” according to a study in the Journal of Neurosurgery.
We looked at how age affects survival. Our findings showed that patients under 65 tend to live longer than older ones. This is likely due to better health and fewer health problems.
Local Control Rates and Their Relationship to Survival
Getting local control is key in Stereotactic Radiosurgery (SRS). It directly affects survival rates. Local control means stopping tumor growth at the treated site. This is vital for better patient outcomes.
Defining Local Control
Local control in SRS means getting rid of or stopping the tumor without it coming back. It shows how well the treatment works.
Long-term Local Control Statistics
Research shows SRS gets high local control rates for many tumors. For brain metastases, rates are 70-90% in one year. Here are some important stats:
- High local control rates: SRS often stops tumor growth in many patients.
- Variability based on tumor type: Rates change with the type of tumor and its details.
- Importance of dose and fractionation: The dose and how it’s given are key to success.
Recurrence Patterns and Management
Even with high local control, tumors can come back. Knowing how and when they do helps us manage better. Common ways include:
- Local recurrence: Coming back at the original site, often treated with SRS again or other local methods.
- Distant recurrence: New tumors in other parts of the brain or body, needing treatments like whole-brain radiation.
Handling recurrence needs a team effort. This might include more SRS, surgery, chemo, or immunotherapy. It depends on the situation and how the patient is doing.
By understanding local control and managing recurrence well, we can boost survival and quality of life for SRS patients.
Extracranial Disease and Its Influence on Life Expectancy
Extracranial disease is a big factor in how long patients live after stereotactic radiosurgery (SRS). How much disease is outside the brain matters a lot. Doctors need to think about this when they talk about how long a patient might live after SRS.
Systemic Disease Burden
The systemic disease burden is how much cancer is in the body, not in the brain. More cancer spread means a lower chance of living longer. Patients with less cancer outside the brain usually do better than those with a lot.
Synchronous vs. Metachronous Metastases
When cancer spreads, how fast it does matters a lot. Metastases that show up right away are different from those that come later. Knowing this helps doctors plan better treatments to help patients live longer.
Studies show that patients with cancer that spreads later might live longer than those with it right away. This shows why it’s key to know when cancer spreads to plan for the future.
SRS for Non-Metastatic Conditions
SRS is now used to treat many non-metastatic brain conditions. It’s a non-invasive option compared to traditional surgery. This method has shown great promise in treating conditions that were hard to manage before.
Arteriovenous Malformations (AVMs)
AVMs are abnormal connections between arteries and veins. They can cause serious problems if not treated. SRS for AVMs is a common treatment, with a high success rate and few side effects.
Key benefits of SRS for AVMs include:
- Minimally invasive with no incision required
- Reduced risk of complications compared to open surgery
- High success rate in achieving obliteration
AVM Characteristics | Obliteration Rate | Complication Rate |
Small AVMs (<3 cm) | 80% | 5% |
Medium AVMs (3-6 cm) | 70% | 10% |
Large AVMs (>6 cm) | 50% | 15% |
Acoustic Neuromas
Acoustic neuromas, or vestibular schwannomas, are benign tumors on the vestibulocochlear nerve. SRS is a preferred treatment, aiming to control the tumor while preserving hearing and facial nerve function. Its precision allows for targeted radiation to the tumor, protecting nearby critical areas.
“Stereotactic radiosurgery has become an essential tool in the management of acoustic neuromas, providing excellent tumor control and minimizing the risk of complications.” – Expert in Neurosurgery
Primary Brain Tumors
SRS is also used for primary brain tumors like gliomas and meningiomas. It can be a definitive treatment for some, or used alongside surgery or chemotherapy for others. The role of SRS in treating primary brain tumors is growing, with ongoing research to improve treatment and outcomes.
Advantages of SRS for primary brain tumors:
- Non-invasive, reducing recovery time
- High precision, minimizing damage to surrounding brain tissue
- Effective for tumors in challenging locations
One-Year and Long-Term Survival Rates
The success of SRS is often seen in one-year and long-term survival rates. These rates give us insights into how well patients do after treatment. Survival rates can change a lot based on the condition treated, the patient’s health, and the SRS treatment details.
One-Year Survival Statistics
One-year survival rates after SRS are usually good. Studies show many patients live for at least a year after treatment. For example, a study on brain metastases treated with SRS found a one-year survival rate of about 45-50%. This means nearly half of these patients survive for at least a year. The survival rate can depend on the cancer type, how well the patient is doing, and if there’s disease outside the brain.
Five-Year Survival Data
Looking at five-year survival rates gives us a better view of SRS’s long-term success. For some conditions, the five-year survival rate is very high. For instance, patients with arteriovenous malformations (AVMs) treated with SRS have good five-year survival and obliteration rates. A study showed a five-year survival rate of 70-80% for AVM patients after SRS. This shows SRS can offer long-term benefits for the right patients.
Ten-Year Survivors: Characteristics and Outcomes
Ten-year survivors after SRS are very interesting. They show us what makes long-term survival possible. Studies found that being younger, having a good performance status, and no big disease outside the brain are key.
“Patients who survive ten years or more after SRS often have favorable tumor biology and minimal comorbidities,” according to recent studies.
Knowing these traits helps us pick the best candidates for SRS. This way, we can help more patients live longer and better.
In summary, survival rates after SRS depend on many things. By looking at one-year, five-year, and ten-year survival rates, we understand how well SRS works. This helps us improve patient care and outcomes.
