Last Updated on November 27, 2025 by Bilal Hasdemir

Prostate surgery is a big deal and can lead to stress urinary incontinence. Stress urinary incontinence can significantly impact one’s daily activities and overall quality of life. It’s crucial to understand the risks associated with prostate surgery and the available treatment options for subsequent urinary incontinence.stress incontinence treatment includes Kegel exercises and lifestyle changes. Learn effective methods to regain bladder control.
Awareness of the available treatment options empowers individuals to make informed health decisions.
Key Takeaways
- Prostate surgery can lead to stress urinary incontinence.
- It’s crucial to understand the risks associated with prostate surgery and the available treatment options for subsequent urinary incontinence.
- Talking to your doctor about your risks is very important.
- Awareness of the available treatment options empowers individuals to make informed health decisions.
- Making informed decisions can greatly improve your quality of life.
Understanding Prostate Surgery and Its Classification
Prostate surgery is classified based on several factors. These include the type of procedure and the condition being treated. It’s important to know about the prostate gland, its functions, and why surgery might be needed.
What is the Prostate and Its Function
The prostate is a gland the size of a walnut. It’s between the bladder and the penis. It plays a key role in the male reproductive system. It surrounds the urethra and helps produce seminal fluid, which supports sperm during ejaculation.
Common Conditions Requiring Prostate Surgery
Several conditions may need prostate surgery. These include prostate cancer, benign prostatic hyperplasia (BPH), and prostatitis. Prostate cancer often requires radical prostatectomy. BPH can cause urinary symptoms that surgery like TURP can help with.
Criteria for Classifying Surgeries as Major or Minor
Surgeries are classified by their complexity, risk, and the extent of the procedure. Major surgeries are risky, have longer recovery times, and are more complex. Minor surgeries are less invasive, have quicker recovery times, and are simpler.
| Criteria | Major Surgery | Minor Surgery |
| Complexity | High | Low |
| Risk | Significant | Minimal |
| Recovery Time | Longer | Quicker |
Types of Prostate Surgical Procedures
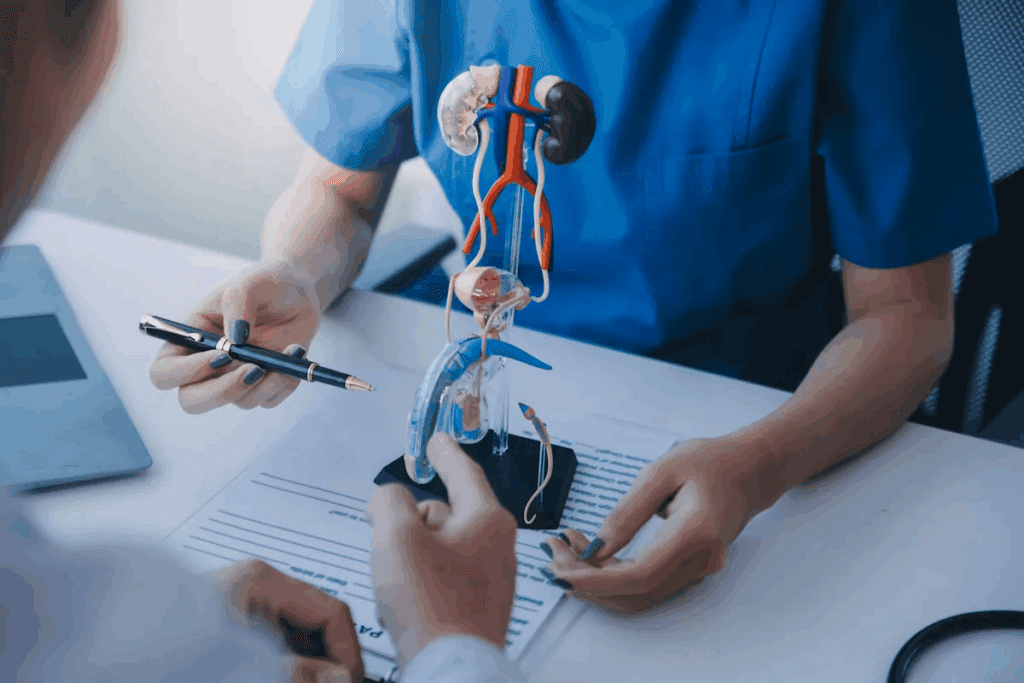
There are many prostate surgeries, each for different reasons. Doctors pick the right surgery based on the patient’s health and the prostate problem. This choice depends on the patient’s condition and overall health.
