Last Updated on November 24, 2025 by
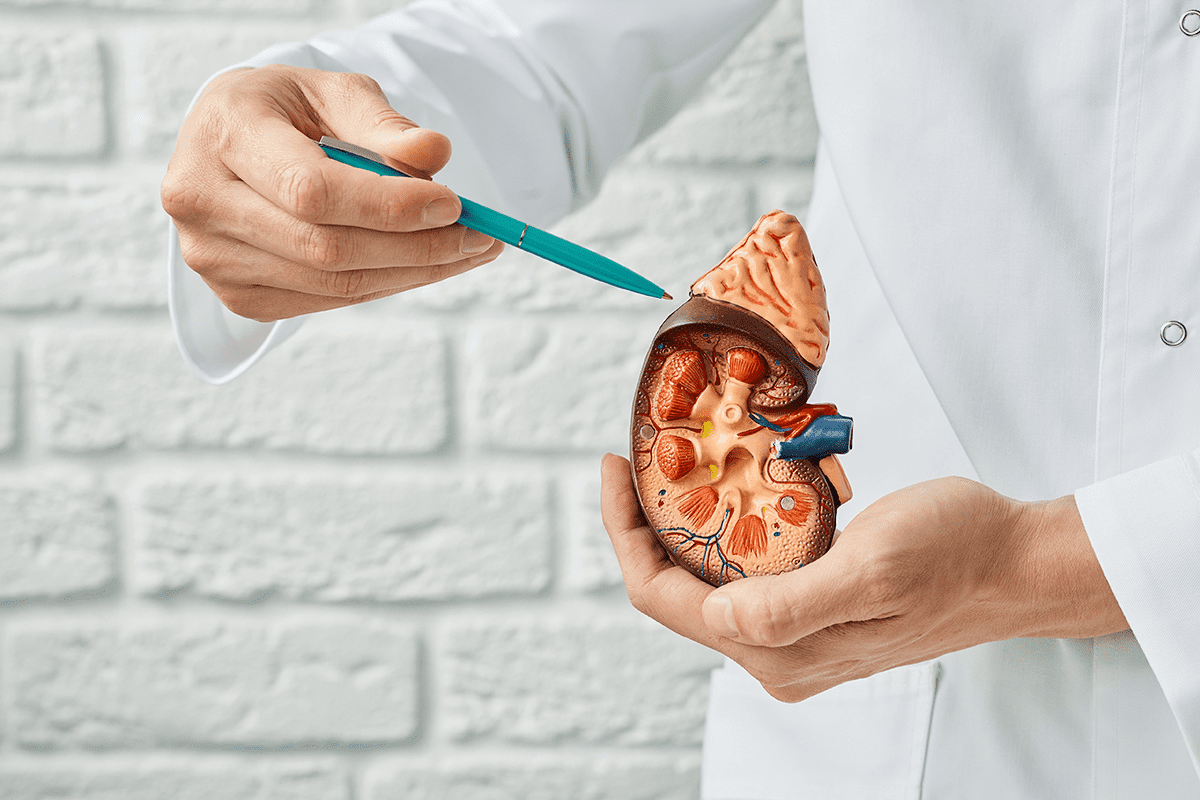
Urology surgery includes many procedures, like prostate cancer surgery and surgical correction for hypospadias. The success of these surgeries depends on the surgeon’s skill, the technology used, and the patient’s health.
New technologies, such as robotic-assisted surgery, have greatly improved results. For example, robotic-assisted prostate cancer surgery has a 95% success rate. This shows how technology boosts the success of urology surgeries.
Looking into the success rates of different urology surgeries is key. We need to know what affects these rates and how they help patients. We’ll see how places like Liv Hospital are setting new standards globally.
Key Takeaways
- Urology surgery success rates vary based on the procedure and factors like surgeon skill and technology used.
- Robotic-assisted prostate cancer surgery has a high success rate of 95%.
- Advancements in technology have improved patient outcomes in urology surgery.
- The skill of the surgeon and patient health are key factors in urology surgery success rates.
- Hospitals with advanced technology and multidisciplinary care are setting new standards in urology surgery.
Understanding Success Rates in Modern Urological Procedures
Looking at how well urological surgeries work gives us important information. It shows how good they are and where they can get better. Many things affect how well a surgery goes, like the skill of the doctors, the tools used, and the patient’s health.
