Knowing what’s normal for endometrial thickness in premenopausal women is key. It helps tell the difference between normal changes and health problems. The lining of the uterus changes a lot during the menstrual cycle. This is all thanks to hormones like estrogen and progesterone thickened heterogeneous endometrium.
At Liv Hospital, we know how important it is to check endometrial thickness right. We use the latest in diagnostic imaging. This, along with caring for each patient, helps us give clear answers about endometrial health.
Key Takeaways
- Normal endometrial thickness varies throughout the menstrual cycle.
- Understanding these variations is key to identifying possible issues.
- Premenopausal women experience cyclic changes in endometrial thickness.
- Liv Hospital offers advanced diagnostic imaging for accurate assessment.
- Patient-centered care is our priority at Liv Hospital.
Understanding the Endometrium and Its Function
To grasp the importance of endometrial lining thickness in premenopausal women, we need to know about the endometrium. This tissue is complex and vital for women’s reproductive health.
Anatomy of the Endometrium
The endometrium has two layers: the basal and the functional. The basal layer helps the functional layer grow back. The functional layer changes with hormones, thickening for pregnancy and shedding if not.
Physiological Role in Reproductive Health
The endometrium’s main job is to support a fertilized egg. Its thickness and structure are key for early pregnancy. It must be thick and mature for successful implantation. The endometrium changes with hormones, getting ready for pregnancy.
The Menstrual Cycle and Endometrial Changes
During a woman’s menstrual cycle, the endometrium changes a lot. These changes help get the uterus ready for a baby.
Hormonal Regulation of the Endometrium
Two hormones, estrogen and progesterone, control the endometrium. Estrogen makes it grow in the first half of the cycle. Progesterone gets it ready for a fertilized egg by keeping it thick and active.
These hormones change a lot during the cycle. Estrogen goes up first, making the endometrium thicker. Then, after ovulation, progesterone increases, getting it even more ready for a baby.
Cyclic Endometrial Remodeling
The endometrium changes a lot during the cycle. At the start, it’s 1-4 mm thick. As the cycle goes on, it gets thicker, up to 16 mm in the secretory phase.
This constant change is key for reproductive health. It lets the uterus get ready for a baby or shed the lining if there isn’t one.
Impact of Age on Endometrial Thickness
Age affects how thick the endometrium is. In younger women, it changes with the cycle. But as women get older, it gets thinner because of less estrogen.
Doctors need to know about these changes to check endometrial health. This helps them make better care plans for their patients.
Normal Endometrial Thickness Measurements
Knowing what’s normal in endometrial thickness is key for spotting issues in premenopausal women. The endometrium’s thickness changes throughout the menstrual cycle. It’s vital to know these changes for correct diagnosis and treatment.
Statistical Ranges in Premenopausal Women
Studies show the median endometrial thickness in premenopausal women is about 8.6 mm. The 90% and 95% quantiles are 13.8 mm and 15.8 mm, respectively. These numbers help define what’s considered normal.
Quantile | Endometrial Thickness (mm) |
Median | 8.6 |
90% | 13.8 |
95% | 15.8 |
Factors Affecting Measurement Accuracy
Several things can make endometrial thickness measurements less accurate. These include the measurement technique, the quality of the ultrasound equipment, and the practitioner’s skill.
- Technique: The angle and position of the ultrasound probe greatly affect accuracy.
- Equipment Quality: Better ultrasound equipment leads to more accurate measurements.
- Practitioner Skill: More experienced practitioners tend to get more reliable results.
