Last Updated on December 2, 2025 by Bilal Hasdemir
Bladder surgery is a key treatment for many bladder issues. The transurethral resection of bladder tumor (TURBT) is the most common surgery done worldwide.

TURBT is the main surgery for bladder cancer in its early stages. Studies show that over 70% of early bladder cancer surgeries use TURBT. This is because it’s less invasive and patients recover quickly.What is the most common type of bladder surgery? Learn why suprapubic catheterization is frequently used and what it involves.
TURBT removes bladder tumors effectively, reducing complications. As we explore bladder surgery, TURBT’s benefits and success rate are clear. It’s a top choice for patients because of its effectiveness and patient benefits.
Key Takeaways
- TURBT is the most common surgical procedure for bladder cancer.
- Over 70% of early-stage bladder cancer surgeries use TURBT.
- TURBT is valued for its minimally invasive approach.
- Rapid recovery is a significant benefit of TURBT.
- TURBT involves the resection of bladder tumors.
Understanding Bladder Surgery and Its Indications
Bladder surgery treats conditions like bladder cancer and urinary tract disorders. It’s key to know the common reasons for surgery.
Common Conditions Requiring Surgical Intervention
Bladder cancer is a top reason for bladder surgery. Transurethral Resection of Bladder Tumor (TURBT) is used for diagnosis and treatment. Other issues, like bladder stones and incontinence, may also need surgery.
For advanced bladder cancer or damage, radical reconstruction is used. This includes ileal conduit urinary diversion or conduit urinary diversion. These surgeries change how urine leaves the body.
Pre-Surgical Evaluation and Diagnostic Procedures
Before surgery, patients get a detailed check-up. This includes imaging tests like CT scans and biopsies to confirm the disease.
A thorough pre-surgery evaluation is vital. It prepares patients and reduces risks. A team of healthcare experts works together to create a treatment plan.
- Imaging tests (CT scans, MRI, ultrasound)
- Biopsies for disease confirmation
- Assessment of overall patient health
Knowing why bladder surgery is needed and the tests involved helps patients. It lets them make informed decisions about their care.
Transurethral Resection of Bladder Tumor (TURBT): The Gold Standard
TURBT is seen as the top choice for diagnosing and treating bladder tumors. It’s both effective and safe. This procedure has changed how we manage bladder cancer, giving patients a good treatment option.
Step-by-Step TURBT Procedure
The TURBT process has several important steps. First, the patient gets anesthesia to avoid pain. Then, we put a resectoscope through the urethra to see the tumor in the bladder.
We use the resectoscope to resect the tumor carefully. This makes sure all tumor tissue is taken out. The removed tissue is checked to learn about the tumor’s type and size.
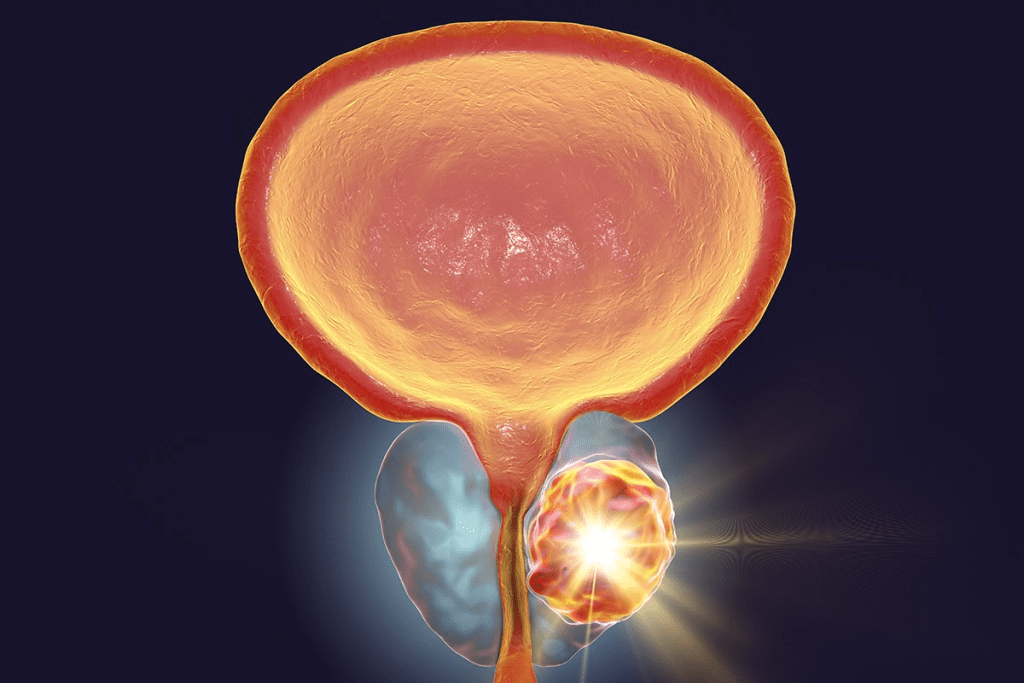
Why TURBT is the Preferred Bladder Surgery
TURBT is the top choice because it’s less invasive. This means less harm to the patient compared to bigger surgeries. It also leads to faster healing.
