Last Updated on December 1, 2025 by Bilal Hasdemir

Understanding the T3 tumor stage is essential for effective treatment planning and prognosis. What is a T3 tumor stage? Our essential guide explains this awful diagnosis and the critical facts about cancer staging.
Key Takeaways
- The T3 classification plays a crucial role in determining prognosis and treatment options.
- The T3 classification shows a specific tumor size and extent.
- Understanding T3 is vital for healthcare providers and patients.
- T3 tumor stage affects overall cancer staging and treatment strategy.
- Oncology terminology like T3 classification aids in precise diagnosis.
The TNM system is the global standard for classifying cancer’s spread. It’s used by oncologists and healthcare professionals to stage cancer. This helps them describe the extent of cancer’s spread in a consistent way.
History and Development of TNM
The TNM staging system was created by the Union for International Cancer Control (UICC) and the American Joint Committee on Cancer (AJCC). It was first published in 1953 by Pierre Denoix. Over the years, it has been updated to include new knowledge and improve its accuracy.
The TNM system’s development was a big step in oncology. It gave a standardized way to classify cancer. This has helped healthcare professionals around the world to talk about cancer cases clearly. It makes research, treatment planning, and patient care easier.
Purpose of Cancer Staging
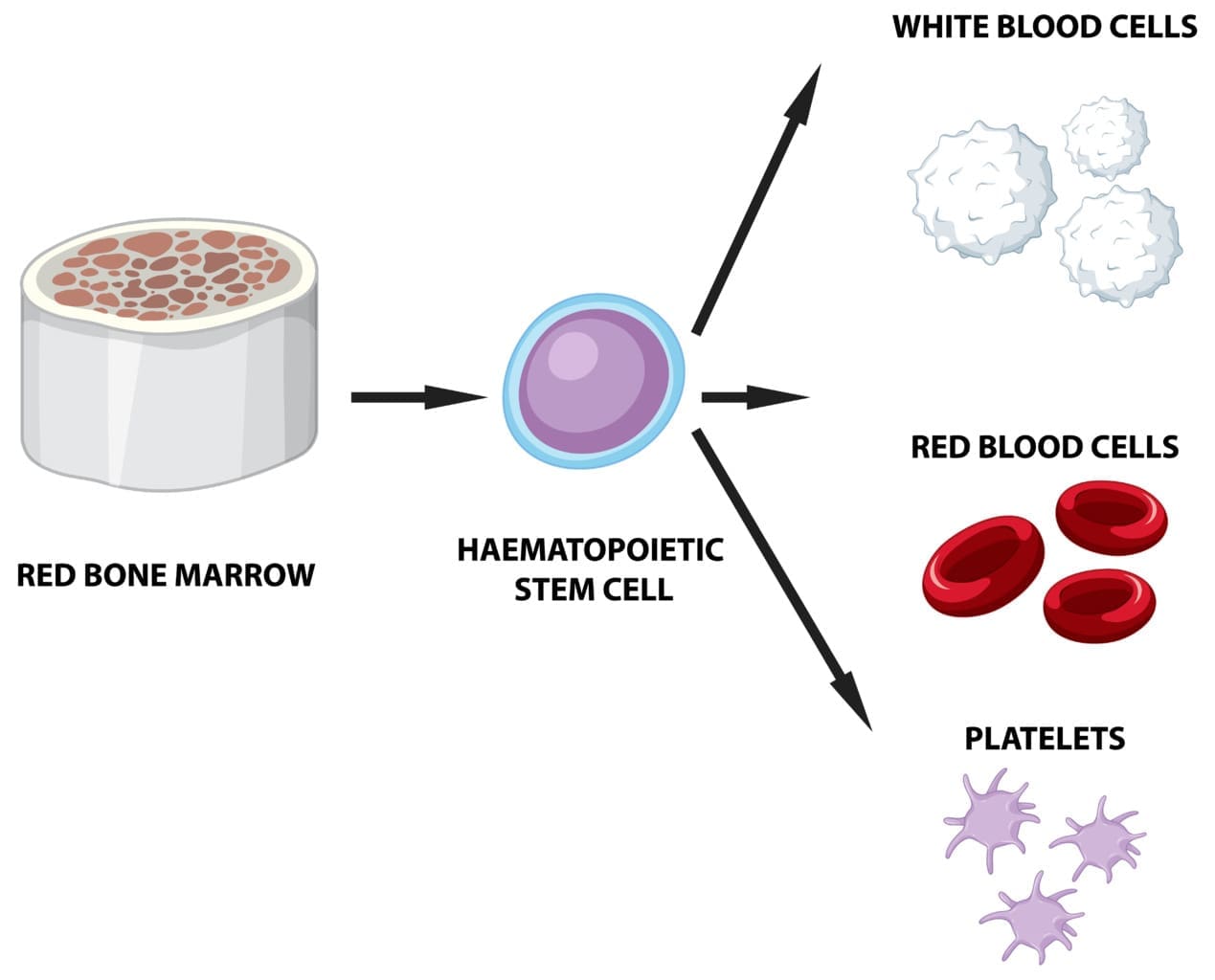
The main goal of the TNM staging system is to provide a consistent and reliable way to classify cancer. It looks at three main things: the size and extent of the primary tumor (T), the involvement of regional lymph nodes (N), and the presence of distant metastasis (M).
