Last Updated on October 31, 2025 by

TURBT and the Role of Suprapubic Catheterization in Bladder Surgery
Bladder surgery is key to treating many bladder issues, such as cancer and incontinence. One of the most common procedures is Transurethral Resection of Bladder Tumor (TURBT).
TURBT is mainly used for treating bladder cancer that hasn’t spread deeply. It allows doctors to remove tumors through the urethra, helping both diagnose and treat the cancer. Often, after TURBT, doctors may recommend additional treatments like BCG therapy to reduce the risk of recurrence.
In many cases, patients may need temporary bladder drainage after surgery. This is where suprapubic catheterization can play a role. Instead of placing a catheter through the urethra, a small opening is made in the lower abdomen to allow urine to drain directly from the bladder. Doctors sometimes prefer suprapubic catheterization for TURBT patients because it can reduce urethral irritation and improve comfort during recovery.
Early detection and treatment of bladder cancer are vital, as they lead to much better survival rates. With advancements in medical technology and supportive methods such as suprapubic catheterization, patient care and surgical safety continue to improve.
In the U.S., many people need surgery for bladder issues every year. Over 84,000 new bladder cancer cases were reported in 2025. This shows we need good surgery options.
Bladder problems that need surgery include bladder cancer and severe incontinence. Bladder cancer is a big reason for surgery, with more cases in recent years. Other issues like bladder blockage and neurogenic bladder also need surgery.
“More bladder cancer and other problems mean more surgeries,” says a top urologist.
There are many ways to fix bladder problems, like radical reconstruction and ileal conduit urinary diversion. Radical reconstruction removes and rebuilds the bladder. Ileal conduit makes a new way for urine to leave the body.
Choosing the right surgery depends on the problem, how bad it is, and the patient’s health. For example, ileal conduit is used when a lot of the bladder must be removed because of cancer.

It’s important for doctors and patients to know about all surgery options. Learning about the latest in bladder surgery helps improve care and life quality.
TURBT is seen as the top choice for diagnosing and treating non-muscle-invasive bladder cancer. This method removes bladder tumors, helping with both diagnosis and treatment.
The TURBT procedure is done under anesthesia to keep patients comfortable. A special tool called a resectoscope is used to see the tumor in the bladder. Then, the tumor is removed from the bladder wall.
This tissue is checked to find out the cancer’s stage and grade.
The TURBT procedure has several key steps:
TURBT is the top choice for treating non-muscle-invasive bladder cancer. It’s effective and safe. The procedure removes visible tumors, which is key for diagnosis and treatment.
By removing the tumor, we can accurately stage the cancer. This helps plan further treatments, like intravesical therapies.
The benefits of TURBT include:
Understanding TURBT and its benefits helps patients and healthcare providers make informed decisions. We keep TURBT as a key part of treating non-muscle-invasive bladder cancer. This ensures the best results for our patients.
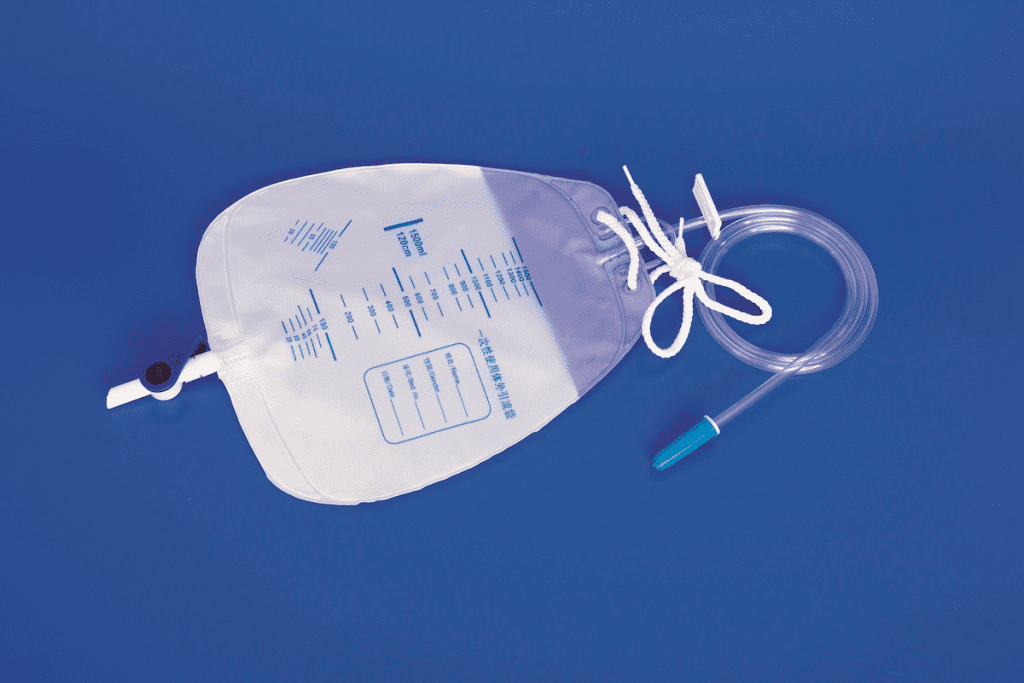
Suprapubic catheterization is used when patients have trouble with urine flow. It’s done to drain urine from the bladder through the abdomen. This method is used when other ways don’t work.
