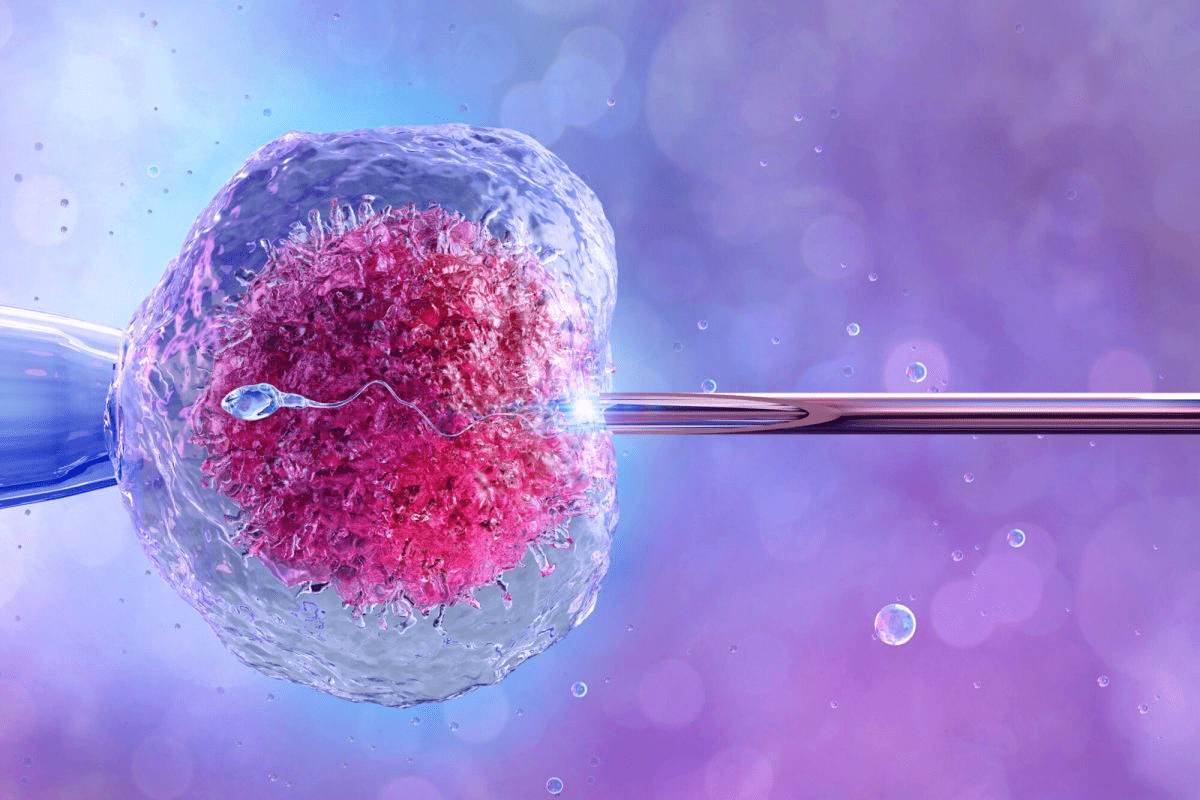
Data breakdown of success rates with chromosomally normal embryos after PGT-A testing. Understanding embryo grading is key for those going through IVF. It’s a tool that checks embryo quality to guess how well they might implant and lead to pregnancy success.
At Liv Hospital, we use top-notch embryo grading systems to see how good embryos are. Studies show that embryos with the best grades have much better chances of leading to a pregnancy success.
Our fertility experts use detailed grading systems to look at things like how much the embryo grows, the quality of its inner cells, and its outer layer. This careful look helps us tailor care to each person and boost IVF outcomes.
Key Takeaways
- Embryo grading is a key factor in IVF success.
- Embryos with the best grades have higher pregnancy rates.
- Comprehensive grading systems check many factors to predict IVF results.
- Liv Hospital’s fertility specialists use advanced grading methods to tailor care.
- Knowing about embryo grading can help set realistic hopes and make the IVF journey better.
The Fundamentals of Embryo Grading in IVF

Learning about embryo grading is key for those going through IVF. It affects the chances of a successful pregnancy. This process looks at cell number, symmetry, and fragmentation at different stages.
What is Embryo Grading?
Embryo grading checks how well embryos can grow and implant. It looks at their shape and structure.
The Gardner grading system is a common way to check blastocyst embryos. It looks at three things: how expanded the embryo is, the quality of the Inner Cell Mass (ICM), and the Trophectoderm (TE). These help see how well the embryo can develop.