Key Factors Influencing Surgical Outcomes
Several important factors shape the results of urological surgeries. Surgeon expertise is key, as more experienced doctors usually get better results. The type of urological procedure also matters; for example, the success of hypospadias surgery depends on the type of hypospadias and the surgery method.
Advanced medical technology has changed urological surgeries for the better. It makes surgeries more precise and cuts down on recovery time. Robotic-assisted surgery, for instance, has improved results in surgeries like prostate cancer treatment.
How Medical Centers Measure and Report Success
Medical centers use different ways to check how well urological surgeries do. They look at complication rates, recovery times, and patient satisfaction. This helps them see how well their treatments work and find ways to get better.
For example, success in hypospadias surgery is often judged by how many complications happen and if more surgery is needed. By knowing these details, we can understand the challenges in making urological surgeries successful.
Robotic-Assisted Prostate Cancer Surgery: 95% Success Rate
Robotic-assisted prostate cancer surgery has a 95% success rate. It’s changing how we treat prostate cancer. This method makes treatment more precise and improves patient results.
Robotic surgery has cut down on complications by 40%. This is thanks to the advanced technology. It gives surgeons better control and vision, leading to more accurate surgery.
Reduced Complications with Advanced Technology
Robotic technology has made a big difference in prostate cancer surgery. It makes the surgery less invasive. This leads to fewer complications after surgery.
Also, patients recover 70% faster with robotic surgery. This means they can get back to their daily lives sooner. It shows how minimally invasive the surgery is.
Faster Recovery and Improved Outcomes
Robotic-assisted surgery offers more than just fewer complications. It also means patients recover faster. As we keep improving, we expect even better results for our patients.
Using the latest in robotic technology, we give our patients the best care. The high success rate, fewer complications, and quicker recovery make it a great choice for treatment.
Female Urinary Incontinence Treatment Success Rates
Female urinary incontinence affects many women around the world. There are several treatments available. Thanks to new medical technologies, these treatments are getting better, giving hope to those who suffer.
Two treatments stand out: Transobturator Tape Surgery and Polyacrylamide Hydrogel Injections. We’ll look at how well they work and what they mean for patients.
Transobturator Tape Surgery: A Highly Effective Solution
Transobturator Tape Surgery is a top choice for treating incontinence. It has a success rate of 93.75%. This surgery uses a tape to support the urethra, greatly reducing leaks.
Alternative Approaches: Polyacrylamide Hydrogel Injections
Polyacrylamide Hydrogel Injections are another option, with a success rate of 82.76%. It’s a less invasive method that uses a hydrogel to help the urethra close better, reducing leaks.
Transobturator Tape Surgery is more effective than Polyacrylamide Hydrogel Injections. Yet, both have their uses, depending on the patient’s needs and preferences.
The main benefits of these treatments are:
- High success rates: Both treatments greatly improve symptoms.
- Minimally invasive options: Procedures like Polyacrylamide Hydrogel Injections are less invasive, leading to quicker recovery.
- Improved quality of life: Successful treatment improves patients’ overall well-being.
In summary, both Transobturator Tape Surgery and Polyacrylamide Hydrogel Injections are effective for treating incontinence. Understanding their success rates helps healthcare providers and patients make better choices.
Surgical Correction for Hypospadias: Outcomes and Statistics
It’s important to know the success rates and statistics of hypospadias surgery. This condition, where the urethra’s opening is not at the tip of the penis, affects many male infants. Over the years, surgery for this condition has improved, thanks to new techniques and better care after surgery.
Types of Hypospadias and Their Impact on Success Rates
Hypospadias is divided into types based on where the urethral opening is. The type of hypospadias can affect how well the surgery works. The main types are:
- Distal hypospadias, where the urethral opening is near the tip of the penis
- Midshaft hypospadias, with the opening along the shaft
- Proximal hypospadias, where the opening is closer to the base of the penis
Each type has its own challenges. Distal hypospadias usually has a higher success rate because it’s less complex.
Hypospadias Operation Cost Breakdown in the United States
The cost of hypospadias surgery in the United States varies a lot. It depends on how complex the case is, the surgeon’s fees, and hospital charges. On average, it can cost between $10,000 and $30,000 or more. Insurance and post-operative care costs can also add to the total cost.
Hypospadias Surgery Age Limit: Optimal Timing for Intervention
The best age for hypospadias surgery is a topic of debate. Most surgeons suggest surgery between 6 to 18 months of age. Early surgery can lower the risk of problems and improve results. But, the decision on when to have surgery depends on the child’s health and how severe the condition is.
