Last Updated on December 3, 2025 by Bilal Hasdemir
TERF surgery helps with urination difficulty, offering breakthrough relief and faster recovery time.
Having trouble urinating can really affect your life. TURP (Transurethral Resection of the Prostate) is a common surgery for this issue. It helps with benign prostatic hyperplasia or blockages.

If other treatments don’t work, surgery might be needed. At Liv Hospital, our team offers personalized care. We focus on TURP and other surgeries for urinary problems.
It’s important to know about your surgery options. TURP is a proven method that can greatly improve your life. We also talk about the risks and new ways to care for patients before and after surgery.
Key Takeaways
- Surgical interventions like TURP are effective treatments for difficulty urinating caused by benign prostatic hyperplasia.
- TURP is a common and established procedure that can significantly improve quality of life.
- Non-surgical treatments should be considered before opting for surgery.
- Personalized care is key for the best results in TURP patients.
- Knowing the risks and new care methods is vital for today’s treatment plans.
Understanding Urinary Difficulties and Their Causes
Urinary problems can really affect a person’s life. Knowing what causes them is key to fixing them. We’ll look at why urine flow gets blocked, how Benign Prostatic Hyperplasia (BPH) works, and when surgery is needed.
Common Causes of Urinary Obstruction
Many things can block urine flow. These include an enlarged prostate, a narrow urethra, and bladder stones. An enlarged prostate is a big problem for older men. It can squeeze the urethra, making it hard to pee.
A 2023 study showed that waiting too long to get a TURP procedure after a sudden pee problem can fail 32.9% of the time after 10 years. This shows how important quick action is.
Benign Prostatic Hyperplasia (BPH) and Its Effects
BPH is when the prostate gets too big. It’s common in older men. Symptoms include weak pee, needing to pee a lot, and trouble starting to pee. If not treated, it can cause infections and harm the bladder.
A doctor said, “BPH can really hurt a man’s life quality.”
“The prostate orgasm is a complex phenomenon that is not fully understood, but it is believed to be related to the prostate gland’s role in male sexual function.”

When Surgery Becomes Necessary
If other treatments don’t work, surgery might be needed. Transurethral Resection of the Prostate (TURP) is a common surgery for BPH. Deciding to have surgery should be a careful choice based on health and symptoms.
Stress urinary incontinence is a problem that can happen. It’s when you pee when you shouldn’t. Knowing about urinary problems helps us find better treatments.
In short, urinary issues can really change someone’s life. By understanding why they happen, we can help people feel better and live better lives.
TURP: The Traditional Effective Remedy For Urinary Problems
TURP, or Transurethral Resection of the Prostate, is a common surgery for urinary issues caused by an enlarged prostate. Our team has a lot of experience with TURP, having done many successful surgeries. This surgery helps men with Benign Prostatic Hyperplasia (BPH), where the prostate gets too big and blocks urine flow.
Understanding Transurethral Resection of the Prostate
Transurethral Resection of the Prostate removes prostate tissue that blocks urine. It’s done through the urethra, so no big cuts are needed. We use the latest tools and methods to be precise and avoid problems. The goal is to fix urine flow, reduce BPH symptoms, and lower the risk of complications.

The TURP Procedure: A Step-by-Step Guide
The TURP procedure is done under anesthesia to keep the patient comfortable. Here’s what happens:
- A resectoscope is inserted through the urethra to the prostate.
- The resectoscope has a loop that cuts away extra prostate tissue with electricity.
- The cut tissue is then flushed out through the resectoscope.
- The whole thing usually takes about 90 minutes, depending on the prostate size and tissue amount.
We watch the patient’s vital signs closely during the surgery. We make sure it’s done carefully and precisely.
Recovery Timeline and Expected Outcomes
After TURP surgery, patients usually stay in the hospital for a day or two. The catheter comes out a few days later. Most men see big improvements in their urine issues within a few weeks.
Things like age, health, and infections before surgery can affect recovery and results. We tell patients to avoid hard work for a few weeks to heal right. Our team gives detailed care instructions to help with recovery.
Good results from TURP include better urine flow, less need to pee, and fewer BPH symptoms. While results can differ, TURP often works well to solve urinary problems.
Alternative Surgical Interventions for Urinary Difficulties
When traditional TURP isn’t the best option, there are other ways to help with urinary problems. Every person’s situation is different. So, it’s important to look at all the options available.
Prostatic Urethral Lift: A Minimally Invasive Option
The Prostatic Urethral Lift (PUL) is a minimally invasive procedure that’s becoming popular. It treats benign prostatic hyperplasia (BPH) by lifting prostate tissue away from the urethra. This improves urine flow without removing tissue.
Studies show PUL can lead to up to 88.4% of patients not needing a catheter by 90 days after surgery. This makes it a good choice for those wanting to recover quickly.
