Last Updated on November 25, 2025 by Ugurkan Demir

Cystectomy, or radical cystectomy, is a big surgery for bladder cancer patients. It’s a tough time for those going through it.
At Liv Hospital, we offer top-notch care. We use the latest surgery methods and focus on our patients. Our goal is to give the best healthcare possible.
A complete guide to the surgical removal of the bladder (cystectomy), including the procedure, recovery, and urinary diversion methods.
A cystectomy means taking out some or all of the bladder. It’s mainly for bladder cancer but can also treat other bladder issues.
Cystectomy, or the surgical removal of the bladder, is a big operation. It’s needed for many medical reasons. The surgery can take out part or all of the bladder, based on the problem.
Cystectomy means taking out the urinary bladder. It’s also called bladder cystectomy or bladder removal. Radical cystectomy is when they take out the bladder and some nearby tissues and organs too.
There are two main types of cystectomy: partial and radical.
Procedure Type | Description | Indications |
Partial Cystectomy | Removal of the diseased portion of the bladder | Localized tumors or diseases |
Radical Cystectomy | Removal of the entire bladder and surrounding tissues | Advanced bladder cancer or widespread disease |
It’s important for patients to know about these surgeries. The choice between partial and radical cystectomy depends on the disease, how far it has spread, and the patient’s health.
Bladder cancer is a main reason for removing the bladder through surgery, called cystectomy. The surgery’s type and extent depend on the cancer’s stage and grade, and other factors.
Muscle-invasive bladder cancer means the cancer has gone through the bladder wall’s muscle layer. At this stage, aggressive treatments like radical cystectomy are often needed. This surgery removes the bladder and sometimes nearby tissues and organs.
When non-muscle invasive bladder cancer doesn’t get better with treatments put directly into the bladder, cystectomy might be suggested. This choice is made after a thorough talk with a healthcare provider.
Bladder removal is also needed for other reasons, not just cancer. These include:
The following table summarizes the common reasons for bladder removal:
Condition | Description | Typical Treatment Approach |
Muscle-Invasive Bladder Cancer | Cancer that has invaded the bladder muscle | Radical Cystectomy |
Non-Responsive Non-Muscle Invasive Bladder Cancer | Cancer that hasn’t responded to intravesical therapy | Cystectomy |
Interstitial Cystitis | Condition causing bladder pain and pressure | Cystectomy (in severe cases) |
Knowing why the bladder might need to be removed helps patients and their families make better choices. It’s important to talk about each condition and treatment options with a healthcare provider.
Before a cystectomy, several tests and evaluations are done. These steps are key to figuring out the bladder cancer’s stage and grade. They also check the patient’s overall health.
We run many tests, like blood and urine tests, and imaging scans. These include CT scans or MRI. They help us see how far the cancer has spread and if there are any other issues.
Staging and grading are very important. Staging shows how far the cancer has spread. Grading looks at the cancer cells under a microscope.
Test | Purpose |
CT Scan | Assesses cancer spread and evaluates lymph nodes |
Urine Test | Checks for cancer cells or other abnormalities |
MRI | Provides detailed images of the bladder and surrounding tissues |
We look at the patient’s health, medical history, and test results. This helps us decide if they’re a good candidate for cystectomy. It’s all about making the right treatment choice.