Choosing to have hypospadias surgery is a big decision. Knowing the outcomes and statistics can help make a better choice. Our team is dedicated to providing top-notch healthcare and support for international patients.
Pediatric Pyeloplasty: Success Rates and Reoperation Statistics
Pediatric pyeloplasty is a successful surgery for kids with ureteropelvic junction obstruction. It fixes the blockage that stops urine from flowing right. Our team has seen great results with this surgery, aiming to give top care to our young patients.
Below International Averages: Reoperation Rate
Our reoperation rate for pediatric pyeloplasty is 3.9%, which is lower than the world average. This shows our surgery’s success and the care we give our patients. A low reoperation rate means our surgeons are skilled and our care is thorough.Our numbers match those of other top medical centers.
Long-term Functional Outcomes
Children who have this surgery usually see big improvements. Many kids have normal kidney function after surgery. We stress the need for long-term follow-ups to catch any issues early.
The main advantages of pediatric pyeloplasty are:
- High Success Rate: The surgery works well, with few need for more operations.
- Minimal Complications: Modern surgery methods reduce risks of problems.
- Improved Kidney Function: Successful surgery can make kidney function better or keep it good.
Choosing a skilled surgical team means your child gets the best care. We keep watching results and improving our methods to ensure top care.
Single-Port Robotic Urological Procedures: The Cutting Edge
Single-port robotic urological procedures are now a leading solution for many urological issues. They use just one incision. This approach reduces visible scars and may shorten recovery times.
Comparable Success with Superior Cosmetic Results
Research shows single-port robotic pyeloplasty is as safe and effective as traditional methods. It also offers better cosmetic results. This is great for those worried about surgical scars.
Recent studies found these procedures are not just effective but also boost patient happiness. The study published in PMC points out the benefits of less scarring and quicker healing.
Reduced Hospital Stays and Patient Recovery Experience
Patients who get single-port robotic surgery often stay in the hospital less. They also have a better recovery. This is because the surgery is less invasive, causing less pain and trauma.
Single-port robotic urological procedures offer many benefits. They combine high success rates with superior cosmetic outcomes. As this technology grows, we’ll see even better care and results for patients.
Conclusion: Advancing Success Rates Through Multidisciplinary Care
Throughout our discussion, we’ve seen how important multidisciplinary care is in urology surgery. By using the latest research and always improving, top hospitals can greatly increase their success rates. This approach helps patients get the best care possible.
Success rates depend on many things, like the surgery type and technology used. But, it’s the teamwork in multidisciplinary care that really makes a difference. It improves patient results and makes the care process smoother. This leads to quicker recoveries and happier patients.
By focusing on teamwork and using the newest urology surgery techniques, we can keep improving success rates. As urology advances, the role of multidisciplinary care will stay key in achieving top results.
FAQ
What is the success rate of robotic-assisted prostate cancer surgery?
Robotic-assisted prostate cancer surgery is very successful, with a 95% success rate. It also reduces complications by 40% compared to older methods.
How does the type of hypospadias affect the success rate of hypospadias surgery?
The type of hypospadias can change how well surgery works. It’s key for doctors to know this to choose the best treatment.
What is the success rate of transobturator tape surgery for female urinary incontinence?
Transobturator tape surgery is very effective, with a success rate of 93.75%. It’s a top choice for treating female urinary incontinence.
What is the reoperation rate for pediatric pyeloplasty?
Pediatric pyeloplasty has a low reoperation rate of 3.9%. This shows the surgery is very successful for kids.
How does single-port robotic urological surgery compare to traditional methods in terms of success rates?
Single-port robotic surgery has success rates similar to older methods. But it offers better looks and shorter hospital stays.
What factors influence the success rate of urology surgeries?
Many things affect urology surgery success. These include the surgery type, technology, surgeon skill, and patient health.
What is the optimal age for hypospadias surgery?
Finding the best age for hypospadias surgery is a debate. Doctors decide based on each child’s needs.
How much does hypospadias surgery cost in the United States?
Hypospadias surgery costs vary in the U.S. Patients should talk to their doctor to get an estimate.
References
Li, P., Yang, Y., Ma, H., Zhao, X., & Gao, Y. (2022). Comparative outcomes of robotic radical prostatectomy: continence recovery, oncologic results, and functional outcomes. PMC / PubMed.