Why Grading Matters for IVF Success
The grade of an embryo is a big factor in IVF success. Better-grade embryos are more likely to implant and lead to a live birth. Knowing about grading helps make better choices about which embryos to use.
Limitations of Current Grading Methods
Even though grading is helpful, it has its downsides. It can be hard to agree on what an embryo looks like. Also, it doesn’t consider genetic issues that might affect an embryo’s health.
Understanding embryo grading helps patients get a better grasp of their IVF journey. It shows what can affect its success.
The Gardner Blastocyst Grading System Explained

In IVF, the Gardner blastocyst grading system is key for checking embryo health. It helps judge the quality of blastocysts, which are embryos at about 5 days old.
Expansion Stage (1-6 Scale)
The Gardner system rates the blastocyst’s expansion from 1 to 6. This is important because it shows how ready the blastocyst is to implant. A score of 1 means the blastocyst is just starting, with a small cavity. A score of 6 shows a fully expanded blastocyst, ready to hatch.
The expansion stage shows how well the embryo might develop. Scores from 3 to 6 are usually good for transfer, with higher scores linked to better implantation chances.
Inner Cell Mass (ICM) Quality (A-C)
The Inner Cell Mass (ICM) is another key part of the Gardner grading. The ICM is rated from A to C, with A being the best, showing a tight group of many cells. C means a loose, sparse group with fewer cells.
The ICM’s quality is linked to the embryo’s implantation and growth chances. A high-quality ICM (A) is linked to better IVF success, showing a strong group of cells for the fetus.
Trophectoderm (TE) Quality (A-C)
The Trophectoderm (TE) is the outer layer of the blastocyst, forming the placenta and other tissues. The TE is graded from A to C, with A being the best, showing a cohesive layer with many cells.
The TE’s quality is vital for implantation and placenta development. A well-developed TE (A or B) is key for successful implantation, helping with nutrient and waste exchange.
Day 5 Embryo Grading and Success Rates
Day 5 embryo grading is key in IVF success. It shows how well an embryo can develop. On day 5, embryos that have grown into blastocysts are checked for quality and readiness for transfer.
What Makes a “Perfect” Blastocyst
A “perfect” blastocyst has grown well, with a strong inner cell mass (ICM) and trophectoderm (TE). The Gardner blastocyst grading system is used to judge these features. A top blastocyst has a high growth score, a dense ICM, and a TE with many cells.
Research shows that grade AA embryos have the best pregnancy success rates. Higher grades mean better IVF success rates.
Understanding Combined Grades (5AA, 4AB, etc.)
Combined grades give a full view of a blastocyst’s quality. The first number shows its growth stage. Then, the ICM and TE grades follow. For example, a 5AA embryo is fully grown with excellent ICM and TE, showing great implantation chances.
Knowing these grades helps doctors and patients decide on embryo transfer.
Blastocyst Success Rates by Grade
Blastocyst success rates change with their grade. Here’s a table showing success rates for different grades:
| Blastocyst Grade | Success Rate |
|---|---|
| 5AA | 63-65% |
| 4AA | 55-60% |
| 4AB | 45-50% |
| 3AA | 40-45% |
Higher-grade blastocysts have much better success rates. For example, a 4AA embryo has a very high success rate. This shows how important grading is.
Top-Quality Embryos: AA Grade Success Rates
IVF success depends a lot on embryo quality. The best embryos, graded as AA, have a much higher chance of leading to a successful pregnancy. Studies show that AA embryos have significantly higher success rates in IVF treatments.
AA embryos are considered the best because they are morphologically ideal. They have a higher chance of implanting and leading to pregnancy. The grading system looks at factors like expansion stage, inner cell mass quality, and trophectoderm quality.
5AA Embryo Success Rates (63-65%)
A 5AA embryo is of the highest quality, with a success rate of 63% to 65% per single transfer. This is because it has reached the optimal expansion stage and has high-quality inner cell mass and trophectoderm. This makes 5AA embryos very desirable for transfer.
4AA Embryo Success Rate
A 4AA embryo is not fully expanded but has high-quality inner cell mass and trophectoderm. Its success rate is a bit lower than 5AA embryos but is very promising. Research shows that 4AA embryos can have significant success rates, though figures can vary based on patient age and health.
6AA Embryo Success Rate
A 6AA embryo is a fully expanded blastocyst with excellent inner cell mass and trophectoderm quality. While there’s less data on 6AA embryos, they are generally seen as having high success rates. Their fully expanded state is often linked to a higher implantation chance.
