Last Updated on November 25, 2025 by Ugurkan Demir
It’s important to know the difference between supraventricular tachycardia (SVT) and atrial tachycardia. At Liv Hospital, we focus on making the right diagnosis. This is because both conditions can cause similar symptoms like palpitations, dizziness, and shortness of breath.
Compare svt vs atrial tach, their ECG differences, and treatment options explained.
Even though both start above the ventricles, they need different treatments. Our team uses the latest treatments to help each patient. We make sure our care is tailored to meet each person’s needs.

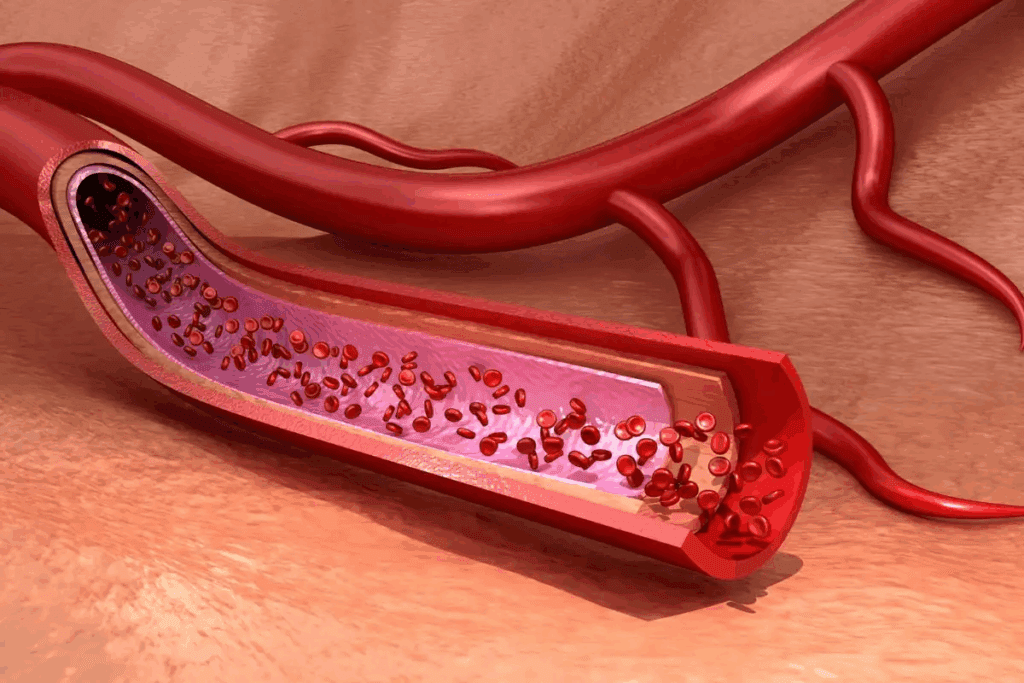
Cardiac arrhythmias are irregular heartbeats that can be too fast, too slow, or irregular. They affect the heart’s ability to function properly. Knowing about heart rhythm and its role in health is key.
A normal heart rhythm is consistent and coordinated, usually between 60 to 100 beats per minute at rest. Arrhythmias are deviations from this rhythm. Arrhythmias can be harmless or life-threatening, depending on their type and cause.
Knowing the difference between a normal heart rhythm and arrhythmias is vital. A normal rhythm ensures efficient blood circulation. But arrhythmias can cause symptoms like palpitations, dizziness, or even syncope.
The heart’s electrical conduction system controls the heartbeat. It starts with the sinoatrial (SA) node, the heart’s natural pacemaker. It generates electrical impulses that travel through the atria, causing them to contract.
These impulses then reach the atrioventricular (AV) node. This node delays the signal before it goes to the ventricles. This ensures coordinated contraction. Any disruption in this system can lead to arrhythmias, showing how critical it is.
Understanding the heart’s electrical system and how arrhythmias occur helps us appreciate cardiac health. It also highlights the need for proper diagnosis and treatment.

Supraventricular tachycardia, or SVT, is a heart rhythm disorder. It starts in the upper chambers of the heart. This affects how well the heart works.
SVT makes the heart beat too fast. It happens because of abnormal electrical signals in the upper heart chambers. Knowing the type helps doctors understand and treat it better.
Classification of SVT depends on where the problem starts. It can be AVNRT, AVRT, or other atrial tachycardias. Each needs a different approach to manage.
SVT comes in several forms, each with its own traits.
