Last Updated on December 2, 2025 by Bilal Hasdemir
About 80% of adults will face lower back pain at some point. Many cases are due to sciatica from L5 nerve damage.
Dealing with L5 nerve damage is tough. It affects your health and happiness. The straight leg raise test helps figure out sciatica symptoms.
We’ll look into l4-l5 nerve damage and how to treat it. Knowing how to diagnose is key.
Learn if L5 nerve damage can be repaired after a positive straight leg. Understanding the healing potential and treatment clearly.
Key Takeaways
- Understanding the causes and symptoms of L5 nerve damage.
- The role of the straight leg raise test in diagnosing sciatica.
- Exploring treatment options for l4-l5 nerve damage.
- The importance of early diagnosis for effective treatment.
- Overview of sciatica symptoms and their impact.
Understanding L5 Nerve Anatomy and Function
The L5 nerve is in the lumbar spine and plays a key role in the lower body. It’s important to know its anatomy and how it works in the spinal system.
Location of L5 in the Lumbar Spine
The L5 nerve root is between the L4 and L5 vertebrae. It’s part of the lumbosacral plexus, which controls the lower limbs. The L5 nerve comes out of the spinal canal and goes through a narrow space between the vertebrae.
Areas Innervated by the L5 Nerve Root
The L5 nerve root controls several important muscles and areas in the lower limb. These include:
- The extensor hallucis longus muscle, which extends the big toe.
- The tibialis anterior muscle, which helps in ankle dorsiflexion.
- Sensory innervation to parts of the lower leg and foot.
This is key for walking, balance, feeling touch, and pain.
Normal Function and Importance of L5
The L5 nerve root’s normal function is vital for:
| Function | Description | Impact of Dysfunction |
| Motor Control | Controls muscles involved in ankle and toe movements. | Weakness or paralysis in foot and toe muscles. |
| Sensory Perception | Provides sensation to the lateral lower leg and dorsum of the foot. | Numbness, tingling, or pain in the areas innervated. |
| Gait and Balance | Essential for normal gait and balance functions. | Altered gait patterns, increased risk of falls. |
Knowing about the L5 nerve root’s anatomy and function is key for diagnosing and treating problems like sciatica and lumbar radiculopathy.
Common Causes of L5 Nerve Damage
Knowing why L5 nerve damage happens is key to treating it. The L5 nerve in the lower back controls many functions. Damage can come from spinal problems and injuries.