PUL also has the advantage of possibly preserving sexual function. It reduces the risk of complications from more invasive surgeries. So, it’s a strong alternative to traditional TURP for many patients.
Laser Prostatectomy Techniques
Laser prostatectomy techniques are another big step forward in treating urinary issues. These methods use laser energy to remove or reduce prostate tissue. This improves urine flow.
The precision of laser surgery can mean fewer complications and less bleeding than traditional surgery.
- HoLEP (Holmium Laser Enucleation of the Prostate) is a highly effective technique that allows for the removal of prostate tissue with minimal bleeding.
- GreenLight Laser Therapy is another popular option that vaporizes obstructing prostate tissue, providing quick relief from urinary obstruction.
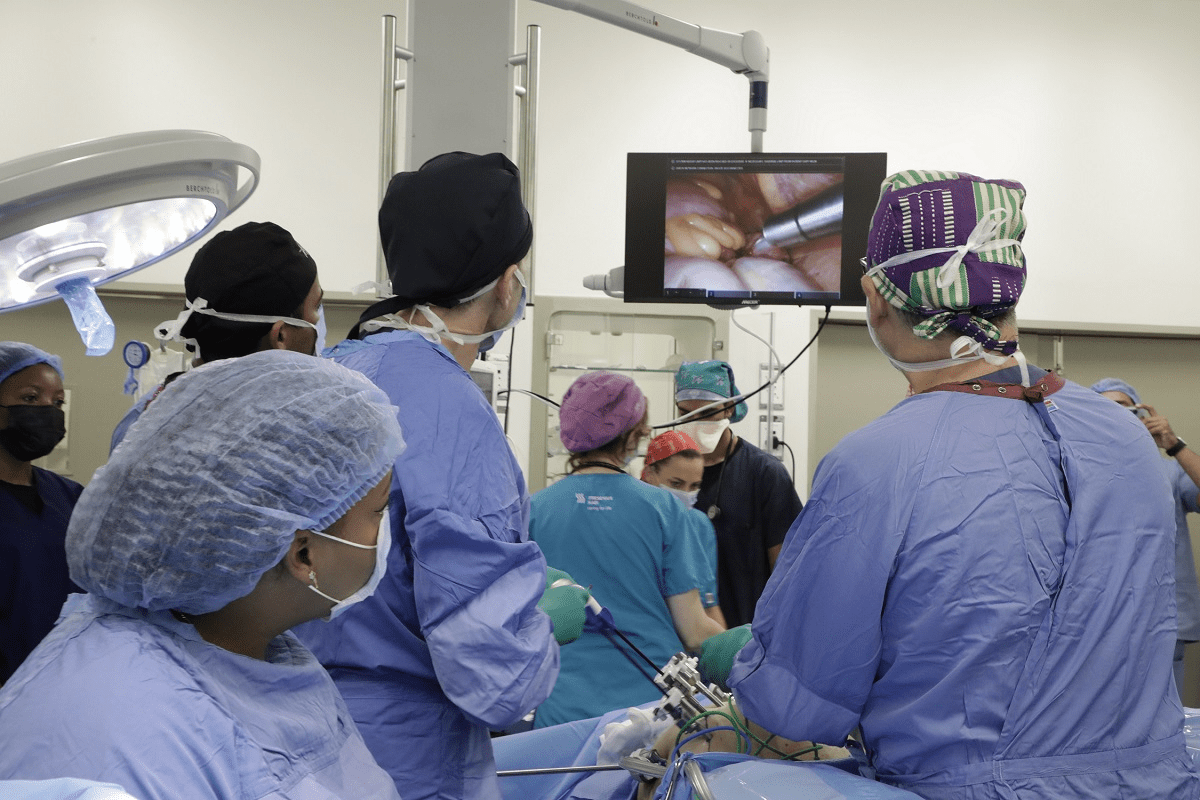
Open and Robotic Prostatectomy Approaches
In some cases, open or robotic prostatectomy may be recommended. This is for patients with more complex conditions or larger prostates. These surgeries remove the prostate gland or parts of it, relieving urinary obstruction.
Robotic prostatectomy offers the benefits of minimally invasive surgery. This includes less pain, shorter hospital stays, and quicker recovery times. The precision of robotic-assisted surgery can also lead to better outcomes and fewer complications.
As we continue to advance in the field of urology, it’s essential to consider the range of surgical options available for treating urinary difficulties. By understanding the benefits and risks of each procedure, we can work together to determine the best course of treatment for each individual patient.
Critical Factors Affecting Surgical Outcomes
Many factors influence the success of surgeries for urinary problems. Knowing these factors is key to better patient care and outcomes.
Timing of Surgery: Why Prompt Intervention Matters
The timing of surgery is very important for urinary issues. Waiting too long can increase risks like urinary tract infections and kidney damage. Quick action can lower these risks and improve results.
For example, urethroplasty works better when done quickly. Delaying surgery can make conditions worse, making the surgery harder.