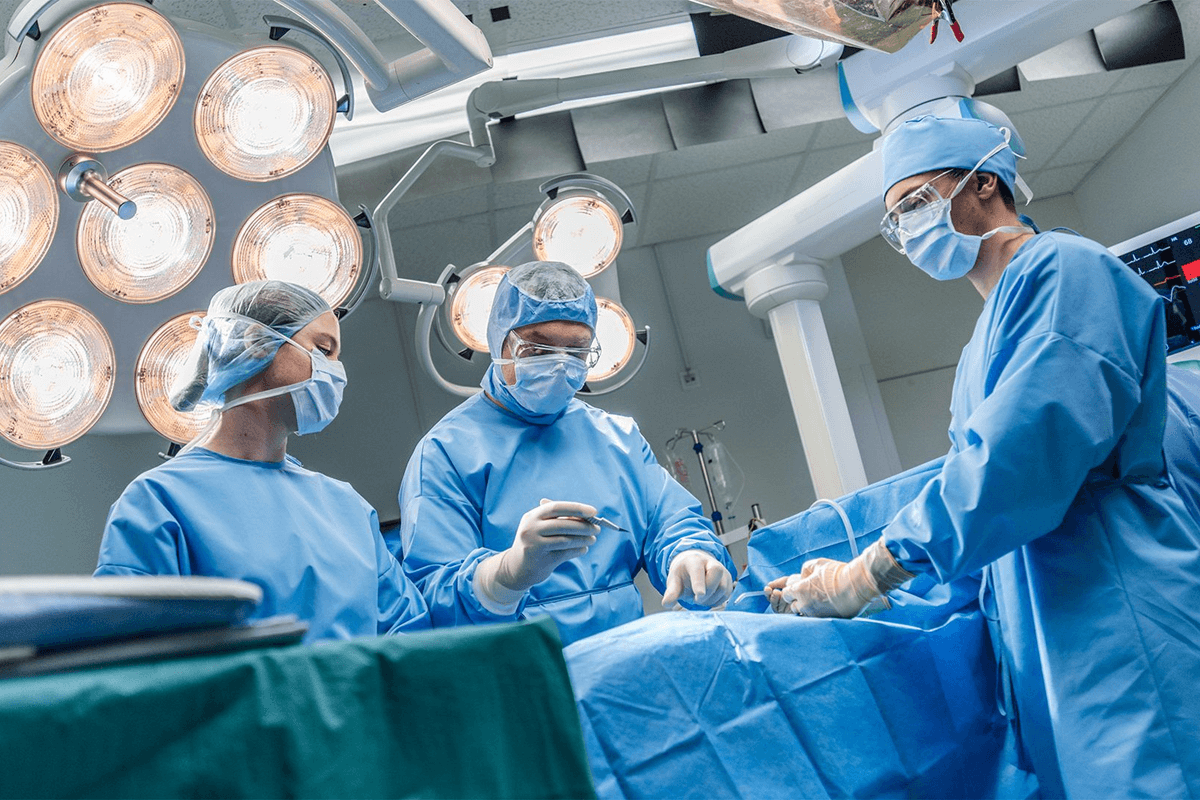
Radical cystectomy is a complex surgery that removes the bladder. It’s mainly done to treat bladder cancer or other bladder issues.
For men, the surgery might also remove the prostate gland. Women might have their uterus, ovaries, or other reproductive organs taken out. The decision to remove these organs depends on the cancer’s extent and the patient’s health.
After surgery, patients must follow a recovery plan. This includes managing pain, attending follow-up appointments, and making lifestyle changes.
The main goal of radical cystectomy is to remove cancer cells and stop the disease from spreading. Though it’s a complex surgery with risks, it’s often a lifesaver for many.
Bladder removal surgery, or cystectomy, uses different methods. Each method has its own benefits and things to think about. The choice depends on the patient’s health, the disease’s extent, and the surgeon’s skills.
We will look at the main surgical techniques for cystectomy. We’ll talk about their key points and advantages.
Open radical cystectomy is a traditional method. It involves one big incision in the abdomen to reach the bladder. This way, the bladder and nearby tissues, plus pelvic lymph nodes, can be removed. This is important for checking the disease’s stage and treating it.
Key aspects of open radical cystectomy include:
Minimally invasive surgery, like laparoscopic and robotic-assisted, offers alternatives to open surgery. These methods use smaller cuts and special tools for the surgery.
Benefits of minimally invasive approaches may include:
When choosing a surgical method for bladder removal, talking to a healthcare provider is key. They can help pick the best method for each person’s situation.
Choosing a surgical approach needs careful thought. It depends on the patient’s health, the disease’s stage, and the benefits and risks of each method.