Many things can hurt the L5 nerve. Finding out what caused the damage helps choose the right treatment. We’ll look at the main causes, like structural problems and injuries.
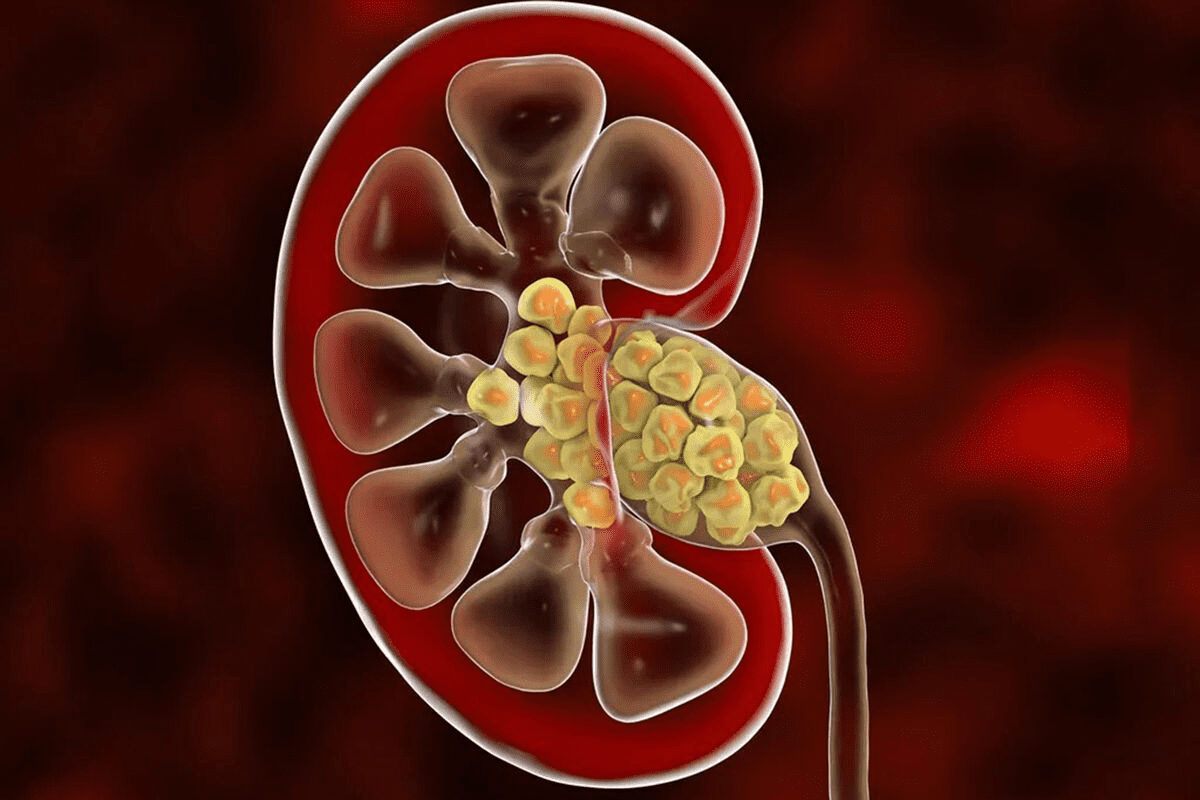
Herniated Discs at L4-L5 and L5-S1 Levels
Herniated discs at L4-L5 and L5-S1 are big causes of L5 nerve damage. A herniated disc happens when the soft center leaks out. This can hurt nearby nerves, causing pain and weakness.
The L4-L5 area is more likely to have herniated discs. When a disc presses on the L5 nerve, it can cause a lot of pain and make it hard to move.
Spinal Stenosis and Nerve Compression
Spinal stenosis is another common reason for L5 nerve damage. It’s when the spinal canal gets too narrow, pressing on nerves. This can happen due to aging or other spine problems.
When nerves get compressed, it can cause pain and weakness. Activities that stretch the spine can make it worse. But bending forward can help.
Key factors contributing to spinal stenosis include:
- Degenerative changes
- Osteoarthritis
- Disc degeneration
- Thickening of ligaments
Trauma and Other Causes
Lower back trauma can also damage the L5 nerve. This can happen from accidents or sports injuries. The impact can cause fractures or direct nerve damage.
Less common causes include infections, tumors, and birth defects. These can also harm the L5 nerve, leading to symptoms.
In summary, L5 nerve damage can come from many sources. Understanding these causes is vital for effective treatment.
Recognizing L5 Nerve Damage Symptoms
Knowing the signs of L5 nerve damage is important. It helps patients get the right medical care early. The L5 nerve controls muscles in the lower leg and foot and provides sensation to these areas.
Motor Symptoms and Weakness
L5 nerve damage can cause muscle weakness or paralysis. This might make it hard to lift the foot or move the toes. Walking can also become difficult.
Common motor symptoms include:
- Weakness in ankle dorsiflexion (lifting the foot upwards)
- Difficulty walking on heels
- Foot drop, where the foot drags on the ground during walking
Sensory Symptoms and Pain Patterns
Sensory symptoms from L5 nerve damage include pain, numbness, or tingling. The pain often goes down the back of the leg and to the top of the foot. These symptoms help doctors figure out if it’s L5 nerve damage.
The pain from L5 nerve damage is sharp, shooting, or burning. It gets worse with activities that put pressure on the nerve, like coughing or heavy lifting.
