Last Updated on December 2, 2025 by Bilal Hasdemir
Nearly 30% of patients with a brain tumor choose surgery. It’s a key treatment option.Learn the crucial survival outcomes for brain tumor surgery. Understand how tumor type, grade, and patient age impact prognosis clearly.
Knowing the survival rate for brain tumor surgery is important. A brain tumor diagnosis can be scary. Deciding on surgery is often hard.
We offer a full care plan at our institution. We look at many factors that affect survival outcomes. Our team is committed to top-notch healthcare for all patients, including those from abroad.
Key Takeaways
- Understanding the importance of survival rates for brain tumor surgery
- Factors influencing survival outcomes for brain tumor patients
- Comprehensive care approach for patients undergoing brain tumor surgery
- Our institution’s commitment to delivering world-class healthcare
- Support services available for international patients
Brain Tumors: Classification and Diagnosis

Understanding brain tumors starts with knowing their types and how they are diagnosed. There are two main types: primary and secondary. Each type has its own features and treatment options.
Primary vs. Secondary Brain Tumors
Primary brain tumors start in the brain. Secondary tumors come from cancer spreading to the brain from elsewhere. Primary brain tumors are divided into gliomas, meningiomas, and schwannomas based on their cell type. Knowing if a tumor is primary or secondary helps doctors choose the right treatment.
| Tumor Type | Origin | Common Characteristics |
| Primary | Originates in the brain | Can be benign or malignant, varies in growth rate |
| Secondary (Metastatic) | Spreads to the brain from other parts of the body | Often aggressive, multiple lesions may be present |
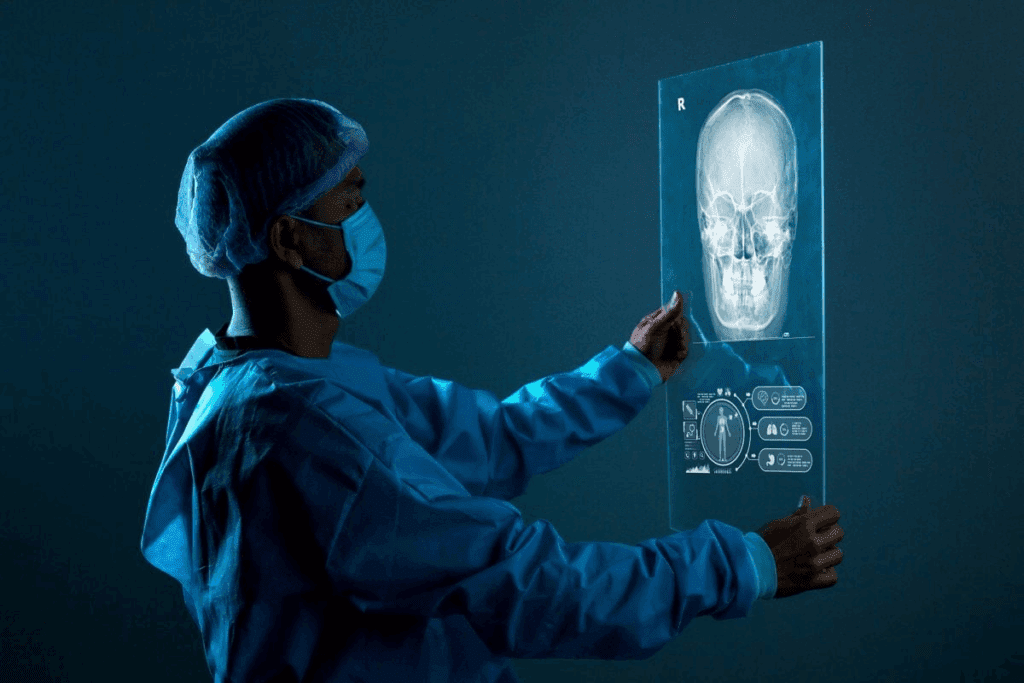
Diagnostic Methods and Staging
Diagnosing brain tumors uses imaging and tissue tests. Magnetic Resonance Imaging (MRI) and Computed Tomography (CT) scans help see the tumor’s size and location. Staging checks how far the tumor has spread, which is key for treatment planning.