Studies show TURBT works well for bladder cancer. This makes it a favorite among doctors.
Recovery and Follow-Up Care
Patients usually recover quickly after TURBT. Most go home within a day or two. We stress the need for follow-up care to watch for any signs of the tumor coming back.
We guide patients on how to recover. This includes advice on post-operative care and when to come back for check-ups. Even though TURBT is the main focus, knowing about other treatments for bladder cancer helps with patient care.
Alternative Bladder Cancer Surgeries
There are other surgeries for bladder cancer beyond the usual treatments. Transurethral Resection of Bladder Tumor (TURBT) is common. But other surgeries might be needed based on the cancer’s stage and the patient’s health.
Radical Cystectomy for Muscle-Invasive Cancer
Radical cystectomy is often suggested for muscle-invasive bladder cancer. This surgery removes the bladder, lymph nodes, and sometimes other organs. Men might lose the prostate and seminal vesicles, while women could lose the uterus, ovaries, and part of the vagina.
The surgery aims to remove all cancer, aiming for a cure or better prognosis. It’s a big surgery with big life changes.
Partial Cystectomy: When and Why
In some cases, a partial cystectomy is done. This means only the tumor part of the bladder is removed. It’s less common for patients to have a single tumor and no cancer elsewhere in the bladder.
This surgery tries to keep more bladder function, avoiding the need for urinary diversion. But it’s important to decide on a case-by-case basis.
Ileal Conduit and Other Urinary Diversions
After a radical cystectomy, a new way to handle urine is needed. An ileal conduit is often used. It’s made from a part of the intestine. Other options include continent cutaneous reservoirs and orthotopic neobladders.
The choice depends on the patient’s health, cancer extent, and personal wishes. We help patients choose the best option, explaining the pros and cons of each.
Knowing about bladder cancer surgery options is key to treatment decisions. We aim to give full care and support, ensuring the best results for our patients.
Suprapubic Catheterization: Applications and Techniques
Suprapubic catheterization is a good choice for long-term urine drainage. It’s different from the usual way of putting in a catheter. This method goes through the belly to get urine from the bladder.
The Procedure and Its Benefits
The process is done under local anesthesia or sedation. A small cut is made in the lower belly. Then, the catheter goes into the bladder.
This method has fewer risks of damage to the urethra. It also might lead to fewer infections in the urinary tract.
It’s easier to manage for patients, like women, because it doesn’t go through the urethra. This is great for people with certain body issues or who have trouble with the usual catheter method.
Comparing Suprapubic and Urethral Catheterization
Urethral catheterization is more common and seems simple. But it’s not right for everyone, like those with urethral strictures.
Suprapubic catheterization is a gentler option for some. It depends on the patient’s health, why they need a catheter, and how long they’ll need it.
- Suprapubic catheterization is for long-term needs.
- It’s for those who can’t use the usual catheter.
- A healthcare professional does it in a clean place.
In summary, suprapubic catheterization is a key method for dealing with urine issues. Knowing its uses, benefits, and differences with urethral catheterization helps doctors choose the best option for their patients.
Advancements in Bladder Surgery Technology
New technologies are changing bladder surgery for the better. They make surgeries more effective and improve how patients feel. This is great news for people all over the world.
Robotic-Assisted Surgical Approaches
Robotic surgery is a big step forward in bladder surgery. It lets the surgeon do detailed work with less harm to the body. Research shows it can make recovery faster and reduce problems.
One great thing about robotic surgery is the clear, 3D view it gives. This helps the surgeon see and work on the area better.