Radical Prostatectomy
Radical prostatectomy means removing the prostate gland. It’s often chosen for patients with early prostate cancer. This surgery can be done in several ways, including open, laparoscopic, or robotic-assisted.
Transurethral Resection of the Prostate (TURP)
TURP helps with an enlarged prostate. It removes parts of the prostate that block urine. It’s a common treatment for severe BPH symptoms.
Laser Prostatectomy
Laser prostatectomy uses lasers to remove extra prostate tissue. It’s less invasive than TURP. This means less bleeding and shorter hospital stays.
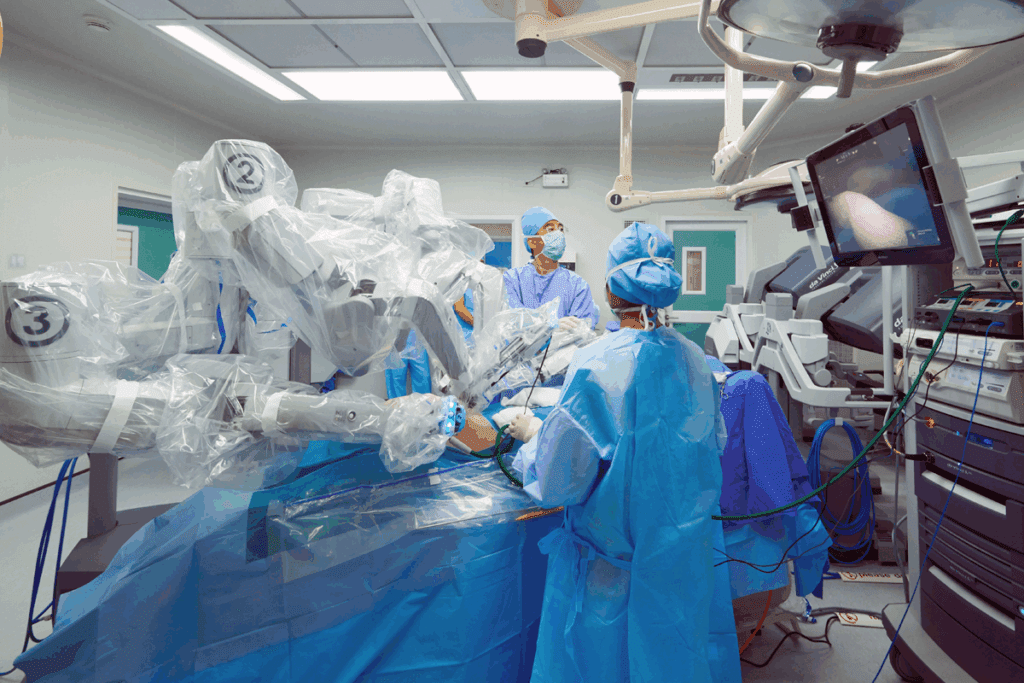
Robotic-Assisted Laparoscopic Prostatectomy
This surgery is a minimally invasive method. It uses a robotic system to help the surgeon. It offers better precision and a quicker recovery.
The following table compares these prostate surgical procedures:
| Procedure | Indications | Benefits |
| Radical Prostatectomy | Localized prostate cancer | Potential cure for prostate cancer |
| TURP | Benign prostatic hyperplasia (BPH) | Relief from urinary obstruction |
| Laser Prostatectomy | BPH, prostate enlargement | Minimally invasive, less bleeding |
| Robotic-Assisted Laparoscopic Prostatectomy | Prostate cancer | Precision, less recovery time |
Risks and Complications of Prostate Surgery
It’s crucial to understand the risks associated with prostate surgery and the available treatment options for subsequent urinary incontinence.
Short-term Complications
Short-term issues after prostate surgery include infection, bleeding, and reactions to anesthesia. These problems are usually handled in the hospital or right after you go home.
| Complication | Description | Management |
| Infection | Bacterial infection at the surgical site or urinary tract | Antibiotics |
| Bleeding | Excessive bleeding during or after surgery | Transfusion, surgical intervention |
| Anesthesia Reaction | Adverse reaction to anesthesia | Monitoring, adjustment of anesthesia |
Long-term Complications
Long-term issues can greatly affect your quality of life. These include urinary incontinence, erectile dysfunction, and urethral stricture.
Stress Incontinence as a Major Complication
Stress incontinence is a big problem after prostate surgery. It’s when you leak urine when you exert yourself. This happens because of damage to the urinary sphincter or its nerves during surgery.