We use the latest diagnostic tools for accurate staging. This includes looking at the tumor’s grade and genetic markers. This detailed approach helps us create a treatment plan that fits each patient.
The Role of Biopsy in Prognosis
A biopsy examines tumor tissue to find out its type and grade. This info is key for predicting how the tumor will behave and the patient’s outlook. Biopsy results help decide if surgery, radiation, or chemotherapy is needed.
We see biopsy as very important for planning treatment. It gives us the info we need to make the best treatment plan.
Survival Outcomes for Brain Tumor: Statistical Overview
Looking at survival rates for brain tumor patients shows us trends and areas to improve care. We’ll dive into the data on survival rates, giving insights into treatment and patient results.
Understanding 5-Year Survival Rates
The 5-year survival rate is key for brain tumor patients. It shows the percentage of patients alive 5 years after diagnosis. Studies say about 40% to 50% of patients survive this long. But, survival rates change a lot based on tumor type, grade, and age.
For example, low-grade gliomas have better survival rates than high-grade glioblastomas. Knowing these differences helps doctors create better treatment plans for each patient.
Relative vs. Absolute Survival Rates
It’s important to know the difference between relative and absolute survival rates. Relative survival rate compares brain tumor patients to the general population, adjusting for age and other factors. Absolute survival rate just shows the percentage of patients alive for a certain time.
Relative survival rates give a clearer picture of how brain tumors affect survival. For instance, a relative survival rate of 60% at 5 years means brain tumor patients are 60% as likely to live 5 years as people of the same age in the general population.
Recent Trends in Survival Statistics
New advances in surgery, radiation, and chemotherapy have boosted brain tumor survival rates. Cancer registries show a slow but steady increase in 5-year survival rates over the years.
Studying survival statistics trends helps find what’s working. For example, targeted and immunotherapies are showing promise for some brain tumors. More research and data analysis are needed to keep improving patient care.
Brain Tumor Survival Rates by Type
Survival rates for brain tumors vary a lot. This depends on the tumor type, its features, and the patient’s health. Knowing these differences helps doctors predict outcomes and plan treatments.
Glioblastoma Multiforme (GBM)
Glioblastoma multiforme (GBM) is the most aggressive brain tumor. It’s classified as Grade IV by the World Health Organization (WHO). GBM has a poor prognosis, with a median survival of about 15 months after diagnosis. Despite new treatments, the 5-year survival rate for GBM is only 5-10%. We’ll look at the latest research and treatments for GBM patients.
Meningioma Prognosis
Meningiomas are usually benign tumors from the meninges. The majority of meningiomas grow slowly and can be treated with surgery. Patients with benign meningiomas have a 5-year survival rate over 90%. But, some meningiomas are malignant, and their prognosis is worse.
Astrocytoma Survival Patterns
Astrocytomas are gliomas that vary in grade. The survival for astrocytoma patients depends on the tumor grade. Low-grade astrocytomas have a better prognosis, with 5-year survival rates of 50-70%. High-grade astrocytomas, like glioblastoma, have a poorer prognosis.
Oligodendroglioma and Ependymoma Outcomes
Oligodendrogliomas and ependymomas are less common gliomas. Oligodendrogliomas grow slowly and may have a better prognosis than astrocytomas. Complete surgical resection is key to improving survival for both oligodendroglioma and ependymoma patients.
How Tumor Grade Influences Survival Prognosis
The grade of a brain tumor is key in predicting survival. It shows how much the tumor cells look like normal cells. This grade tells us how aggressive the tumor is.
We use the World Health Organization (WHO) grading system. It classifies brain tumors based on their look and behavior. This helps us know what to expect and how to treat the tumor.
WHO Grading System Explained
The WHO grading system puts brain tumors into four grades. Grade I tumors are the least aggressive and look most like normal brain tissue. On the other hand, Grade IV tumors are the most aggressive and malignant.