Minimally Invasive Techniques and Patient Outcomes
Less invasive surgeries, like laparoscopic and robotic, are gaining favor. They have smaller cuts, less pain, and quicker healing. This is good for patients.
- Less chance of problems
- Shorter hospital stays
- Quicker to get back to daily life
These methods make surgeries better and improve life quality for patients.
Emerging Treatments and Clinical Trials
Bladder surgery is always getting better, thanks to new treatments and trials. We’re seeing new robots, better imaging, and new ways to operate.
“The future of bladder surgery lies in the continued development and refinement of minimally invasive techniques, coupled with advancements in technology,” says a leading urologist.
As we keep learning and improving, we’ll see even better treatments. This will make bladder surgeries safer and more effective, helping patients live better lives.
Conclusion
Bladder surgery is a key treatment for many bladder issues, including cancer. We’ve looked at the different surgeries, focusing on the TURBT procedure. It’s a common and effective way to treat bladder tumors.
The TURBT procedure removes bladder tumors, helping both diagnose and treat them. It’s important because it takes out tumors without harming the bladder. Knowing about TURBT and other surgeries like radical cystectomy and partial cystectomy helps patients make better choices.
New techniques in bladder surgery, like robotic-assisted and minimally invasive methods, have made things better. These advancements mean less recovery time and fewer complications. This makes surgery a good option for more people. As we keep improving in urology, treating vejiga conditions will get even better.
Understanding the different bladder surgery options helps patients on their treatment path. We suggest talking to your doctor about your needs and condition. This way, you can find the best surgery for you.
FAQ
What is TURBT, and why is it considered the gold standard for bladder cancer treatment?
TURBT stands for Transurethral Resection of Bladder Tumor. It’s a surgery to diagnose and treat bladder cancer. It’s the top choice because it removes tumors well, lowers risks, and shortens hospital stays.
What are the benefits of robotic-assisted surgery for bladder cancer?
Robotic-assisted surgery brings many benefits. It offers better precision, less blood loss, and quicker healing. This method lets surgeons do complex tasks with high accuracy and less invasion.
How does suprapubic catheterization differ from urethral catheterization?
Suprapubic catheterization goes through the abdomen to the bladder. Urethral catheterization goes through the urethra. Suprapubic is safer for long-term use because it has fewer risks.
What is an ileal conduit urinary diversion, and when is it necessary?
An ileal conduit urinary diversion is a surgery to create a new urine path after removing the bladder. It’s needed for patients having a radical cystectomy for muscle-invasive bladder cancer.
How can I speed up nerve regeneration after prostate surgery?
Nerve recovery after prostate surgery takes time. But you can help it along. Stay healthy, do physical therapy, and follow your doctor’s advice.
What are the risks associated with radical reconstruction after bladder removal?
Radical reconstruction, like ileal conduit, has risks. These include urinary diversion problems, infections, and metabolic changes. But, these can be managed with proper care and follow-up.
What is the difference between a female catheter and a standard catheter?
Female catheters are made for women, considering their anatomy. They are shorter and more curved than regular catheters. This makes them more comfortable and easier to use.
Can I expect a full recovery after TURBT surgery?
Yes, most people fully recover from TURBT surgery with little trouble. Just follow your doctor’s instructions and go to all follow-up appointments for a smooth recovery.
What are the latest advancements in bladder surgery technology?
New advancements in bladder surgery include robotic-assisted surgery, minimally invasive methods, and treatments like immunotherapy and targeted therapy. These advancements are improving care and outcomes for patients.
References
- Kim, J. K., et al. (2020). Recent trends in transurethral surgeries and urological procedures in Korea: A nationwide population-based study. Investigative and Clinical Urology, 61(3), 303“312. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7521963/
- Mariappan, P., & Singh, P. (2021). Transurethral resection of bladder tumour (TURBT)”getting the basics right in bladder cancer management. BJU International, 128(4), 391“400. https://pubmed.ncbi.nlm.nih.gov/33802016/
- Babjuk, M., et al. (2019). EAU Guidelines on Non-Muscle-Invasive Bladder Cancer (Ta, T1, and CIS). European Urology, 76(5), 639“657. https://pubmed.ncbi.nlm.nih.gov/31576313/
- Brucker, B. M., et al. (2020). Robotic-assisted radical cystectomy: An overview. Current Opinion in Urology, 30(5), 790“796. https://pubmed.ncbi.nlm.nih.gov/32887410/