Differentiating L5 from L4 and S1 Nerve Damage
Telling L5 nerve damage apart from L4 and S1 nerve damage is important. While the nerves overlap, specific patterns can point to the right nerve root.
| Nerve Root | Motor Symptoms | Sensory Symptoms |
| L4 | Weakness in knee extension | Numbness on the inner aspect of the lower leg |
| L5 | Foot drop, weakness in ankle dorsiflexion | Pain or numbness on the top of the foot |
| S1 | Weakness in ankle plantarflexion | Numbness on the outer aspect of the foot |
Knowing these differences is key to diagnosing and treating nerve damage. A detailed neurological exam is needed to find the right nerve root.
The Straight Leg Raise Test for Sciatica
The straight leg raise test is key for diagnosing sciatica and nerve damage. It’s also known as Lasègue’s test. It checks for sciatic pain and its link to lumbar disc herniation or other sciatica causes.
Proper Technique for Performing the Test
To do the straight leg raise test right, the patient lies on their back. We lift their leg straight up to see when pain starts. Pain down the leg is a sign of sciatica, usually between 30 to 70 degrees.
Key steps in performing the SLR test:
- Patient lies on their back
- Leg is slowly lifted while keeping it straight
- Angle of pain onset is noted
- Presence of radiating pain is observed
Interpreting Test Results
A positive test means sciatic nerve irritation or compression. This is often due to a herniated disc or lumbar spine issues. The test’s accuracy can vary, but it’s very helpful in medical practice.
| Test Result | Interpretation |
| Positive | Sciatic nerve irritation or compression likely |
| Negative | Less likely to have significant sciatic nerve compression |
Limitations and Variations of the Test
The straight leg raise test has its limits. Patient cooperation, other health issues, and technique can impact its results. There are also test variations, like the crossed straight leg raise test, for more info.
Knowing about the straight leg raise test helps doctors decide on next steps for sciatica patients.
Additional Diagnostic Methods for L5 Nerve Damage
Diagnosing L5 nerve damage needs a detailed approach. The Straight Leg Raise Test is helpful but not enough. More tests are needed to fully understand the damage.
Imaging Studies: MRI, CT, and X-rays
Imaging studies are key in diagnosing L5 nerve damage. They show the spine and its surroundings in detail. Magnetic Resonance Imaging (MRI) is great for seeing soft tissues like nerves and discs. It can spot herniated discs and nerve compression.
Computed Tomography (CT) scans are good for bones. They help find bone spurs or fractures that might harm the L5 nerve. But, they’re not as good as MRI for soft tissues.
X-rays are first used to check the spine’s alignment. They can find big bony problems. But, they don’t show soft tissues as well as MRI.
Electromyography (EMG) and Nerve Conduction Studies
Electromyography (EMG) and Nerve Conduction Studies (NCS) test the L5 nerve’s function. EMG checks muscle electrical activity. It can show if a muscle is getting the right nerve signals.
NCS look at how fast and strong nerve signals are. They’re often used for nerve injuries but can also check nerve roots.
Physical Examination Techniques Beyond SLR Test
There are more ways to check the L5 nerve than just the Straight Leg Raise Test. These include:
- Manual muscle testing to check muscle strength
- Sensory testing for numbness or odd sensations
- Reflex testing, though L5 doesn’t have a specific reflex
- Looking at how you walk and move your legs
These tests, along with imaging and electrophysiology, give a full picture of L5 nerve damage. They help doctors decide the best treatment.
Can Damaged Nerves Regenerate?
Nerve regeneration is a complex process. It depends on how severe the damage is. Knowing if nerves can heal is key for those with nerve damage.
The Science of Nerve Repair and Regeneration
Nerve repair and regeneration are complex. When nerves are damaged, the body first gets inflamed. Then, it starts repairing the nerve fibers.
Nerve regeneration goes through several stages:
- Degeneration: The damaged nerve fiber breaks down, making room for new growth.
- Regeneration: New nerve fibers start growing from the injury site towards their targets.
- Remyelination: These new fibers get a myelin sheath, helping them function better.