Grade I and II (Low-Grade) Tumor Outcomes
Patients with Grade I or II tumors usually have a better outlook. These tumors grow slowly and don’t spread much. Treatment often includes surgery, and sometimes, just watching or radiation therapy.
Grade III (Anaplastic) Tumor Survival
Grade III, or anaplastic, tumors are more aggressive than low-grade ones. They grow and spread more easily. The outlook for these tumors is less good, and treatment often includes surgery, radiation, and chemotherapy.
Grade IV (High-Grade) Tumor Prognosis
Grade IV tumors are the most aggressive and have a poor prognosis. They grow fast and spread a lot. Even with aggressive treatment, the survival chances for Grade IV tumors are tough.
Knowing the grade of a brain tumor is vital for doctors and patients. It affects treatment plans and survival hopes. By using the WHO system, we can predict outcomes better and tailor treatments to each patient’s needs.
Age-Related Factors in Brain Tumor Survival
Knowing how age affects brain tumor survival is key for good treatment plans. Age impacts not just the tumor type but also survival chances and treatment response.
Pediatric Brain Tumor Outcomes
Pediatric brain tumors are special challenges. Kids often have different tumors than adults, and their survival rates differ. Advances in pediatric neuro-oncology have boosted survival rates, with some tumors showing a 5-year survival rate over 80%.
Children’s brains are more resilient and can recover well from tough treatments. But, it’s important to manage long-term treatment effects to ensure a good quality of life.
Young Adults (Under 40) Survival Rates
Young adults with brain tumors usually have better survival rates than older adults. This is because they often have fewer health issues and respond better to treatment. Aggressive treatment approaches work well in this age group, leading to better survival chances.
- Higher tolerance to intensive therapies
- Better overall health
- Increased likelihood of undergoing aggressive treatment
Middle-Age Patient Statistics
Middle-aged patients (40 to 65 years old) have varied brain tumor types and survival rates. Health issues can make treatment harder and affect survival.
Statistics show this age group has a moderate survival rate. Finding the right balance between effective treatment and tolerance is key.
Elderly Patients and Treatment Tolerance
Elderly patients face unique challenges, like less physical strength and more health issues. These factors can limit treatment options and tolerance.
Tailored treatment approaches are vital for elderly patients. They aim to improve quality of life while maximizing survival benefits. Palliative care is also important for symptom management and better outcomes.
Surgical Approaches and Their Impact on Survival
Brain tumor surgery has changed a lot. Different methods affect survival in different ways. The right surgery is key to better outcomes.
Extent of Resection and Survival Correlation
How much of the tumor is removed matters a lot. Studies show more removal means better survival chances. We’ll look into how much removal affects survival.
A study in the Journal of Neurosurgery found a big difference. Patients with all tumor removed did much better than those with some left behind.
| Extent of Resection | Survival Rate |
| Gross Total Resection | 65% |
| Subtotal Resection | 40% |
| Partial Resection | 25% |
Advanced Surgical Techniques
New methods like intraoperative MRI and awake craniotomy make surgery safer and more precise. These help doctors remove more tumor while keeping brain functions safe.
Intraoperative MRI lets doctors see the tumor in real time. Awake craniotomy helps avoid brain damage by checking function during surgery.
Surgical Complications and Mortality Risk
Even with new tech, surgery can have risks. Knowing these risks helps set realistic hopes and outcomes for patients.
Problems like infection, brain damage, and swelling can happen. The risk depends on the tumor and the patient’s health.
- Infection: 2-5% risk
- Neurological deficits: 10-20% risk
- Cerebral edema: 5-10% risk
By using the latest techniques, we can make surgery safer and improve survival rates.
Adjuvant Therapies and Survival Enhancement
Adjuvant therapies have changed how we treat brain tumors. They help patients live longer by getting rid of cancer cells left after surgery. This reduces the chance of cancer coming back.
Radiation Therapy Protocols and Outcomes
Radiation therapy is a key adjuvant treatment for brain tumors. It uses high-energy rays to kill cancer cells. The success of this treatment depends on the tumor type, grade, and the patient’s health.