| Component | Description |
| T | Primary Tumor Size and Extent |
| N | Regional Lymph Node Involvement |
| M | Distant Metastasis |
Understanding these components helps healthcare professionals figure out the cancer stage. This is key for creating an effective treatment plan and predicting patient outcomes.
Definition of T3 Classification
The T3 classification is based on the tumor’s size or spread. T3 tumors are bigger or more invasive than T1 or T2. The exact criteria for T3 can change based on the cancer type.
In colorectal cancer, T3 tumors grow through the muscularis propria. They reach the pericolorectal tissues but not other organs.
Understanding the T3 tumor stage is essential for effective treatment planning and prognosis.
- Larger tumor size compared to T1 and T2
- More extensive invasion into surrounding tissues
- May not have reached nearby organs or structures
How T3 Differs from Other T Stages
The T3 stage is different from other T stages in size and invasion. Let’s look at the differences:
| T Stage | Tumor Size/Extent | Typical Characteristics |
| T1 | Small | Limited to the organ of origin |
| T2 | Moderate | Some invasion into surrounding tissues |
| T3 | Large or extensive | Significant invasion into surrounding tissues |
| T4 | Very large or highly invasive | Invasion into nearby organs or structures |
Understanding the T3 tumor stage is essential for effective treatment planning and prognosis. It helps doctors plan the best treatment and talk about outcomes with patients.
Components of TNM Staging

The TNM staging system helps classify how far cancer has spread. It’s key for figuring out treatment and how well a patient might do.
This system looks at three main parts: the size of the main tumor (T), if nearby lymph nodes are affected (N), and if cancer has spread to distant places (M). Each part gives important clues about the cancer’s spread.
T: Primary Tumor Size and Extent
The “T” part talks about the tumor’s size and if it’s grown into nearby tissues. Tumors are classified based on their size and how far they’ve grown. For example, a small tumor is different from a big one that’s grown into other tissues.
Tumor size is very important. Bigger tumors mean cancer is more advanced. How far the tumor has grown into nearby tissues also matters a lot.
N: Regional Lymph Node Involvement
The “N” part shows if cancer has reached nearby lymph nodes and how much. Lymph nodes are small, bean-shaped parts of the body’s lymph system. They help fight infections and diseases.
Understanding the T3 tumor stage is essential for effective treatment planning and prognosis.
M: Distant Metastasis
The “M” part tells if cancer has spread to other parts of the body. This means cancer has moved from the original site and nearby lymph nodes to other areas.
Having distant metastasis is a big deal in cancer staging. It means cancer is more advanced and might need different treatments. This can affect how well a patient might do.
Clinical Significance of T3 Classification
eans the cancer is more advanced. This requires a detailed plan to find the best treatment.
Impact on Treatment Planning
A T3 tumor changes how doctors plan treatments. It often needs a team effort from surgeons, medical oncologists, and radiation oncologists. This team works together to create a good treatment plan.
The size and spread of T3 tumors might need neoadjuvant therapies to shrink the tumor before surgery. Or, adjuvant therapies to kill any cancer cells left after surgery.