Factors Affecting Nerve Healing
Many things can affect how well nerves heal. These include:
| Factor | Description | Impact on Healing |
| Severity of Damage | The extent of nerve damage | More severe damage makes healing harder |
| Age | The patient’s age | Younger people usually heal nerves better |
| Overall Health | The patient’s general health condition | Poor health can slow down nerve healing |
How to Determine if Nerve Damage is Permanent
Figuring out if nerve damage is permanent needs a detailed check-up. Healthcare experts look at:
- How symptoms and medical history match up.
- Imaging tests like MRI or CT scans.
- Tests like EMG and nerve conduction studies.
Knowing about nerve regeneration and what affects it helps both patients and doctors. It guides treatment choices.
Conservative Treatment Approaches for L5 Nerve Damage
Managing L5 nerve damage well needs a detailed plan. Treatments aim to ease symptoms and boost life quality. They are often the first step in managing L5 nerve damage.
Medication Options for Pain and Inflammation
Medicines are key in fighting pain and swelling from L5 nerve damage. Here are some common ones:
- Nonsteroidal anti-inflammatory drugs (NSAIDs) to reduce inflammation and pain
- Oral corticosteroids to decrease swelling and inflammation
- Gabapentin or pregabalin to manage neuropathic pain
- Muscle relaxants to alleviate muscle spasms
Effective pain management is vital in the early stages. It lets patients do physical therapy and other rehab activities.
“Pain is a complex phenomenon that requires a multifaceted treatment approach. By combining different medication classes, we can often achieve better pain control and improve patient outcomes.”
— A Pain Management Specialist
Physical Therapy Interventions
Physical therapy is key in treating L5 nerve damage. A good physical therapy plan can help a lot:
| Therapy Component | Benefits |
| Stretching Exercises | Improve flexibility, reduce muscle tension |
| Strengthening Exercises | Enhance muscle support for the spine, improve stability |
| Nerve Mobilization Techniques | Reduce nerve irritation, promote healing |
Physical therapists create a custom exercise plan for each patient. They focus on the patient’s specific needs and goals.
Rest and Activity Modification
Rest and changing how you do things are key in treating L5 nerve damage. Patients should:
- Avoid heavy lifting and bending
- Modify daily activities to reduce strain on the lower back
- Gradually return to normal activities under the guidance of a healthcare provider
By mixing medicines, physical therapy, and lifestyle changes, we can make a detailed treatment plan. This plan meets the complex needs of patients with L5 nerve damage.
Therapeutic Exercises for L5 Nerve Recovery
L5 nerve damage can be very tough. But, special exercises can help ease symptoms and aid in healing. It’s key to have a plan that includes exercises for the core, nerve gliding, and slowly getting back to normal activities.
Core Strengthening Exercises
Strengthening the core is essential for supporting the spine and easing pressure on the L5 nerve. Planks, bridges, and pelvic tilts are great for keeping the lower back stable.
- Planks: Hold a straight line from head to heels for 30-60 seconds.
- Bridges: Lie on your back, knees bent, feet flat, and lift your hips up.
- Pelvic Tilts: Lie on your back, knees bent, tilt your pelvis up and then back down.
Nerve Gliding and Mobilization Techniques
Nerve gliding exercises help move the L5 nerve gently, which can reduce tension and aid in healing. It’s important to do these exercises with the help of a healthcare professional.
“Nerve gliding can be an effective method for reducing nerve tension and improving symptoms.” – A Physical Medicine Specialist
- Sciatic nerve glide: Slowly tilt your head towards your shoulder while extending the affected leg.
- Straight leg raise: Gradually lift the affected leg while keeping the knee straight.
Gradual Return to Activity Protocol
It’s important to return to activities slowly to avoid injury and ensure a full recovery. Start with easy activities like walking or swimming. Then, slowly increase the intensity and time spent doing them.
Interventional Procedures for L5 Nerve Damage
Interventional procedures are key for managing L5 nerve damage when other treatments fail. They offer relief for those with severe symptoms.