How common stress incontinence is varies. But it’s a known risk of prostate surgery. Knowing this helps patients make better choices about their treatment.
Understanding Stress Incontinence After Prostate Surgery
It’s important to understand stress incontinence after prostate surgery to manage its effects. This condition makes you leak urine when you exert yourself or cough. Many men face this issue after prostate surgery.
Definition and Causes of Post-Prostatectomy Incontinence
Post-prostatectomy incontinence (PPI) is when you lose bladder control after prostate surgery. Several factors can cause PPI, like damage to the sphincter muscles or nerve damage. The integrity of the urethral sphincter mechanism is key for continence.
‘The most common cause of incontinence after radical prostatectomy is damage to the external urethral sphincter'”. Knowing these causes helps in finding the right treatments.
Prevalence and Impact on Quality of Life
Many men experience stress incontinence after prostate surgery. This condition can greatly affect their quality of life. It impacts not just physical comfort but also emotional and social well-being.
A study showed that
“Men with post-prostatectomy incontinence experience significant distress and impairment in their quality of life, underscoring the need for effective management strategies.”
So, treating stress incontinence is key to improving these patients’ lives.
Differences Between Male and Female Stress Incontinence
Stress incontinence affects both men and women, but the reasons and impacts are different. In men, it’s often due to prostate surgery. In women, it’s often caused by childbirth, menopause, or pelvic floor disorders. The anatomy and physiology of continence mechanisms also vary by gender, affecting treatment approaches.
Male stress incontinence, after prostate surgery, needs a specific management plan. This plan should focus on the condition’s causes and severity. Healthcare providers must understand these differences to provide the right care.
Stress Incontinence Treatment Options Overview
It’s crucial to understand the risks associated with prostate surgery and the available treatment options for subsequent urinary incontinence.
Conservative vs. Surgical Approaches
Conservative treatments are often the first step. They include pelvic floor exercises, lifestyle changes, and behavioral adjustments. Surgical options are for more severe cases or when other treatments don’t work well.
Conservative management aims to reduce symptoms without surgery. This can include pelvic floor rehabilitation, diet changes, and bladder training. The goal is to better control the bladder and reduce leaks.
Timeline for Treatment After Prostate Surgery
When to start treatment after prostate surgery is key. Doctors usually wait a bit to see if the body heals on its own. This waiting time can vary, but most say to start treatment if leaks last more than 6-12 months after surgery.
Factors Affecting Treatment Selection
Many things decide the best treatment for stress incontinence. These include how bad the symptoms are, the patient’s health, past treatments, and what they prefer. Other urinary symptoms or health issues also play a role.
Healthcare providers need to understand these factors. This helps them create treatment plans that fit each patient’s needs. This approach improves outcomes and quality of life.
Pelvic Floor Exercises for Stress Incontinence Treatment
Stress urinary incontinence can significantly impact one’s daily activities and overall quality of life.
How Kegel Exercises Work for Men
Kegel exercises make the pelvic floor muscles stronger. These muscles help hold the bladder and urethra in place. By making these muscles stronger, men can better control when they urinate. This helps reduce stress incontinence.
Proper Technique and Frequency
To do Kegel exercises right, men need to find their pelvic floor muscles. They can do this by stopping the flow of urine while they pee. Then, they contract these muscles for 5-10 seconds and relax for the same amount of time. Do this 10-15 times, 3 times a day.
“Kegel exercises are a simple yet effective way to manage stress incontinence. By incorporating them into your daily routine, you can significantly improve your bladder control.”
Effectiveness and Expected Results
Kegel exercises work differently for everyone. But, with regular practice, most men see better bladder control. Studies show that men who do Kegel exercises well can cut down on stress incontinence episodes.
| Duration of Kegel Exercises | Expected Improvement in Stress Incontinence |
| 1-3 months | Noticeable improvement in bladder control |
| 3-6 months | Significant reduction in stress incontinence episodes |
| 6 months and beyond | Optimal bladder control with continued practice |
In conclusion, pelvic floor exercises are a great option for men with stress incontinence after prostate surgery. Knowing the right way to do them and practicing regularly can greatly improve a man’s life.
Behavioral and Lifestyle Modifications
Managing stress incontinence needs a mix of changes in behavior and lifestyle. These adjustments can help control symptoms and enhance life quality.
Bladder Training Techniques
Bladder training helps improve bladder control by gradually increasing time between bathroom visits. It’s a behavioral method to reduce incontinence episodes. Start by keeping a diary to track when you urinate and when you leak.