Treatment for T3 cancers can be surgery, radiation, chemotherapy, or a mix of these. The choice depends on the tumor’s location, the patient’s health, and the cancer type.
Specific Criteria for T3 in Colon Cancer
In colon cancer, T3 tumors grow through the muscularis propria into the pericolorectal tissues. This makes T3 tumors different from T1 and T2, which stay within the colon wall.
- Tumors that have grown through the muscularis propria
- Invasion into the pericolorectal tissues
- No perforation of the visceral peritoneum
The T3 classification plays a crucial role in determining prognosis and treatment options.
Treatment Approaches for T3 Colorectal Tumors
Treatment for T3 colorectal cancer often includes surgery, chemotherapy, and sometimes radiation therapy. The treatment plan depends on the tumor’s location, size, and the patient’s health.
| Treatment Modality | Description | Applicability to T3 Colorectal Cancer |
| Surgery | Primary treatment involving resection of the tumor and affected tissues | Often the first-line treatment for localized T3 tumors |
| Chemotherapy | Systemic treatment using drugs to kill cancer cells | Used before or after surgery to address microscopic disease |
| Radiation Therapy | Localized treatment using high-energy rays to kill cancer cells | May be used for rectal cancers to shrink tumors before surgery |
The T3 classification plays a crucial role in determining prognosis and treatment options.
The T3 classification plays a crucial role in determining prognosis and treatment options.
The TNM staging system is used by the American Joint Committee on Cancer (AJCC). The ‘T’ in TNM stands for the tumor’s size and how far it has spread.
Defining Features of T3 Lung Tumors
T3 lung tumors are big or have extra nodules in the same lung lobe. They are more than 5 cm but not over 7 cm. Or, they have extra nodules in the same lobe.
Key features of T3 lung tumors include:
- Tumors larger than 5 cm but not exceeding 7 cm
- Presence of additional tumor nodules in the same lobe
- Involvement of structures such as the chest wall, diaphragm, or phrenic nerve
Management Strategies for T3 Lung Cancer
Understanding the T3 tumor stage is essential for effective treatment planning and prognosis.
Surgical resection is considered when possible. It’s often with adjuvant therapy to lower recurrence risk. For those not good for surgery, chemoradiation is an option.
Treatment options may include:
- Surgery, such as lobectomy or pneumonectomy
- Chemotherapy to address microscopic spread
- Radiation therapy to control local disease
- Targeted therapy or immunotherapy based on tumor characteristics
Patients with T3 lung cancer should talk to a team. This team will help find the best treatment plan for them.
The T3 classification plays a crucial role in determining prognosis and treatment options.
Characteristics of T3 Breast Tumors
T3 breast tumors are over 5 cm in size. This size means the cancer is more advanced and may need intense treatment. The tumor’s grade and hormone receptor status also affect the prognosis.
Treatment Options for T3 Breast Cancer
Treatment for T3 breast cancer usually involves several steps. These include surgery, chemotherapy, radiation, and hormone therapy. The treatment choice depends on the tumor’s hormone and HER2 status, and the patient’s health.
- Surgery: Surgery might be mastectomy or breast-conserving, based on the tumor’s size and location.
- Chemotherapy: Chemotherapy is often used to lower the risk of recurrence and metastasis.
- Radiation Therapy: Radiation therapy may be used after surgery to kill any cancer cells left behind.
- Hormone Therapy: For hormone receptor-positive tumors, hormone therapy can help prevent recurrence.
Criteria for T3 Prostate Tumors
T3 prostate cancer means the tumor has grown beyond the prostate gland. It’s split into T3a and T3b based on how far it has spread.
T3a Classification: This is for tumors that have grown past the prostate but not into the seminal vesicles.
T3b Classification: This is for tumors that have invaded the seminal vesicles. It shows a more serious invasion.
Therapeutic Approaches for T3 Prostate Cancer
T3 prostate cancer treatment often combines different methods. This approach aims for the best results.
- Radiation Therapy: This can be external beam radiation or brachytherapy. It’s used alone or with hormone therapy.
- Hormone Therapy: Known as androgen deprivation therapy (ADT), it lowers testosterone. This slows cancer cell growth.