This procedure is for those who can’t use a regular catheter. Reasons include urinary retention, urethral stricture, or enlarged prostate. It’s also for patients with neurogenic bladder or urethral trauma.
Doctors decide on a case-by-case basis. They consider the patient’s health, the reason for the issue, and if they can handle the catheter.
The steps for suprapubic catheterization are:
Proper care and maintenance of the suprapubic catheter are key to avoiding problems like infections or blockages.
In females, suprapubic catheterization is often better due to the shorter urethra. This might lower the risk of some complications. But it’s important to think about the unique challenges and anatomical differences.
We make sure female patients get care tailored to their needs. We address any concerns they have about the procedure and managing the catheter.
For those dealing with complex bladder issues, knowing about radical reconstruction and cystectomy is key. These surgeries are often for advanced bladder cancer or severe conditions.
Cystectomy, or removing the bladder, is a big treatment for bladder problems. There are two main types: partial and radical.
Choosing between partial and radical cystectomy depends on many things. These include cancer stage and location, patient health, and personal wishes.
After a cystectomy, patients need a way to manage urine flow. The ileal conduit urinary diversion is a common method.
Ileal Conduit Procedure: It makes a conduit from the intestine (ileum) and connects it to the ureters. This lets urine drain through a stoma into a bag.
The ileal conduit is a tried and true method for urinary diversion. But, it needs careful post-op care and stoma management.
Knowing about such a big surgery can be scary. Our team is here to offer full support and guidance. We aim to ensure patients get the best care possible.
Minimally invasive bladder surgeries are changing how we treat bladder issues. They aim to cause less harm to the patient while keeping treatment effective. Thanks to new medical tech, surgeons can now do complex surgeries with more precision and fewer problems.
Endoscopic procedures are key in minimally invasive bladder surgery. They use a thin, flexible tube with a camera and light. This lets surgeons see inside the bladder without open surgery.
Endoscopy helps diagnose and treat bladder issues without open surgery. A study on NCBI shows these procedures are getting better, helping patients more.
One big plus of endoscopic procedures is that they can be done outside the hospital. This lowers healthcare costs and cuts down on infection risks.
Laser treatment is a top choice for bladder issues like tumors. Laser therapy can remove or destroy diseased tissue while keeping healthy tissue safe. This method is precise, reducing risks and helping patients heal faster.
“Laser treatment for bladder conditions has revolutionized the field of urology, providing a minimally invasive solution with great results.”
Robotic-assisted surgery is the latest in minimally invasive techniques. It uses robotic tools to improve the surgeon’s skills and view. Robotic-assisted bladder surgery leads to less blood loss, less pain, and quicker recovery than traditional surgery.
As urology advances, so will the use of minimally invasive surgeries, like robotic-assisted ones. This change improves patient care and shows a move towards more caring and effective healthcare.
Surgical treatments for urinary incontinence have improved a lot. They offer new hope to people all over the world. We will look at the different surgeries, like sling procedures and bladder neck suspension. We will talk about how well they work and any possible problems.
Sling procedures help by placing a supportive sling under the urethra. This method is very effective for many, mainly those with stress urinary incontinence. The sling can be made from synthetic mesh or biological tissue. It’s usually put in place through a small incision.