Radiation Therapy Outcomes:
| Tumor Type | Radiation Dose | Survival Rate |
| Glioblastoma | 60 Gy | 12-15 months |
| Meningioma | 50-54 Gy | 5-year survival: 80% |
Chemotherapy Regimens and Effectiveness
Chemotherapy is another adjuvant therapy for brain tumors. It uses drugs to kill cancer cells. How well chemotherapy works depends on the tumor type and the patient’s response.
Combined Modality Treatment Results
Using different treatments together, like radiation and chemotherapy, has shown great results. This approach helps treat the tumor from all sides. It leads to better survival rates and quality of life.
- Improved survival rates
- Enhanced tumor control
- Better quality of life
Timing of Adjuvant Therapy and Survival Impact
When adjuvant therapy starts can greatly affect survival. Starting it early after surgery helps tackle cancer cells quickly. This can lead to better outcomes.
- Early initiation of adjuvant therapy
- Personalized treatment planning
- Regular follow-up and monitoring
Molecular and Genetic Markers Predicting Survival
Understanding brain tumors at a molecular level is key to predicting survival and treatment. Recent studies have found several markers that greatly affect prognosis.
IDH Mutation Status and Prognosis
IDH mutations are linked to better survival in some brain tumors, like gliomas. Patients with these mutations often have a better outlook than those without.
IDH mutation status is now a major factor in glioma management. It helps guide treatment and patient care.
MGMT Promoter Methylation
MGMT promoter methylation is a key marker for glioblastoma patients. It silences the MGMT gene, which helps repair DNA.
Patients with this methylation tend to do better with certain chemotherapy. This leads to longer survival times.
1p/19q Codeletion in Oligodendrogliomas
The 1p/19q codeletion is a genetic sign of oligodendrogliomas. It happens when parts of chromosomes 1 and 19 are deleted.
Those with this codeletion in oligodendrogliomas usually have a better prognosis. They also respond well to chemotherapy and radiation.
Emerging Biomarkers for Survival Prediction
New biomarkers are being studied for their role in predicting survival in brain tumor patients. These include genetic mutations and molecular changes.
| Molecular Marker | Tumor Type | Prognostic Impact |
| IDH Mutation | Gliomas | Favorable |
| MGMT Promoter Methylation | Glioblastoma | Favorable with chemotherapy |
| 1p/19q Codeletion | Oligodendrogliomas | Favorable |
As research advances, we’ll better understand how genetics and brain tumors interact. This will help us predict outcomes and tailor treatments more effectively.
Innovative Treatments and Clinical Trials
Brain tumor treatment is on the verge of a big change. New treatments and ongoing trials are making a difference. Patients are now getting therapies that improve their quality of life and outcomes.
Immunotherapy Approaches
Immunotherapy uses the body’s immune system to fight cancer. It’s showing great promise in treating brain tumors. Researchers are looking into different ways to boost the immune system’s fight against tumors.
Key Benefits of Immunotherapy:
- Potential for targeted treatment with fewer side effects
- Ability to adapt to changing tumor characteristics
- Possibility of long-term immune memory against tumor cells
Targeted Molecular Therapies
Targeted molecular therapies focus on specific genetic or molecular changes in tumors. They aim to treat tumors more precisely, reducing side effects. For brain tumors, these therapies target specific mutations or pathways that help tumors grow.
| Therapy Type | Target | Potential Benefits |
| Targeted Molecular Therapy | Specific genetic mutations | Precision treatment, reduced side effects |
| Immunotherapy | Cancer cells | Enhanced immune response, long-term protection |
| Tumor Treating Fields (TTFields) | Rapidly dividing tumor cells | Non-invasive, can improve survival with other treatments |
Tumor Treating Fields (TTFields)
TTFields is a non-invasive treatment that uses electric fields to stop tumor cells from dividing. It has been shown to improve outcomes when used with other treatments for certain brain tumors. This therapy offers a new way to slow tumor growth.
Accessing Clinical Trials for Improved Outcomes
Clinical trials are key to advancing brain tumor treatment. They offer patients access to new therapies not yet available. It’s important for patients to talk to their doctors about clinical trials to explore all treatment options.