Epidural Steroid Injections
Epidural steroid injections are a common treatment for L5 nerve damage. They put corticosteroids near the nerve to cut down inflammation and pain.
The benefits of these injections include:
- Reduced inflammation around the affected nerve
- Significant pain relief for many patients
- Minimally invasive with a relatively quick recovery
But, there are risks like temporary side effects from corticosteroids and nerve damage during the procedure.
Nerve Blocks and Their Complications
Nerve blocks involve injecting local anesthetics or steroids around the affected nerve to block pain signals. They can be effective for severe pain, but there are risks.
Some complications include:
- Nerve damage from the injection
- Temporary or prolonged numbness
- Infection at the injection site
Talking to a healthcare provider about these risks is important. They can help decide if the benefits are worth the risks.
Emerging Minimally Invasive Techniques
New medical technologies have brought new, minimally invasive techniques for L5 nerve damage. These aim to reduce risks and provide effective pain relief.
Some new techniques include:
- Laser-assisted procedures
- Radiofrequency ablation
- Spinal cord stimulation
These techniques are promising, but it’s important to talk to a healthcare professional. They can help decide if they’re right for you.
Surgical Options for Repairing L5 Nerve Damage
When other treatments don’t work, surgery might be needed for L5 nerve damage. Surgery aims to ease nerve pressure, improve function, and reduce pain. We’ll look at the different surgeries available and who might need them.
Microdiscectomy and Decompression Procedures
Microdiscectomy is a small surgery to remove disc material pressing on the L5 nerve. It involves a small incision and a microscope to see the area. This can help relieve nerve pressure and ease pain.
Decompression focuses on removing bone spurs or thickened ligaments that press on the nerve. It can be done alone or with microdiscectomy, depending on the case.
Spinal Fusion Techniques
Spinal fusion joins vertebrae together with bone grafts and sometimes rods and screws. It’s for those with spinal instability or who haven’t improved with other treatments. This can stabilize the spine and help with pain.
There are different spinal fusion methods, like PLIF and TLIF. The choice depends on the patient’s condition and the surgeon’s preference.
Determining Surgical Candidacy
Deciding if surgery is right involves checking a patient’s health, symptom severity, and nerve damage cause. We look at neurological deficits, treatment failure, and structural issues that surgery can fix.
Patients will get MRI or CT scans to see nerve compression and spinal issues. Talking to a spine specialist is key to understand surgery’s benefits and risks and choose the best treatment.
Recovery Timeline and Prognosis
L5 nerve damage recovery is complex. It depends on damage severity and treatment success. Knowing these factors helps set realistic goals and achieve the best results.
Factors Affecting Recovery Outcomes
Many things affect L5 nerve damage recovery. These include the cause of damage, patient health, and treatment methods. For example, damage from a herniated disc might differ from that caused by spinal stenosis.
The initial damage’s severity is key. Mild damage might heal quickly with simple treatments. But severe damage may need more intense treatments and a longer recovery.
Setting Realistic Expectations
It’s important for patients to have realistic recovery hopes. Some may see big improvements in weeks, while others may take months. Age, health, and treatment adherence all play roles in recovery.
We suggest patients team up with their healthcare providers for a custom treatment plan. This teamwork helps set reachable goals and adjust hopes based on progress.
Success Rates for Different Treatment Approaches
Treatment success for L5 nerve damage varies by method. Conservative treatments like physical therapy and meds work well for mild to moderate cases. But for severe cases or when conservative methods fail, surgical interventions might be needed.
- Conservative management success rates range from 60% to 80% for patients with mild to moderate L5 nerve damage.
- Surgical interventions, such as microdiscectomy, have success rates ranging from 70% to 90% in appropriately selected patients.
Knowing the outcomes of different treatments helps patients make informed choices. By understanding recovery factors and treatment success rates, patients can better manage their recovery from L5 nerve damage.