Patient-Specific Risk Factors
Each patient’s health affects surgery success. Age, overall health, and other conditions can impact results. Older patients or those with health issues may face more risks.
Knowing a patient’s risks helps doctors plan better. This might mean improving health before surgery, choosing the right technique, and careful care after. The term “op meaning” in medicine highlights the importance of understanding the surgical plan for each patient.
Managing Postoperative Urinary Retention
Postoperative urinary retention (POUR) is a common issue after surgery, affecting 6.9“9.2% of patients. It’s important to manage POUR to avoid infections and longer hospital stays. Doctors use urinary catheters and other strategies to prevent it.
In some cases, using roto (a specific device or technique) may help manage POUR. Understanding and managing POUR risks can improve patient care and outcomes.
Conclusion: Advances in Urinary Surgery Care
Advances in urinary surgery care have greatly improved patient results. We aim to offer top-notch healthcare with full support for international patients. At Liv Hospital, we use the latest research and team care to achieve the best surgical results worldwide.
Various surgeries, like TURP and laser prostatectomy, are effective for urinary issues. By knowing the causes of blockages and choosing the right surgery, we help patients get better. Understanding the patient’s situation and the meaning of any blockage is key to the best treatment.
Our team focuses on personalized care and support. We ensure patients get the best results. By leading in urinary surgery care, we keep improving patient outcomes and setting new healthcare standards.
FAQ
What is TURP and how does it help with urinary difficulties?
TURP stands for Transurethral Resection of the Prostate. It’s a surgery that removes extra prostate tissue. This helps improve urine flow and solve urinary problems. It’s a common treatment for Benign Prostatic Hyperplasia (BPH).
What are the benefits of semen retention?
Semen retention is thought by some to have health benefits. But, its direct link to TURP or urinary surgery is not widely discussed in medicine. Some practices related to semen retention might be talked about in terms of prostate health.
What does “bore” mean in a medical context?
In medicine, “bore” means to make a hole or cavity in a body part. This is seen in surgeries. But, it’s not a term used in TURP or urinary issues.
What is the meaning of “turbo cancer”?
“Turbo cancer” is not a term used in medicine. It might refer to aggressive or fast-growing cancers. But, without a clear definition, it’s hard to give a precise answer.
How does the TURP procedure work?
The TURP procedure removes extra prostate tissue that blocks urine flow. It’s done through the urethra, without any external cuts.
What is the recovery timeline after a TURP procedure?
Recovery from TURP varies. Patients usually stay in the hospital for a few days. It can take several weeks for full recovery and normal urine function.
What are the alternative surgical interventions for urinary difficulties?
Alternatives to TURP include Prostatic Urethral Lift, Laser Prostatectomy, and Open or Robotic Prostatectomy. These options treat urinary blockage in different ways, with their own benefits and risks.
What is a Prostatic Urethral Lift?
Prostatic Urethral Lift is a less invasive procedure. It lifts or repositions prostate tissue to improve urine flow. It’s for men with BPH who want to avoid big surgeries.
What does “op” mean in medical terminology?
“Op” is short for “operation” or “operative,” meaning a surgical procedure. In TURP or other surgeries, it refers to the surgery itself.
What are the risks associated with TURP and other prostate surgeries?
Risks include bleeding, infection, urinary incontinence, and erectile dysfunction. The risks and their chances vary by procedure and patient.
What is the meaning of “strenuous” in a medical context?
In medicine, “strenuous” means activities that need a lot of energy or effort. Patients are told to avoid these after surgery to help recover.
What is “terf” meaning, and is it related to medical terminology?
“Terf” is not a medical term and is not related to urinary surgery or TURP. It has other meanings outside of medicine.
How does managing postoperative urinary retention impact surgical outcomes?
Managing postoperative urinary retention is key for good surgical results. It ensures patients can urinate properly after surgery. This helps avoid complications and aids in recovery.
Reference
- Roehrborn, C. G. (2008). Benign prostatic hyperplasia: An overview. Reviews in Urology, 10(Suppl 1), S3“S14. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2719468/
- Foster, H. E., Barry, M. J., Dahm, P., Gandhi, M., Kaplan, S. A., Kohler, T. S., … & Wilt, T. J. (2018). Surgical management of lower urinary tract symptoms attributed to benign prostatic hyperplasia: AUA guideline. The Journal of Urology, 200(3), 612“619. https://www.auajournals.org/doi/10.1016/j.juro.2018.05.029
- Reich, O., Gratzke, C., & Stief, C. G. (2008). Techniques and long-term results of surgical procedures for BPH. European Urology, 53(1), 121“131. https://www.sciencedirect.com/science/article/pii/S0302283807002566
- McVary, K. T. (2017). Surgical management of benign prostatic hyperplasia: Current techniques and outcomes. World Journal of Urology, 35(4), 579“585. https://link.springer.com/article/10.1007/s00345-017-2044-3