Patients who have their bladder removed have many choices for how to manage urine. Choosing the right option is key to a good quality of life after surgery. We help patients pick the best choice based on their needs and health.
An ileal conduit is a common choice. It uses a piece of intestine to make a path for urine. This path is then connected to the ureters. The path is brought to the abdomen, where it’s secured to a pouch on the skin.
Key aspects of ileal conduit:
Neobladder reconstruction makes a new bladder from intestine. This new bladder connects to the urethra for natural urination. Not everyone can have this surgery, depending on health and disease extent.
Benefits of neobladder reconstruction include:
A continent urinary reservoir is another option. It creates a pouch inside the body from intestine. Unlike an ileal conduit, it’s not on the skin. Patients use a stoma for catheterization to drain urine.
Considerations for continent urinary reservoir:
Choosing the right urinary diversion is a personal decision. It depends on health, lifestyle, and preferences. We help patients make the best choice for them.
The decision between ileal conduit, neobladder reconstruction, and continent urinary reservoir is important. It should be made after talking with healthcare providers. They can help weigh the benefits and challenges of each option.
Understanding the recovery stages after a cystectomy is key. It includes immediate care, physical therapy, and learning to manage your urinary system. Each step is important for a full recovery.
Your hospital stay is several days long. Your team will watch over you, manage pain, and look for complications. They focus on pain, wound care, and starting your recovery.
Physical therapy is vital for your recovery. It helps you regain strength and mobility. At first, you’ll need to avoid heavy lifting and strenuous activities. These restrictions will be lifted as you get better.
Learning to manage your urinary system is a big part of recovery. This includes caring for your stoma, using a neobladder, or a continent reservoir. Your healthcare team will guide you through this.
Recovery times vary, but most see big improvements in a few months. Here’s what you can expect:
Recovery Stage | Timeline | Milestones |
Immediate Post-Operative | 0-2 weeks | Pain management, initial wound healing |
Early Recovery | 2-6 weeks | Increased mobility, initial physical therapy |
Advanced Recovery | 6-12 weeks | Full mobility, managing urinary diversion |
It’s important to follow your healthcare team’s advice and attend follow-up appointments. Report any concerns or complications right away. With time, patience, and proper care, you can fully recover from a cystectomy.
Knowing the survival rates after a cystectomy is key for patients. These rates vary based on several factors.
Regular follow-ups are essential for monitoring recurrence.
Bladder removal surgery, or cystectomy, is a big deal. It needs careful thought and understanding. We’ve looked at everything from diagnosis to recovery and the need for support.
Recovering from this surgery means following a detailed care plan. This includes regular check-ups and maybe changing your lifestyle. Knowing what to expect helps patients make smart choices about their health.
Thanks to new medical tech, results from bladder removal surgery are getting better. With the right care and support, people can live happy lives after this big surgery.
A cystectomy is a surgery to remove the bladder.
It’s needed to treat bladder cancer or other serious bladder issues.
Risks include infection, bleeding, and damage to nearby organs.
Recovery time varies depending on the individual and the type of procedure, but it can take several weeks to a few months.
Alternatives may include bladder-sparing treatments such as chemotherapy, radiation therapy, or partial cystectomy, depending on the condition and its severity.
A urinary diversion is a surgery that creates a new way for urine to exit the body after the bladder is removed.
Types include ileal conduit, neobladder, and continent urinary reservoir.
An ileal conduit uses a small piece of intestine to divert urine to an external bag, while a neobladder creates a new internal bladder from a section of the intestine, allowing more natural urination.
A cystectomy is performed under general anesthesia. The surgical approach depends on the individual’s health and medical condition—it may be done through open surgery, laparoscopic, or robotic-assisted techniques.
National Center for Biotechnology Information. How to Understand Surgical Removal of the Bladder. Retrieved from https://pmc.ncbi.nlm.nih.gov/articles/PMC4024950/
Subscribe to our e-newsletter to stay informed about the latest innovations in the world of health and exclusive offers!