In summary, AA grade embryos have much higher success rates in IVF treatments. Knowing about embryo grading and success rates helps patients and fertility specialists make better decisions about embryo transfer.
Good Quality Embryos and Their Outcomes
Embryo grading is key in IVF treatment. Good quality embryos have success rates that help guide patient choices. These embryos are graded based on criteria, showing their chance for successful implantation and pregnancy.
Studies show that embryos graded 6AA, 5AA, 5AB, 4AA, 4AB, 3AA, and 3AB have a 46.8% live birth rate. This highlights the importance of embryo grading in IVF success.
5AB Embryo Success Rate
A 5AB embryo is of high quality. It has reached the blastocyst stage and has a high inner cell mass (ICM) and trophectoderm (TE) quality. The success rate for 5AB embryos is generally good.
Research shows that 5AB embryos have a pregnancy rate similar to 5AA embryos. The difference in TE quality between “A” and “B” does not greatly affect success rates.
4AB Embryo Success Patterns
4AB embryos are also of good quality. They have a lower expansion grade than 5AB but high ICM and TE quality. Success rates for 4AB embryos are positive but slightly lower than 5AB.
Success rates for 4AB embryos depend on patient age and sperm quality.
3AA and 3AB Embryo Outcomes
3AA and 3AB embryos are of good quality, with “3” indicating an early blastocyst stage. “AA” grading means high quality for both ICM and TE, while “AB” means high ICM quality and good TE quality.
Outcomes for these embryos vary. 3AA embryos generally have a better prognosis than 3AB due to higher grading. Both are viable for transfer.
| Embryo Grade | Success Rate (%) | Live Birth Rate (%) |
|---|---|---|
| 5AB | 55-60 | 45-50 |
| 4AB | 50-55 | 40-45 |
| 3AA | 45-50 | 35-40 |
| 3AB | 40-45 | 30-35 |
Knowing the success rates of different embryo grades helps patients and clinicians make informed IVF decisions. While outcomes vary, the data offer a general guideline.
Fair to Poor Quality Embryos: Grade B and C Success Rates
Fair to poor quality embryos, graded B or C, face unique challenges in IVF. While top-quality embryos are preferred, many people in IVF may have lower-grade embryos. Knowing the success rates of these embryos helps in making treatment decisions.
Grade B Embryo Success Rates
Grade B embryos are of fair quality and have a good chance of leading to a successful pregnancy. Studies show that embryos graded 6BB, 5BB, 4BB, and 3BB have live birth rates of about 39.0%. This means they are a viable option for those undergoing IVF, even if their success rates are lower than top-quality embryos.
Every person’s situation is different. Deciding to transfer a Grade B embryo should be discussed with a fertility specialist. Health, sperm quality, and uterine receptivity all affect the success of the transfer.
Grade C Embryo Success Rate
Grade C embryos are of poor quality and have lower success rates than Grade A and B embryos. Research indicates that Grade C embryos have live birth rates of around 34.1%. Though lower, some individuals may achieve a successful pregnancy with a Grade C embryo.
Embryo grading is just one factor in IVF success. We work with our patients to consider all factors and create a personalized treatment plan.
When Lower-Grade Embryos Are Worth Transferring
In some cases, transferring lower-grade embryos might be the best choice. For those with few embryos, transferring a lower-grade embryo may be better than another cycle of egg retrieval. For individuals with specific circumstances, the benefits of transferring a lower-grade embryo might outweigh the risks.
Talking about the risks and outcomes with a fertility specialist is key. Understanding Grade B and C embryo success rates and individual circumstances helps patients make informed choices for their IVF journey.
Expanded Blastocyst Success Rates
The growth stage of a blastocyst is a key sign of its readiness for implantation. In the world of IVF, knowing about blastocyst growth is key to predicting success.
What Makes a Blastocyst “Expanded”
An expanded blastocyst has grown to a certain size. It has a bigger cavity and a thinner outer layer. This growth is important for implantation, as it lets the blastocyst attach to the uterine lining better.
Key characteristics of an expanded blastocyst include:
- A larger blastocoel cavity
- A thinner zona pellucida
- An inner cell mass (ICM) that is more defined
- A trophectoderm (TE) layer that is more prominent
Grades 5-6: Fully Expanded Blastocysts
Fully expanded blastocysts, grades 5 or 6, have a high chance of implanting. They have a big cavity and a very thin outer layer.