- Radical Prostatectomy: Surgery to remove the prostate gland. It’s considered for some T3 patients, followed by more treatment.
| Treatment Modality | Description | Applicability to T3 Prostate Cancer |
| Radiation Therapy | External beam radiation or brachytherapy | Often used, may be combined with hormone therapy |
| Hormone Therapy | Androgen deprivation therapy (ADT) | Commonly used to reduce testosterone levels |
| Radical Prostatectomy | Surgical removal of the prostate gland | Considered for selected patients, often followed by adjuvant therapy |
The right treatment for T3 prostate cancer depends on many things. These include the patient’s health, the tumor’s details, and what the patient prefers.
T3 Classification in Head and Neck Cancers
Site-Specific T3 Criteria in Head and Neck Regions
Understanding the T3 tumor stage is essential for effective treatment planning and prognosis.
| Cancer Site | |
| Larynx | Vocal cord fixation or large tumor size |
| Oral Cavity | Tumor size > 4 cm or deep invasion |
| Nasopharynx | Tumor extension to cranial nerves or infratemporal fossa |
| Oropharynx | Tumor size and extent, potentially involving nearby structures |
Treatment Modalities for T3 Head and Neck Tumors
Treatment for T3 head and neck cancers often combines surgery, radiation, and chemotherapy. The treatment choice depends on the cancer site, the patient’s health, and other factors.
For instance, a T3 laryngeal cancer might need a total laryngectomy or chemoradiation. T3 oral cavity cancers might get surgery followed by radiation or chemoradiation.
Here’s a list of common treatments for T3 head and neck cancers:
- Surgery: Removes the tumor and affected tissues
- Radiation Therapy: Uses high-energy rays to target cancer cells
- Chemotherapy: Kills cancer cells with drugs
- Targeted Therapy: Targets specific molecules in cancer growth
- Immunotherapy: Boosts the body’s immune system to fight cancer
Understanding T3 classification helps healthcare providers tailor treatments to each patient’s needs.
Diagnostic Methods for T3 Tumors
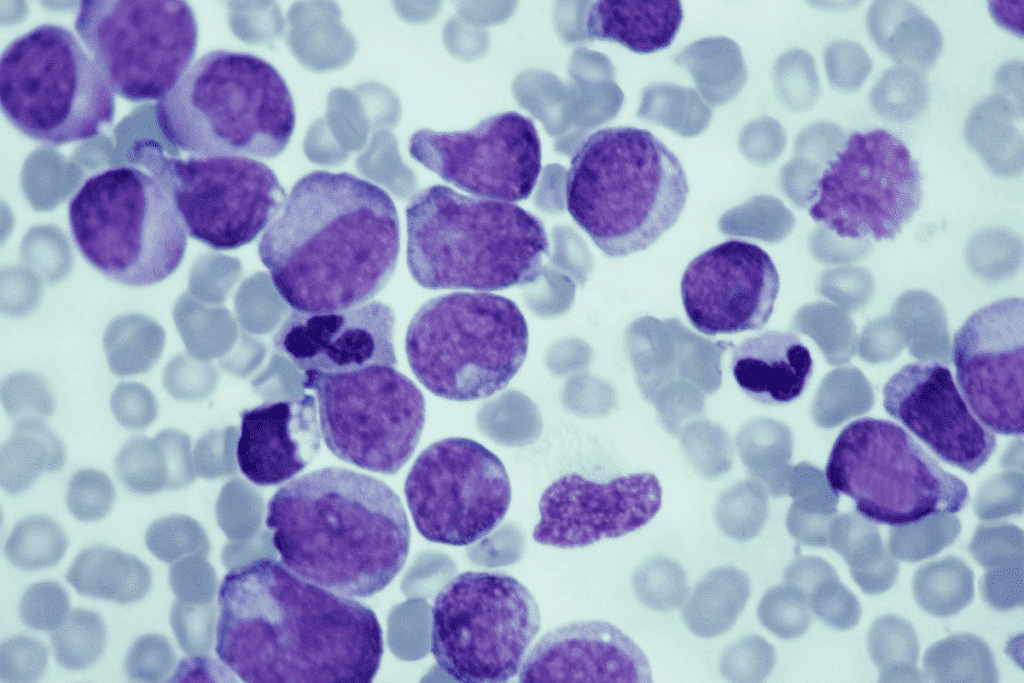
Diagnosing T3 tumors requires a detailed approach. It uses many diagnostic techniques. Getting the diagnosis right is key to choosing the right treatment and understanding the patient’s future.