Benefits of Participating in Clinical Trials:
- Access to cutting-edge treatments
- Potential for improved outcomes
- Contribution to advancing medical knowledge
As we keep exploring new treatments, the future for brain tumor patients looks brighter. Staying updated on the latest research and trials helps patients and their families make better care choices.
Quality of Life Considerations After Surgery
After brain tumor surgery, quality of life is complex. It involves many health aspects. Today, we focus on helping patients not just survive but thrive.
Neurological Function Preservation
Keeping neurological function intact is key after surgery. Neurological function preservation helps patients do daily tasks and stay independent. We use new surgical methods like intraoperative MRI and awake craniotomy to protect brain tissue.
This approach helps patients enjoy a better quality of life after surgery. They can keep their motor skills, senses, and thinking sharp.
Cognitive and Psychological Outcomes
Cognitive and psychological health are also important for quality of life. Patients who get support like counseling and cognitive therapy do better.
Improving cognitive outcomes requires teamwork from neurology, psychology, and rehab medicine. This way, patients can get back their thinking skills and adjust to changes.
Seizure Management and Control
Managing seizures is vital for brain tumor patients after surgery. Seizure management uses medicine and lifestyle changes to prevent seizures. We create a plan that fits each patient’s needs.
Controlling seizures boosts a patient’s quality of life and overall happiness and confidence.
Rehabilitation Strategies and Their Effectiveness
Rehabilitation strategies are key for recovery after brain tumor surgery. A good rehab program includes physical, occupational, and speech therapy, customized for each patient.
These rehabilitation strategies lead to big improvements in patients’ abilities and quality of life. It shows the value of a team effort in care after surgery.
Long-Term Survivors: Case Studies and Common Factors
Looking into the lives of long-term brain tumor survivors can teach us a lot. By studying their stories and finding common traits, we learn what helps them live longer and better.
Exceptional Responders to Standard Therapy
Some patients beat the odds and live longer than expected. For example, a study in a top medical journal told of a glioblastoma patient who did great with temozolomide and radiation. This patient lived longer than most with this type of tumor.
These patients often have special genetic or molecular traits. These traits make their tumors more treatable. Finding these traits can help doctors tailor treatments for others with similar tumors.
Survivors of Aggressive Tumor Types
People who beat aggressive tumors, like glioblastoma, have amazing stories. One young adult had a big surgery and then a new mix of chemotherapy and immunotherapy. This combo greatly reduced the tumor and extended their life.
These stories show how important bold and new treatments are for aggressive tumors.
Psychological Resilience Factors
Being mentally strong is key for brain tumor patients. Research shows that those with strong support, a positive outlook, and good coping skills do better. They live longer and have a better quality of life.
For example, a brain tumor survivor credits her family, meditation, and joining a support group. These helped her deal with stress and stay hopeful during treatment.
Lifestyle Patterns Among Long-Term Survivors
Long-term survivors often change their lifestyle after diagnosis. They start eating better, exercising more, and managing stress. These changes help them feel better and might even help them live longer.
| Lifestyle Factor | Common Practices Among Long-Term Survivors |
| Diet | More fruits, veggies, and whole grains; less processed foods and sugar. |
| Exercise | Regular activities like walking, yoga, or swimming, based on their health. |
| Stress Management | Practices like mindfulness, meditation, or therapy to handle stress. |
By learning from these survivors, doctors can give better care. This could lead to more people living longer and better with brain tumors.
Strategies to Improve Survival Outlook
Improving survival for brain tumor patients requires a detailed plan. This plan includes medical treatments, lifestyle changes, and support care.
Early Detection and Its Impact
Early detection is key to better survival rates for brain tumors. Finding tumors early means treatment can start sooner, leading to better results.
Regular health checks and knowing symptoms help find tumors early. New diagnostic tools like MRI and CT scans help spot tumors sooner.
Multidisciplinary Treatment Approaches
Using a team approach is vital for treating brain tumors. This team includes neurosurgeons, oncologists, and more.