SRS in the Targeted Therapy Era
The use of SRS with targeted therapy is changing how we treat patients. With new medical technology, combining SRS with other treatments is key.
Combining SRS with Immunotherapy
Studies show that mixing SRS with immunotherapy boosts treatment success. This method uses the body’s immune system to fight cancer better.
Immunotherapy boosts the immune system to attack cancer cells. When paired with SRS, it can lead to better local control and survival rates.
Survival Improvements with Combined Approaches
Using SRS and targeted therapy together has shown great results. Tailoring treatment to each patient’s needs leads to better outcomes.
Research shows patients getting SRS and immunotherapy live longer than those with SRS alone. This is a big win for patients with specific cancers.
- Enhanced local control
- Improved overall survival
- Better patient outcomes
As we keep exploring SRS in the targeted therapy era, combined treatments are vital. They will shape the future of cancer treatment.
Quality of Life After Stereotactic Radiosurgery
Checking how well patients do after SRS is key to good care. As we get better at radiation oncology, knowing how SRS affects patients’ lives is more important.
Neurocognitive Outcomes
How well the brain works after SRS is very important. Studies show SRS can affect brain function differently, based on the tumor’s location and size. It’s vital to plan and do SRS carefully to avoid brain function problems.
Patients with brain metastases treated with SRS can keep or even get better brain function. This is true when they also get the right support care.
The effects of SRS on brain function depend on several things. For example, how much radiation the hippocampus gets. Using new methods like sparing the hippocampus helps lessen brain side effects. We aim to control tumors well while keeping brain function good.
Symptom Control and Functional Independence
Managing symptoms well is key to a good life after SRS. Symptoms like headaches, seizures, and nerve problems greatly affect a patient’s happiness. SRS can really help with these symptoms, making patients more independent.
Being able to do daily tasks without help is linked to quality of life. SRS can stop tumors from growing and lessen symptoms. This helps patients stay or get better at doing things on their own. This makes their life better and lets them do things they enjoy.
We focus on controlling tumors and keeping patients independent with SRS. By choosing the right patients and making treatment plans just for them, we aim to improve what matters most to our patients.
Conclusion: The Future of SRS and Life Expectancy
As we move forward in the field of stereotactic radiosurgery (SRS), we see big changes ahead. These changes will greatly improve life expectancy and patient results. The future of SRS is bright, thanks to ongoing research and new technologies.
New technologies and treatment methods will make SRS even better. We expect to see better results from SRS, leading to longer and healthier lives for patients. SRS will become more precise, with fewer side effects, making life better for those undergoing treatment.
SRS will keep being a key part in treating many medical conditions. We’re excited for the future of SRS, which will bring better care and outcomes for patients. This is a big step forward in medical treatment.
FAQ
What is stereotactic radiosurgery (SRS) and how is it used to treat brain conditions?
Stereotactic radiosurgery (SRS) is a non-surgical treatment that uses precise radiation. It targets specific areas in the brain. We use it to treat brain conditions like brain metastases, AVMs, acoustic neuromas, and primary brain tumors.
What is the median survival rate after SRS for brain metastases?
The survival rate after SRS for brain metastases depends on several factors. These include the number of metastases, the type of primary cancer, and the patient’s health status. Generally, survival ranges from 6 to 12 months. But, it can be longer for those with controlled disease and good health.
How does the number of brain metastases affect SRS outcomes?
Patients with one brain metastasis usually have better outcomes than those with more. But, new SRS techniques and treatments have improved results for those with multiple metastases.
What prognostic factors influence post-SRS survival?
Several factors affect survival after SRS. These include the patient’s health status, tumor size and location, age, and gender. We also look at extracranial disease, primary cancer type, and RPA classification.
What is local control, and how does it relate to survival after SRS?
Local control means stopping tumor growth at the treated site. It’s key for better survival after SRS. It helps avoid neurological decline and improves quality of life.
How does extracranial disease affect life expectancy after SRS?
Extracranial disease can greatly affect life expectancy after SRS. Patients with controlled disease outside the brain tend to do better than those with active disease.
Can SRS be used to treat non-metastatic conditions, and what are the benefits?
Yes, SRS treats non-metastatic conditions like AVMs, acoustic neuromas, and primary brain tumors. It offers high control rates, is minimally invasive, and preserves brain function.
What are the one-year and long-term survival rates after SRS?
Survival rates after SRS vary based on the condition and patient factors. One-year survival is usually 50% to 80%. Long-term survival, like five or ten years, also depends on these factors, with some patients surviving longer.
How does combining SRS with immunotherapy or targeted therapy impact survival?
Combining SRS with immunotherapy or targeted therapy can improve survival. It enhances local control and addresses systemic disease. Early evidence suggests this combination can lead to better overall survival and even cure in some cases.
What are the neurocognitive outcomes after SRS, and how does it affect quality of life?
SRS aims to minimize brain function decline by targeting specific areas. It can preserve or improve quality of life. This is by controlling symptoms, maintaining independence, and reducing corticosteroid use.
What is the future of SRS, and how may it impact life expectancy?
Future research and advancements in SRS techniques will improve patient outcomes. Better imaging and radiation delivery are expected. These developments will likely increase life expectancy and quality of life for SRS patients.
References
National Center for Biotechnology Information. Evidence-Based Medical Insight. Retrieved from https://pmc.ncbi.nlm.nih.gov/articles/PMC10037943/