Knowing these types is key for proper diagnosis and treatment. We’ll look at how to diagnose and treat SVT next.
Atrial tachycardia (AT) is a heart rhythm disorder. It causes a fast heart rate in the upper heart chambers. Knowing its causes and symptoms is key to understanding it.
AT is caused by abnormal electrical activity in the upper heart chambers. It happens due to faulty electrical signals in the heart. This leads to a heart rate over 100 beats per minute.
Key factors contributing to AT include:
Paroxysmal atrial tachycardia (PAT) is a type of AT. It starts and stops suddenly. Episodes can last from a few minutes to hours and can happen without warning.
PAT can affect people with or without heart disease. Managing it involves treating the cause and controlling symptoms during episodes.
Several things can trigger atrial tachycardia. These include:
Knowing and managing these risk factors helps prevent AT episodes and lowers the risk of complications.
It’s important to know the differences between SVT and atrial tachycardia for the right treatment. Both have fast heart rates, but they start and work in different ways.
SVT starts in the upper heart chambers, like the atria or the area where the atria meet the ventricles. It includes arrhythmias like AVNRT and AVRT. On the other hand, atrial tachycardia is a fast heart rhythm that starts in the atria. The pathway for atrial tachycardia is mainly in the atrial tissue, while SVT can have more complex paths.
“The difference between these two is not just for learning; it affects treatment,” say heart doctors. “Getting the right diagnosis is key to choosing the right treatment.”
SVT often has a loop that includes the AV node. Atrial tachycardia starts in the atria and can be focal or multi-focal. This difference is important because it changes how we treat it. For example, SVT might respond well to certain treatments, while atrial tachycardia might need more specific treatments for the atria.
Knowing the difference between SVT and atrial tachycardia is very important. Getting it wrong can lead to the wrong treatment, which can make things worse. For instance, using certain treatments for atrial tachycardia can be harmful. So, it’s critical to get a precise diagnosis through tests or other tools.
In summary, while SVT and atrial tachycardia have some similarities, their differences are big. Knowing these differences helps doctors give the best care.
Knowing the symptoms of SVT and atrial tachycardia is key for quick medical help. Both can show similar signs, making it hard to diagnose. But, doctors look for specific differences.
People with SVT and atrial tachycardia often feel their heart beating irregularly or too hard. They might also have chest pain or discomfort, shortness of breath, and dizziness or lightheadedness. Some feel fatigue or just not well.
In bad cases, SVT or atrial tachycardia can cause syncope (fainting) or near-syncope. This happens because the heart doesn’t pump well. It leads to less blood to the brain and other important parts.
Get medical help if you have severe chest pain, trouble breathing, or feel very dizzy. Also, if you’ve had heart problems before or if your symptoms get worse, call your doctor.
SVT and atrial tachycardia can really affect your life. They can make you anxious and stressed, making everyday tasks hard. It’s important to manage these conditions well to improve your life and avoid serious problems.
By knowing the symptoms and getting the right medical care, people with SVT and atrial tachycardia can live full lives. It’s vital to work with your doctor to find the best treatment for you.
To tell SVT from AT, doctors use many tests. These include ECG, Holter and event monitors, and electrophysiology studies. These tests help find the right treatment for each arrhythmia.
The ECG is key in diagnosing SVT and AT. It shows the heart’s electrical activity. Doctors look for patterns that show these arrhythmias.
Holter and event monitors are great for those with symptoms that come and go. They record the heart’s rhythm for hours or days. Holter monitors record for 24 to 48 hours. Event monitors are worn longer and activated by the patient.
Sometimes, electrophysiology studies (EPS) are needed. EPS involves putting catheters in the heart to record its electrical activity. It helps find the arrhythmia’s cause and guides treatment.
When diagnosing SVT and AT, other conditions must be ruled out. These include sinus tachycardia, atrial fibrillation, and ventricular tachycardia. A detailed check-up and tests help doctors find the right treatment.
Managing SVT and atrial tachycardia needs a team effort. It’s about getting the heart back to normal quickly. This includes using different methods to fix the rhythm and ease symptoms.
Vagal maneuvers help by stimulating the vagus nerve. This can slow the heart and switch it back to normal. Here are some common ones:
These methods are often the first thing doctors try. They can stop SVT episodes.
If vagal maneuvers don’t work, doctors might use emergency drugs. These include:
The right drug depends on the patient’s situation and medical history.
Cardioversion uses an electrical shock to fix the heart rhythm. It’s great for SVT and some atrial tachycardia cases.