Studies show that fully expanded blastocysts do better in IVF. A study found that:
“The implantation rate for fully expanded blastocysts (grades 5-6) was significantly higher compared to less expanded blastocysts.”
Correlation Between Expansion and Implantation
The more a blastocyst expands, the better it can implant. This is because it has more contact with the uterine lining.
The correlation can be summarized as follows:
- Higher expansion grades are associated with higher implantation rates.
- Fully expanded blastocysts have a better chance of successful implantation.
- The thinning of the zona pellucida facilitates hatching and implantation.
Understanding blastocyst growth and its link to implantation success helps us make better choices in IVF. This can lead to higher success rates.
Success Rates with Chromosomally Normal Embryos
The success of IVF treatments depends a lot on the quality of the embryos. Chromosomally normal embryos have a better chance of implanting and leading to pregnancy. We will look into how PGT-A testing checks embryo quality and its impact on IVF success.
PGT-A Testing and Embryo Quality
PGT-A testing is a key tool in IVF. It checks if embryos have the right number of chromosomes before transfer. “PGT-A testing has greatly improved choosing embryos for transfer,” says Medical Expert, a top fertility expert.
It helps pick the best embryo for transfer, boosting the chance of a successful pregnancy. This is very important for those who have had miscarriages or failed IVF cycles.
How Chromosomal Normality Affects Outcomes
Chromosomal normality is key for IVF success. Normal embryos have a much better chance of implanting and leading to a healthy pregnancy. Studies show that transferring a single normal embryo can lead to high success rates, sometimes better than transferring many embryos without PGT-A testing.
PGT-A testing improves IVF success by lowering the risk of transferring abnormal embryos. This is a common reason for implantation failure and miscarriage. By only transferring normal embryos, we can greatly increase the chance of a successful pregnancy.
Combined Factors: Grade + Genetic Testing
PGT-A testing checks for chromosomal normality, while embryo grading looks at the embryo’s physical quality. Together, they give a full picture of an embryo’s success chances. “Combining PGT-A testing with traditional grading has greatly improved our ability to predict IVF success,” says Medical Expert, a well-known embryologist.
By looking at both the chromosomal normality and physical grade of an embryo, we can make better choices for transfer. This approach has been shown to increase IVF success rates and lower miscarriage risk.
Day 3 Embryo Grading and Success Rates
Grading embryos on day 3 is key to knowing if IVF will work. At this stage, embryos are in the cleavage stage. Their quality is judged by several important factors.
Cell Number and Symmetry Assessment
One main factor is the number of cells, or blastomeres. Studies show that embryos with a certain cell count on day 3 do better. For example, embryos with 8 cells are usually of higher quality.
Symmetry is also very important. Embryos with cells of even size and shape get a higher grade. Those with uneven or broken cells are graded lower.
“The number and symmetry of cells in a day 3 embryo are critical indicators of its potential for successful implantation and development,” say fertility experts.
Fragmentation Evaluation
Fragmentation is when there are small, irregular cell parts in the embryo. Too much fragmentation can hurt the embryo’s quality and IVF success. Embryos with little fragmentation are seen as having a better chance.
Day 3 vs. Day 5 Transfer Success Comparison
Choosing to transfer embryos on day 3 or day 5 is a big decision. Each option has its own success rates. Research compares these rates to help patients decide what’s best for them.
A study in a top fertility journal found,
“The success rates of day 3 and day 5 embryo transfers vary, with some patients achieving better outcomes with one stage over the other.”
We keep up with new research to give the latest info to IVF patients.
Embryo Grading and Gender Correlation
Embryo grading is key in IVF success. But, its link to embryo gender is unclear. As we explore assisted reproduction, knowing if embryo quality affects gender is vital for both patients and doctors.
Is There a Link Between Grade and Gender?
There’s a lot of talk about if embryo grade affects gender. Some studies hint at a connection, while others say the proof is lacking. We’ll look into the research to clarify this.
4AB Embryo: Boy or Girl Tendencies
The 4AB embryo is a focus of interest. Research on it has raised questions about gender tendencies. But, the findings are not clear-cut. The 4AB embryo is seen as high quality, but its gender leanings are under study.
Scientific Evidence and Limitations
Some studies suggest a link between embryo traits and gender. Yet, scientists are cautious. The current evidence is not strong enough to say gender can be predicted by embryo grade. More research is needed to grasp any possible connection.
| Embryo Grade | Potential Gender Tendency | Scientific Evidence Strength |
|---|---|---|
| 4AB | Uncertain | Limited |
| 5AA | No clear tendency | Moderate |
| 3BB | Speculative | Weak |
Transfer Decisions: Embryo Grading and Success Rates
Embryo grading is key in IVF treatment. It helps decide if to transfer one or more embryos. It also decides if to use fresh or frozen embryos.