Imaging Techniques
Positron Emission Tomography (PET) scans might also be used. They check how active the tumor is and if it has spread. The choice of scan depends on the cancer type and the tumor’s features.
Biopsy and Pathological Assessment
Histopathological evaluation is important for confirming the diagnosis. It helps understand the tumor’s behavior and how it might react to treatment.
Molecular and Genetic Testing
Molecular and genetic testing are also used for T3 tumors. These tests look for specific genetic changes or biomarkers. They can help decide on the best treatment and predict the outcome.
These tests can find targets for therapy, leading to more tailored treatments. Adding molecular and genetic data to diagnosis makes treatment planning more accurate for T3 tumors.
Multidisciplinary Approach to T3 Cancer Management
T3 cancer is complex and needs a team of experts for the best care. It’s not just one doctor’s job; many specialties work together. This team tackles the disease from all angles.
Tumor Board Recommendations
The tumor board is key in this team effort. Here, doctors from different fields share patient cases and plan treatments. Tumor boards make sure all viewpoints are heard, leading to better decisions.
“The tumor board brings together experts from various disciplines to review patient cases and recommend treatment strategies based on the latest evidence and guidelines.”
Doctors like surgeons, oncologists, and radiologists join the tumor board. They look at every part of a patient’s health. This way, they create the best treatment plan.
Integrated Care Models
Integrated care is also vital for T3 cancer management. It means working together across different healthcare settings. Integrated care makes care smoother and better for patients.
| Benefits of Integrated Care | Description |
| Improved Patient Outcomes | Coordinated care leads to better health outcomes due to thorough treatment planning. |
| Enhanced Patient Experience | Patients feel less fragmented in their care, leading to higher satisfaction. |
| Efficient Resource Utilization | Resources are used better, cutting costs and improving care delivery. |
Coordination Between Specialists
Good teamwork is essential in T3 cancer care. Doctors need to talk often to keep care on track. Good teamwork avoids mistakes, saves time, and improves care quality.
In summary, managing T3 cancer well needs a team effort. Tumor boards, integrated care, and teamwork are key. Together, doctors ensure patients get the best care for their condition.
Patient Considerations with T3 Cancer Diagnosis
Getting a T3 cancer diagnosis starts a journey with many challenges. It affects not just your health but also your mind and feelings.
Understanding Your Diagnosis
Key aspects to discuss with your healthcare provider include:
- The specific characteristics of your T3 tumor
- Available treatment options and their possible side effects
- The role of additional therapies such as chemotherapy or radiation
- How your overall health impacts your treatment plan
Quality of Life Concerns
Keeping your quality of life good is a big part of cancer care, even more so with a T3 diagnosis. Treatment can change many parts of your life, from how you feel physically to your mood. It’s important to talk about these issues to get the best care.
Some common quality of life concerns include:
| Concern | Description | Potential Solutions |
| Pain Management | Managing pain from the tumor and treatment | Medications, alternative therapies like acupuncture |
| Nutritional Support | Keeping up with nutrition during treatment | Dietary counseling, nutritional supplements |
| Emotional Support | Dealing with the emotional side of cancer and treatment | Counseling, support groups, mindfulness practices |
Support Resources and Services
There are many support resources and services for patients with a T3 cancer diagnosis. These can offer emotional help, practical aid, and information to help you through your cancer journey.
Available support resources include:
- Cancer support groups, either in-person or online
- Nutritional and counseling services made for cancer patients
- Educational materials and workshops on managing cancer and its treatment
Clinical Trials and Research for T3 Cancers
Ongoing clinical trials are key to finding new treatments for T3 cancers. They help us understand the disease better and improve patient care.
Current Clinical Trials
Many clinical trials are looking into new ways to treat T3 cancers. They focus on targeted therapies, immunotherapies, and combining treatments.
Emerging Therapeutic Approaches
New ways to treat T3 cancers are showing great promise. These include personalized medicine and novel drug delivery systems.
Some exciting research areas include:
- Studying genetic mutations in T3 cancer.