For instance, if you usually go every hour, try to wait 15 minutes longer each time. Consistency and patience are key for bladder training success.
Dietary Considerations
Diet is key in managing stress incontinence. Some foods and drinks can irritate the bladder, making symptoms worse. Caffeine and alcohol are known irritants that can increase urine production.
Avoiding these substances can help. Eating a balanced diet to maintain a healthy weight also reduces bladder pressure. A diet high in fiber helps prevent constipation, which can also cause incontinence.
Physical Activity Guidelines
Regular exercise is vital for health and managing stress incontinence. Exercises like Kegel exercises strengthen the pelvic floor muscles. But, it’s also important to stay active to keep a healthy weight and reduce bladder pressure.
Try to do at least 30 minutes of moderate exercise daily. Walking, swimming, or cycling are good choices. Avoid high-impact activities that can strain the pelvic floor.
Medical Treatments for Stress Incontinence
Men who have had prostate surgery and now have stress incontinence have several treatment options. Stress incontinence is when you leak urine when you exert yourself or cough. It can make everyday activities hard and affect your mood.
Medications for Male Stress Incontinence
There are no drugs just for stress incontinence in men. But, some medicines can help. Alpha-blockers relax muscles in the prostate and bladder neck, making it easier to pee. But, they don’t work for everyone.
Antidepressants like imipramine can also help. They work by affecting the bladder muscle and the urethral sphincter. Even though they’re not made for this, they can help manage symptoms.
Effectiveness and Side Effects
How well these medicines work can differ a lot from person to person. It’s important to talk to a doctor about the good and bad sides. Alpha-blockers can cause dizziness, headaches, and tiredness. Antidepressants might lead to dry mouth, constipation, and feeling sleepy.
- Monitoring Side Effects: It’s key to watch for side effects and tell your doctor.
- Adjusting Dosage: Doctors might change the dose or switch medicines based on how you react and any side effects.
Combination Therapy Approaches
For the best results, using more than one treatment is often suggested. This can include medicines, pelvic floor exercises, and changes in your daily routine. These might include bladder training and eating certain foods.
Working with a team of doctors, physical therapists, and other experts can help a lot. They create a plan that fits your needs and helps you get better.
- Pelvic floor physical therapy to strengthen the muscles around the bladder and urethra.
- Making lifestyle changes to lessen symptoms and improve bladder control.
- Using medicines and possibly surgery for more serious cases.
Surgical Options for Post-Prostatectomy Stress Incontinence Treatment
Surgical options for stress incontinence after prostate surgery offer new hope for men. These procedures are designed to address the specific needs of individuals experiencing urinary incontinence following prostatectomy.
Male Slings and Their Types
Male slings are a surgical option for treating stress urinary incontinence. They provide additional support to the urethra, helping to prevent involuntary leakage.
- Types of Male Slings:
- Fixed slings, which are positioned under the urethra and attached to the pelvic bone.
- Adjustable slings, which allow for post-operative adjustments to achieve optimal continence.
Both types have shown effectiveness in managing stress incontinence. The choice between them depends on individual patient factors.
Artificial Urinary Sphincter Implantation
The artificial urinary sphincter (AUS) is a device implanted to manage severe stress urinary incontinence. It consists of a cuff placed around the urethra, a pump, and a balloon reservoir.
Key Benefits:
- High success rate in achieving continence.
- Ability to control urination manually.
AUS implantation is considered for men with significant incontinence. It is for those who have not responded to other treatments.
Bulking Agents and Newer Techniques
Bulking agents involve injecting material around the urethra to improve its coaptive ability. This reduces incontinence.
- Advantages: Minimally invasive procedure.
- Limitations: May require multiple injections; effectiveness can vary.
Newer techniques continue to evolve. They offer promising alternatives for managing post-prostatectomy stress incontinence.
Recovery Process After Prostate Surgery
Knowing what to expect after prostate surgery is key. The recovery time is important for getting back to health and dealing with any issues that might come up.
Immediate Post-Operative Period
The first few days to weeks after surgery are the immediate recovery phase. During this time, doctors watch for any problems and give advice on how to care for yourself.
Important things to do in the immediate post-operative period include:
- Rest and avoid hard activities
- Use medicine to manage pain
- Watch for signs of infection or other issues
- Follow your doctor’s advice for catheter care, if needed
Long-term Recovery Timeline
The recovery doesn’t stop after the first few weeks. It can take months to feel fully back to normal.