These procedures work well because they give extra support to the urethra. Studies show most patients see better control of their bladder after the surgery.
Bladder neck suspension is used for urinary incontinence when the bladder neck needs support. This surgery suspends the bladder neck to better its position and cut down on leaks. The Burch colposuspension is a common method, but laparoscopic or robotic-assisted surgery is gaining popularity.
The aim of this surgery is to fix the anatomy and function of the bladder. It works well, but success can vary based on the case and the surgeon’s skill.
Recovering after surgery is key to treating urinary incontinence. Patients need close follow-up to make sure they’re healing properly and their bladder control is getting better. Nerve regeneration is very important, as it helps after surgeries that might damage nerves, like prostate surgery.
To speed up nerve recovery after prostate surgery, several things can help. These include physical therapy, eating right, and not smoking. Scientists are also working on new ways to help nerves heal faster.
In summary, surgeries for urinary incontinence offer many effective choices for patients. By knowing about sling procedures and bladder neck suspension, patients can make better choices. Recovery, including nerve healing, is a big part of the treatment.
It’s important to know about the risks of bladder surgery. This knowledge helps keep patients safe and ensures a smooth recovery. While these surgeries are usually safe, there are risks that both patients and doctors should be aware of.
Patients may face several challenges after bladder surgery. These can include:
Following post-operative instructions carefully is key. Proper wound care and sticking to medication regimens are critical.
It’s important to spot complications early. Patients should watch for signs like:
Prompt communication with healthcare providers is key to addressing these issues effectively.
Recovery from bladder surgery requires proper care and lifestyle changes. Strategies include:
As one study noted, “The road to recovery is just as important as the surgery itself.”
“Effective recovery strategies can significantly impact the outcome of bladder surgery, improving both short-term and long-term results.”
Understanding complications and using recovery strategies can greatly improve outcomes. We stress the importance of patient education and proactive care in managing risks and achieving successful results.
Medical technology and surgery have made big strides in bladder surgery. We’ve looked at procedures like TURBT, Suprapubic Catheterization, and Radical Cystectomy. We’ve talked about when they’re used, their benefits, and possible risks.
At Liv Hospital, we’re all about top-notch healthcare. We use the newest bladder surgery methods. Our skilled urologists and team work hard to help our patients get better and live better lives.
The future of bladder surgery is bright. There’s a lot of research on new, less invasive ways to do surgery. We’re committed to keeping up with these advances. This way, we can offer our patients the best care possible.
TURBT, or Transurethral Resection of Bladder Tumor, is a surgery for bladder cancer. It’s the top choice because it removes tumors from the bladder wall. This method is very accurate and works well for non-muscle-invasive bladder cancer.
Suprapubic catheterization is a procedure to drain urine through the abdomen. It’s used when someone can’t pee normally. This could be due to urinary retention, obstruction, or neurological issues.
Partial cystectomy removes just the bladder part with the tumor. Radical cystectomy takes out the whole bladder, nearby tissues, and sometimes organs. The choice depends on the cancer’s size and location.
Ileal conduit urinary diversion uses the intestine for urine flow. It’s done after removing the bladder. The ureters are connected to the conduit, and it’s brought to the abdomen, creating a stoma.
Minimally invasive surgeries, like endoscopic and robotic-assisted, have big advantages. They use smaller cuts, cause less pain, and lead to shorter hospital stays. Recovery is also faster than with open surgery.
Supporting nerve regeneration after prostate surgery includes physical therapy and medication. Lifestyle changes also help. It’s key to follow your doctor’s specific advice for the best recovery.
After bladder surgery, common issues are pain, infection, and urinary problems. Managing these includes proper wound care and pain meds. Regular check-ups with your doctor are also important.
Complications like infection, bleeding, and leakage can happen. Watch for fever, severe pain, or unusual discharge. If you see these signs, get medical help right away.
To recover well, follow your doctor’s advice and live healthily. Manage pain, prevent infection, and slowly get back to normal activities. Regular follow-ups are also key.
Early bladder cancer diagnosis is very important. It boosts survival chances and reduces the need for harsh treatments. Regular check-ups and screenings are vital for early detection.
Subscribe to our e-newsletter to stay informed about the latest innovations in the world of health and exclusive offers!