- Looking into liquid biopsies for early detection.
- Developing combination therapies to target multiple pathways.
These advancements highlight the need for ongoing research and trials. They are vital for better outcomes in T3 cancer patients.
Different staging systems are used worldwide, which affects T3 classification. For example, the TNM system is widely used but not the same everywhere. It was developed by the Union for International Cancer Control (UICC) and the American Joint Committee on Cancer (AJCC).
Different Staging Systems Worldwide
Many staging systems are used globally, each with its own rules for tumor classification. The TNM system is very common, but others like the Ann Arbor staging for lymphomas and the FIGO staging for gynecological cancers are also used a lot.
- The TNM system looks at the tumor’s size and spread (T), lymph node involvement (N), and if there are distant metastases (M).
- Other systems might use different factors or criteria for the same cancer type, causing differences in T3 classification.
Harmonization Efforts in Cancer Staging
There are efforts to make cancer staging more uniform. These come from international work among oncology groups and research places. They want to standardize staging and make data easier to compare across regions.
“Standardizing cancer staging is key for better understanding cancer biology and improving patient care worldwide.”
The harmonization process includes:
- Updating staging manuals and guidelines with the latest research and practices.
- Encouraging the use of common systems like TNM for solid tumors.
- Improving education and training for healthcare workers on new staging protocols.
By aiming for consistent cancer staging, the oncology field can share data better, predict outcomes more accurately, and develop more effective treatments for patients everywhere.
Survival Rates and Prognosis for T3 Cancers
Understanding the T3 tumor stage is essential for effective treatment planning and prognosis.
Cancer-Specific Survival Statistics
Survival rates for T3 cancers differ by type. For example, T3 breast cancer and T3 lung cancer have different survival chances. Studies show that T3 breast cancer has a 5-year survival rate of 70-80%. On the other hand, T3 lung cancer’s rate is between 20-30%.
Factors Affecting Prognosis Beyond T Stage
While the T stage is important, other factors also matter. These include:
- Nodal involvement (N stage)
- Presence of metastasis (M stage)
- Patient’s overall health and comorbidities
- Genetic and molecular characteristics of the tumor
“Comprehensive cancer care involves not just treating the tumor, but also addressing the patient’s overall well-being.”
This approach is key to better survival and quality of life for T3 cancer patients.
Healthcare providers can give more accurate forecasts and create effective plans by considering these factors. This helps meet each patient’s unique needs.
FAQ
How is T3 different from other T stages?
The TNM system is a way to stage cancer. It looks at the tumor’s size and spread (T), nearby lymph nodes (N), and if the cancer has spread (M).
What are the treatment options for T3 cancer?
Treatment for T3 cancer depends on the cancer type. It might include surgery, chemotherapy, or radiation therapy. The best plan depends on the patient’s needs and the tumor’s characteristics.
What are the diagnostic methods used to identify T3 tumors?
To find T3 tumors, doctors use CT scans, MRI, and PET scans. They also do biopsies and check the tumor’s cells. Molecular and genetic tests help diagnose and stage cancer.
Managing T3 cancer needs a team effort. Doctors, surgeons, and specialists work together. They create a detailed treatment plan for the patient.
What are the survival rates for T3 cancers?
Survival rates for T3 cancers vary by cancer type. Looking at cancer-specific survival statistics can give insight into a patient’s prognosis.
Are there any clinical trials or emerging therapeutic approaches for T3 cancers?
Yes, there are clinical trials and new treatments for T3 cancers. These include new drugs, targeted therapies, and immunotherapies. They offer hope for better treatment options.
How do different staging systems used worldwide affect T3 classification?
Different staging systems have different T3 criteria. Efforts are being made to make cancer staging more consistent worldwide.
What are the quality of life concerns for patients with T3 cancer?
Patients with T3 cancer face many challenges. These include physical symptoms, emotional distress, and practical issues. Support services can help improve their quality of life.
What support resources and services are available for patients with T3 cancer?
Patients with T3 cancer can find many support resources. These include counseling, support groups, and practical help. These services can help them cope with cancer and enhance their quality of life.
References
JAMA Network. Evidence-Based Medical Insight. Retrieved from https://jamanetwork.com/journals/jamaoncology/fullarticle/2656351