Here’s a general idea of what to expect in the long-term recovery timeline:
| Timeframe | Recovery Milestones |
| 1-3 months | Start to do light activities, see improvement in bladder control |
| 3-6 months | Can do more physical things, bladder control keeps getting better |
| 6-12 months | Most people see big improvements, including better sex life and bladder control |
Managing Incontinence During Recovery
Dealing with incontinence is a big part of getting better. Doing pelvic floor exercises, like Kegels, can help control your bladder. Doctors might also suggest changes in how you live and behave to help with incontinence.
Here are some ways to manage incontinence:
- Do pelvic floor exercises often
- Use products to catch leaks
- Avoid foods and drinks that bother your bladder
- Keep a healthy weight to ease pressure on your bladder
By understanding the recovery and using good strategies for incontinence, patients can have a better outcome and quality of life after prostate surgery.
Preventing Stress Incontinence Before and After Prostate Surgery
To prevent stress incontinence, a mix of pre-surgery training, new surgery methods, and post-surgery care is key. Knowing and using these steps can greatly lower the chance of incontinence after prostate surgery.
Pre-Surgical Pelvic Floor Training
Before surgery, training the pelvic floor is very important. This training makes the muscles around the bladder stronger. Kegel exercises are a top choice for this.
- Find the right muscles: These are the ones that stop urine flow.
- Do Kegel exercises often: Squeeze for 5-10 seconds, then relax. Do this 10-15 times, three times a day.
- Watch your progress: Keep an eye on how strong your muscles get.
Surgical Techniques to Minimize Incontinence Risk
New surgery methods have cut down incontinence risks a lot. Surgeons use nerve-sparing techniques to keep nerves around the prostate intact. These nerves help control urine flow.
- Robotic-assisted laparoscopic prostatectomy is more precise and causes less damage.
- Nerve-sparing surgery helps keep urine control.
- Less invasive methods speed up recovery and lower risks.
Post-Surgical Care Strategies
Good care after surgery is key to avoiding incontinence. Patients should follow their doctor’s advice closely. This may include:
- Keep doing pelvic floor exercises to keep muscles strong.
- Manage pain well to help healing and comfort.
- Go to follow-up visits to check on healing and talk about any issues.
By combining pre-surgery training, new surgery methods, and good care after surgery, patients can greatly lower their risk of incontinence after prostate surgery.
Psychological Impact and Coping Strategies
Stress incontinence after prostate surgery can cause a lot of emotional pain. It affects daily life and overall happiness.
Emotional and Social Challenges
Feeling embarrassed, anxious, or depressed is common. These feelings can hurt not just the person but also their loved ones. Going out and doing things can become hard, making life feel lonely and less fulfilling.
Emotional challenges can show up in many ways. This includes mood swings, being easily upset, and losing confidence. It’s important to recognize these feelings and find help.
Support Systems and Resources
A strong support system is key to dealing with stress incontinence’s emotional side. This includes family, friends, support groups, and doctors. Support groups, whether in person or online, are great for sharing stories and learning from others.
- Family and friends can offer emotional support and help with daily tasks.
- Support groups provide a community and understanding.
- Healthcare professionals can offer guidance on managing incontinence and related psychological issues.
Communication with Partners and Healthcare Providers
Talking openly with partners and doctors is very important. Sharing the emotional and physical struggles of stress incontinence can help find solutions and strengthen bonds. Doctors can give specific advice and treatment plans to handle incontinence and its emotional side.
Good communication leads to better support and understanding. This can greatly improve the patient’s life quality.
Advances in Prostate Surgery to Reduce Incontinence Risk
Prostate surgery has seen big changes, with new methods to lower incontinence risk. These new ways of treating prostate issues have cut down on incontinence cases.
Nerve-Sparing Techniques
Nerve-sparing techniques are a big step forward in prostate surgery. They aim to keep nerves around the prostate that help with bladder control and sex. This helps lower the chance of incontinence after surgery and speeds up recovery.
Using these techniques needs a lot of skill and knowledge of the prostate’s layout. Research shows they help patients avoid stress incontinence.
Minimally Invasive Approaches
Minimally invasive surgeries, like laparoscopic and robotic-assisted ones, are gaining popularity. They use smaller cuts, cause less damage, and hurt nerves and muscles less. This means patients heal faster and feel less pain after surgery.
Robotic prostatectomy, in particular, offers better precision and control. This helps surgeons do complex tasks more accurately. It also lowers the chance of complications, including stress incontinence.
Future Directions in Surgical Innovation
The future of prostate surgery looks bright with new tech and techniques. New materials and devices are being developed to help with nerve-sparing and reduce damage.