Single vs. Multiple Embryo Transfer
Choosing between single or multiple embryo transfers is a big decision in IVF. Studies show single embryo transfers can work as well as multiple ones. This reduces the chance of having twins or more.
Single Embryo Transfer (SET) is best for those with a good chance of success. It lowers the risk of having twins or more. But, the choice depends on age, embryo quality, and past IVF results.
Fresh vs. Frozen Transfer Considerations
Deciding between fresh or frozen embryo transfers is also important. Fresh embryo transfers happen right after egg retrieval. Frozen embryo transfers (FET) thaw embryos that were frozen before.
The choice between fresh and frozen transfers depends on several factors. These include how well the ovaries respond, the risk of OHSS, and how well the uterus is ready to receive the embryo.
Working with Your Fertility Specialist
Deciding on embryo transfer should be done with a fertility specialist. They offer advice tailored to your situation, medical history, and goals.
By teaming up with a fertility specialist, you can make choices that boost your chances of a successful IVF.
Conclusion: Beyond Grading in IVF Success
Embryo grading is key in IVF, but success comes from many angles. We know a full approach to IVF care is vital for the best results.
Research shows that patient health, the skill of the fertility specialist, and a complete treatment plan matter a lot. We look at more than just grading. We also consider things like chromosomal health, how well the embryo grows, and what each patient needs.
By taking a full view of IVF care, we can meet each patient’s unique needs. This mix of advanced grading and personalized care boosts the chances of a successful IVF cycle.
At our clinics, we team up with patients to craft custom treatment plans. We aim to offer top-notch healthcare and support. This way, we help those trying to start a family through IVF get the best start.
FAQ
What is embryo grading, and why is it important for IVF success?
Embryo grading is a way to check the quality and health of embryos during IVF. It looks at how developed the embryo is, the number of cells, and how well it’s formed. This helps doctors pick the best embryo for transfer, which can lead to a successful pregnancy.
How are blastocysts graded using the Gardner blastocyst grading system?
The Gardner system grades blastocysts by three things: how expanded they are (1-6), the quality of the inner cell mass (ICM) (A-C), and the quality of the trophectoderm (TE) (A-C). For example, a 5AA blastocyst is fully expanded with high-quality ICM and TE.
What is a “perfect” blastocyst, and what are its success rates?
A “perfect” blastocyst is a high-quality embryo, like a 5AA or 4AA. These embryos have a high success rate, often between 60-65% for 5AA embryos.
How do success rates vary for different embryo grades?
Success rates change a lot based on the embryo grade. Top-grade embryos like 5AA and 4AA have better success rates than lower grades like 3BC or 2BC. Generally, higher grades mean better outcomes.
Are there any differences in success rates between day 3 and day 5 embryo transfers?
Day 5 (blastocyst-stage) transfers often have higher success rates than day 3 transfers. This is because they allow for better selection of viable embryos.
Does the grade of the embryo influence the gender of the baby?
There’s no scientific proof that the embryo grade affects the baby’s gender. Embryo grading looks at physical traits, not genetic sex.
What is the success rate of grade B embryos compared to grade A?
Grade B embryos usually have lower success rates than grade A embryos. But, success rates can vary based on the patient’s age and the grading system used.
How does PGT-A testing impact embryo grading and success rates?
PGT-A testing checks if embryos have the right number of chromosomes. When used with morphological grading, it helps pick the best embryos. This can improve success rates.
Can lower-grade embryos also result in successful pregnancies?
Yes, even lower-grade embryos can lead to successful pregnancies. While they have lower success rates, favorable factors can sometimes make a lower-grade embryo successful.
How do fertility specialists decide on single versus multiple embryo transfers?
Deciding between single or multiple embryo transfers depends on many factors. These include the patient’s age, embryo quality, and past IVF results. Specialists work with patients to choose the best option.
What is the significance of expanded blastocysts in IVF success?
Expanded blastocysts (grades 5-6) have a higher chance of implanting. The degree of expansion is key in judging an embryo’s viability.
Are there any scenarios where transferring a grade C embryo is considered?
Transferring a grade C embryo might be considered when there are few embryo options. Or when other factors suggest a chance of success despite the lower grade.
References
National Center for Biotechnology Information. Evidence-Based Medical Guidance. Retrieved from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5987494/)