Combining surgery, radiation, and chemotherapy can improve results. The treatment plan depends on the tumor’s type, size, and location, and the patient’s health.
| Treatment Modality | Description | Benefits |
| Surgery | Removal of the tumor | Potential for complete removal, reduced tumor burden |
| Radiation Therapy | High-energy rays to kill tumor cells | Effective for tumors that cannot be fully removed surgically |
| Chemotherapy | Drugs to kill tumor cells | Can be used alone or in combination with other treatments |
Nutrition and Exercise Considerations
Nutrition and exercise are important for brain tumor patients. Eating well helps keep strength up and aids in recovery.
Doing gentle exercises like yoga and walking can boost physical function and lower stress. Always talk to a doctor before starting new exercise or diet plans.
Stress Management and Support Systems
Managing stress and having a strong support system are key for brain tumor patients. Stress-reducing activities like meditation and deep breathing help.
Support from loved ones and groups can offer emotional and practical help. Counseling and psychological services are also important for dealing with the emotional side of a brain tumor diagnosis.
By using these strategies, brain tumor patients can improve their survival chances and quality of life.
Conclusion
Knowing about brain tumor survival rates is key for patients and their families. This knowledge helps them understand their journey with diagnosis and treatment. We’ve looked at how survival rates are affected by things like tumor type, grade, age, and treatment.
Our team is all about giving top-notch care to brain tumor patients. We use the latest in surgery and treatments, plus support services to improve life quality. We stress the need for a team effort to better survival rates and outcomes for patients.
As we move forward in neuro-oncology, keeping up with new research and treatments is vital. We’re committed to providing world-class care and support to patients from around the world. Our goal is to make sure everyone gets the best care for their unique needs.
FAQ
What is the overall 5-year survival rate for brain tumor patients?
The 5-year survival rate for brain tumor patients varies a lot. It depends on the tumor type, grade, and where it is. For example, glioblastoma has a 5-year survival rate of about 22%. But, some meningiomas can have a survival rate over 90%.
How does the type of brain tumor affect survival rates?
Different brain tumors have different survival rates. Glioblastoma has a poor prognosis with a 5-year survival rate of around 22%. On the other hand, meningioma, the benign type, can have a survival rate over 90%. Survival rates for astrocytoma, oligodendroglioma, and ependymoma depend on their grade and genetics.
What is the significance of tumor grade in brain tumor survival?
Tumor grade is very important for survival. The World Health Organization (WHO) grades tumors from I (benign) to IV (highly malignant). Higher grades mean a poorer survival rate. For example, Grade I tumors have a much better prognosis than Grade IV tumors like glioblastoma.
How does age influence brain tumor survival rates?
Age is a big factor in brain tumor survival. Younger patients usually have better survival rates than older ones. This is because younger people can handle treatments better and have fewer health problems.
What is the impact of surgical resection on brain tumor survival?
How much of the tumor is removed during surgery greatly affects survival. Removing as much as possible is often linked to better survival rates. New surgical techniques and tools help achieve this goal.
How do adjuvant therapies like radiation and chemotherapy affect survival?
Treatments like radiation and chemotherapy are very important for brain tumor patients. They help improve survival rates, but their effectiveness depends on the tumor type and grade. Using a combination of treatments often works better than one treatment alone.
What role do molecular and genetic markers play in predicting survival?
Molecular and genetic markers are key in predicting survival for brain tumor patients. Markers like IDH mutation status and MGMT promoter methylation provide important information. They help guide treatment decisions.
Are there innovative treatments that can improve brain tumor survival?
Yes, new treatments like immunotherapy and targeted molecular therapies are being tested. They could improve survival rates, mainly for aggressive or recurrent tumors.
How can patients improve their survival outlook after brain tumor surgery?
Improving survival after surgery involves several steps. Early detection, a team approach to treatment, and staying active are important. Also, managing stress and having a strong support system are key.
What is the importance of quality of life considerations after brain tumor surgery?
After surgery, keeping a good quality of life is essential. It’s important to preserve brain function, manage cognitive and emotional effects, and control seizures. Effective rehabilitation also plays a big role in improving patient outcomes.
References
National Center for Biotechnology Information. Evidence-Based Medical Insight. Retrieved from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4027119/