There’s also research into using artificial intelligence and machine learning in surgery. This could make prostate surgery even more precise and successful.
| Technique | Description | Benefits |
| Nerve-Sparing Techniques | Preserves nerves surrounding the prostate | Reduced risk of incontinence, improved erectile function |
| Minimally Invasive Approaches | Smaller incisions, less tissue damage | Quicker recovery, less post-operative pain |
| Robotic Prostatectomy | Enhanced precision and control | Improved accuracy, reduced complications |
When to Seek Specialized Stress Incontinence Treatment
Knowing when to get help for stress incontinence can greatly improve your life. After prostate surgery, men may face different levels of incontinence. It’s important to know when to look for specialized treatment.
Warning Signs and Symptoms
Spotting the signs of stress incontinence is the first step. Look out for:
- Frequent leakage of urine during physical activities or coughing
- Persistent dribbling of urine
- Need to wear absorbent pads or adult diapers consistently
- Significant impact on daily activities and social interactions due to incontinence
If you notice these symptoms, see a healthcare provider. Early treatment can greatly improve your outcome.
Finding the Right Specialist
Finding a specialist in stress incontinence is key. Start by asking your primary care doctor for a referral to a urologist or a continence specialist. Also, ask for recommendations from support groups or online forums.
Questions to Ask Your Healthcare Provider
When talking to your healthcare provider about stress incontinence, prepare your questions. Some important ones are:
- What are the most effective treatment options for my specific condition?
- What are the possible risks and benefits of each treatment?
- Are there any lifestyle changes or conservative management strategies I can try before surgery?
- What is the expected recovery time for the recommended treatment?
By asking these questions, you can make a well-informed decision. This ensures you get the best treatment for your stress incontinence.
Conclusion
Prostate surgery is a big deal, and knowing the risks is key. Stress incontinence is a common problem after this surgery. Luckily, there are many ways to treat it.
Understanding why and how often men face this issue helps them find the right treatment. There are many options, from exercises to surgery. These can really help improve life quality.
It’s crucial to understand the risks associated with prostate surgery and the available treatment options for subsequent urinary incontinence.
FAQ
What is stress incontinence?
Stress incontinence is when moving or pressure on the bladder makes you leak urine. It’s a common issue after prostate surgery.
What are the causes of stress incontinence after prostate surgery?
Damage to the muscles or nerves that control the bladder during surgery often causes it. This damage can happen during prostate surgery.
How common is stress incontinence after prostate surgery?
About 30% of men might experience some incontinence after prostate surgery. The exact number can vary.
What are the treatment options for stress incontinence?
Treatments include pelvic floor exercises, lifestyle changes, and medical treatments. Surgery like male slings and artificial sphincter implants are also options.
How effective are Kegel exercises in treating stress incontinence?
Kegel exercises can help by strengthening the pelvic floor muscles. But, doing them correctly and often is key to success.
What are the benefits of bladder training techniques?
Bladder training can improve bladder control. It helps by gradually increasing the time between needing to urinate.
Are there any medications available for treating stress incontinence?
There are no approved medications for stress incontinence. But, some medications might be used off-label. Combination therapies can also be effective.
What are the surgical options for treating stress incontinence after prostate surgery?
Surgical options include male slings, artificial urinary sphincter implants, and bulking agents. These can help manage incontinence after prostate surgery.
How long does it take to recover from prostate surgery?
Recovery time varies, but most men take weeks to months to fully recover. During this time, incontinence symptoms may improve.
Can stress incontinence be prevented before or after prostate surgery?
Yes, pre-surgical training, certain surgical techniques, and post-surgical care can reduce incontinence risk. These strategies can help minimize symptoms.
What are the warning signs that indicate the need for specialized stress incontinence treatment?
If you have persistent or severe incontinence, or if it’s affecting your quality of life, you might need specialized treatment. Failure to improve with conservative measures is also a warning sign.
How can I find the right specialist for stress incontinence treatment?
Look for referrals from your healthcare provider. Research specialists experienced in treating stress incontinence. Ask about their approach and experience.
What questions should I ask my healthcare provider about stress incontinence treatment?
Ask about the cause of your incontinence, treatment options, risks, and benefits. Also, ask about expected outcomes.
Reference
- Averbeck, M. A. (2024). Surgery for post-prostatectomy urinary incontinence. International Journal of Surgery, 65, 120-127. https://www.sciencedirect.com/science/article/pii/S2772973724001589