There are two types:
If initial steps fail or the patient is unstable, emergency protocols kick in. These include:
By using these strategies, doctors can manage SVT and atrial tachycardia well. This improves patient results and lowers the chance of problems.
Managing supraventricular tachycardia (SVT) and atrial tachycardia long-term is complex. It involves using medicines, catheter ablation, and making lifestyle changes. We work with patients to create a treatment plan that fits their needs.
Medicines are key in treating SVT and atrial tachycardia. They help control symptoms, prevent episodes, and manage related conditions. Common medicines include beta-blockers, calcium channel blockers, and anti-arrhythmic drugs.
Table: Common Medications for SVT and Atrial Tachycardia
| Medication Class | Examples | Primary Use |
| Beta-blockers | Metoprolol, Propranolol | Control heart rate, reduce symptoms |
| Calcium Channel Blockers | Verapamil, Diltiazem | Slow heart rate, manage symptoms |
| Anti-arrhythmic Drugs | Flecainide, Sotalol | Prevent arrhythmia episodes |
Catheter ablation is a minimally invasive procedure. It destroys abnormal electrical pathways in the heart. This method is great for those who don’t respond to medicines or want a lasting solution.
We use advanced technologies to make the procedure precise and safe. Success rates depend on the condition and patient factors. But, it’s a promising option for long-term management.
Lifestyle changes are important in managing SVT and atrial tachycardia. We advise patients on several changes. These include avoiding caffeine and alcohol, staying at a healthy weight, exercising regularly, and managing stress through meditation or yoga.
Combining these lifestyle changes with medical treatments helps patients control their condition better. This improves their quality of life.
Managing arrhythmias is complex and needs teamwork. At Liv Hospital, we have a team of electrophysiologists and support staff. They use various medical specialties and the latest technology to tackle this challenge.
Electrophysiologists are at the core of our team. They specialize in heart rhythm disorders. They work with cardiologists, radiologists, and others to give patients the best care.
Key responsibilities of electrophysiologists include:
Liv Hospital is known for its detailed approach to arrhythmia management. We use the latest technology and focus on patient care. Our facilities and equipment help us treat even the most complex cases.
Our treatment approach includes:
We focus on patient-centered care at Liv Hospital. We believe patients do best when they’re involved in their care. Our team educates patients, discusses treatment options, and creates care plans that fit their needs.
The benefits of our approach include:
By combining teamwork with patient-centered care, Liv Hospital offers top-notch arrhythmia management. We meet each patient’s unique needs.
It’s important to know the difference between Supraventricular Tachycardia (SVT) and Atrial Tachycardia (AT). We’ve looked at how they are different, including where they start and how they affect the heart. This knowledge helps doctors find the right treatment.
Doctors use many ways to figure out if someone has SVT or AT. They look at heart rhythm on an ECG, use Holter and event monitors, and do electrophysiology studies. Finding out what’s wrong is key to choosing the right treatment.
At Liv Hospital, we work together to manage heart rhythm problems. We focus on what each patient needs, whether it’s SVT or AT. This way, we can create a treatment plan that works best for them.
In short, knowing the difference between SVT and AT is key to treating them right. With the right tools and treatments, we can make patients’ lives better and improve their health.
SVT is a term for many tachycardias from above the ventricles. Atrial tachycardia is a specific SVT from the atria.
Paroxysmal atrial tachycardia (PAT) is a sudden, temporary rapid heart rate from the atria.
Doctors use ECGs, Holter and event monitors, and electrophysiology studies to find the cause and type of arrhythmia.
Symptoms include palpitations, rapid heart rate, shortness of breath, chest pain, and dizziness.
Treatments include vagal maneuvers, emergency meds, cardioversion, pharmacological management, catheter ablation, and lifestyle changes.
Catheter ablation uses energy to destroy abnormal heart pathways causing arrhythmia.
Yes, avoiding triggers, maintaining a healthy weight, and reducing stress can manage symptoms and episodes.
Electrophysiologists are cardiologists who diagnose and treat heart rhythm disorders, including SVT and atrial tachycardia, with advanced techniques.
Liv Hospital uses a team of experienced electrophysiologists and cardiologists for a personalized approach to treating SVT and atrial tachycardia.
Atrial tachycardia is a type of SVT from the atria. SVT is a broader term for tachycardias from above the ventricles.
Subscribe to our e-newsletter to stay informed about the latest innovations in the world of health and exclusive offers!