When to Seek Immediate Medical Attention
It’s important to know the warning signs of severe L5 nerve damage. This is because some cases need quick medical help to avoid serious problems. Many L5 nerve damage cases can be treated without surgery, but some need urgent care.
Red Flag Symptoms
There are red flag symptoms that mean you should see a doctor right away. These include:
- Progressive weakness or numbness in the legs
- Loss of bladder or bowel control
- Saddle anesthesia (numbness in the groin area)
- Severe, unrelenting pain
If you notice any of these signs, get medical help fast.
Cauda Equina Syndrome and Other Emergencies
Cauda Equina Syndrome (CES) is a serious issue linked to L5 nerve damage. It happens when nerves in the lower spine get compressed. This can cause permanent damage if not treated quickly. Symptoms of CES include:
- Severe lower back pain
- Weakness or paralysis in the legs
- Numbness in the legs or groin area
- Loss of bladder or bowel function
CES is a medical emergency that needs quick surgery to avoid permanent damage. If you think you have CES or any red flag symptoms, get emergency medical care right away.
Thinking about these severe symptoms can be scary. But knowing what to do can help a lot. If you’re experiencing any red flag symptoms or think you might have Cauda Equina Syndrome, get medical help immediately.
Conclusion
Understanding L5 nerve damage and how to diagnose it is key for treating sciatica. We’ve looked at the L5 nerve’s role, why it gets damaged, and how to find out. The straight leg raise test is a helpful tool, but it’s often used with other tests too.
Fixing L5 nerve damage needs a full plan. This includes non-surgical steps, some procedures, and sometimes surgery. It’s vital to get the right medical help for L5 nerve damage and sciatica. Early and correct treatment can really help.
Understanding L5 nerve damage and available treatments helps patients make informed decisions. If you have sciatica symptoms, see a doctor. They can help find the best treatment for you.
FAQ
What is the L5 nerve, and what are its functions?
The L5 nerve comes from the fifth lumbar vertebra. It helps control movements like ankle dorsiflexion and toe extension. It also sends sensation to parts of the lower leg and foot.
What are the common causes of L5 nerve damage?
L5 nerve damage often comes from herniated discs at the L4-L5 level. It can also be caused by spinal stenosis, trauma, or other conditions that press or irritate the nerve.
How is L5 nerve damage diagnosed?
Doctors use a few methods to diagnose L5 nerve damage. They check with the straight leg raise test and use MRI or CT scans. They also do EMG and nerve conduction studies.
What is the straight leg raise test, and how is it performed?
The straight leg raise test checks for sciatica and L5 nerve root irritation. You lift your leg while keeping it straight. If you feel pain down your leg, it’s a positive test.
Can a herniated disc cause neuropathy in the feet?
Yes, a herniated disc can press on the L5 or S1 nerve roots. This can cause pain, numbness, and weakness in the lower leg and foot.
How can I determine if my nerve damage is permanent?
A doctor will do a full check-up to see if nerve damage is permanent. They look at your symptoms, do imaging studies, and check with electrophysiological tests. If your symptoms get better, it might not be permanent.
What are the treatment options for L5 nerve damage?
There are many ways to treat L5 nerve damage. You can start with medicine, physical therapy, and changing your lifestyle. Sometimes, doctors might suggest injections or surgery like microdiscectomy or spinal fusion.
What exercises can help in recovering from L5 nerve damage?
Doing exercises like core strengthening and nerve gliding can help. A doctor will guide you with exercises that fit your needs.
When should I seek immediate medical attention for L5 nerve damage symptoms?
You should see a doctor right away if you have severe pain, can’t control your bowel or bladder, or have a bad injury.
Can L5 nerve damage cause pain when bending over on one side?
Yes, bending over can hurt if you have L5 nerve damage. It’s because the movement can press on the nerve more.
What is the role of the L4 and L5 nerves in lower back pain?
The L4 and L5 nerves are key in lower back pain. When they’re compressed or irritated, like by herniated discs, it can cause pain that goes to the legs.