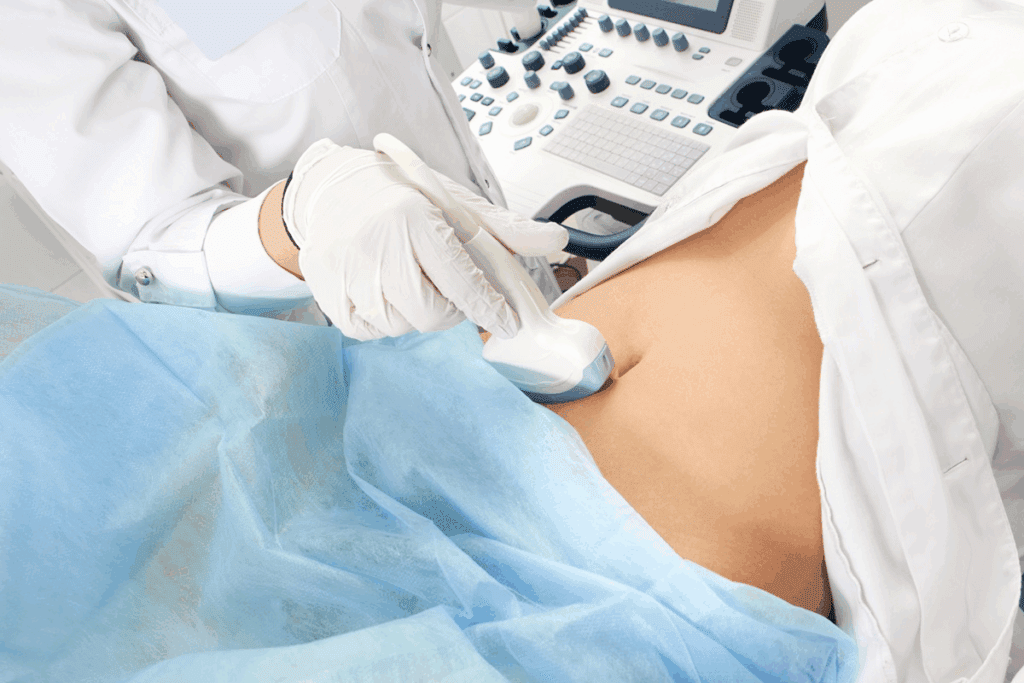
Ultrasound Techniques for Endometrial Assessment
Ultrasound is the main way to check endometrial thickness. Transvaginal ultrasound is best for getting clear images of the endometrium.
Understanding normal endometrial thickness and what can affect measurements helps healthcare providers. They can then make better diagnoses and treatment plans.
Endometrial Thickness During Menstruation
The endometrium is at its thinnest during the menstrual period. This is a normal part of the cycle. It prepares the uterus for a new cycle of pregnancy.
Expected Measurements
During menstruation, the endometrial thickness is usually between 1-4 mm. This is considered normal. It shows the shedding of the endometrial lining during this phase.
Clinical Significance of Thin Endometrium
A thin endometrium during menstruation is usually not a concern. It’s a normal part of the cycle. But, an unusually thin endometrium might hint at reproductive health issues.
The following table summarizes the expected endometrial thickness during menstruation:
Phase | Normal Endometrial Thickness |
During Menstruation | 1-4 mm |
Knowing the normal range of endometrial thickness during menstruation is key. Any big changes might need a doctor’s check-up.
Proliferative Phase Endometrial Thickness
As the menstrual cycle moves into the proliferative phase, the endometrium starts to grow. This is in preparation for ovulation. It’s a key time for the uterus to get ready for a possible pregnancy.
Early Proliferative Phase
In the early proliferative phase, the endometrium starts to grow back and get thicker. It usually measures between 5 to 7 mm. This is when the body starts to get ready for ovulation.
Late Proliferative Phase
As we get closer to ovulation in the late proliferative phase, the endometrium can grow up to 11 mm. This big increase is important for making a good place for the embryo to implant.
The thickness of the endometrium during ovulation is very important for reproductive health. It needs to be thick enough for the embryo to implant successfully.
To understand the changes in endometrial thickness during the proliferative phase, let’s look at the following table:
Phase | Endometrial Thickness | Characteristics |
Early Proliferative | 5-7 mm | Regeneration begins, gradual thickening |
Late Proliferative | Up to 11 mm | Significant growth, preparation for ovulation |
We see that the endometrial thickness grows a lot as the proliferative phase goes on. This growth is essential for a healthy reproductive cycle.
Key factors influencing endometrial thickness include hormonal changes, like the rise in estrogen levels during the proliferative phase. Knowing about these changes helps us understand reproductive health better.
Secretory Phase and Maximum Endometrial Thickness
The endometrium gets its thickest during the secretory phase. This is key for implantation. It happens after ovulation and is fueled by progesterone. This hormone makes the endometrium thicker and more vascular.
The endometrium can grow up to 18mm thick in this phase. This prepares the uterus for a possible pregnancy. An endometrial thickness of 12mm is often enough for implantation.
Peak Thickness Measurements
The endometrium’s peak thickness varies among women. It usually ranges from 8mm to 18mm in the secretory phase. An 8mm endometrium thickness is seen as the minimum for successful implantation.
Here’s a table showing normal endometrial thickness during the secretory phase:
Phase | Typical Thickness Range |
Early Secretory | 8-12mm |
Late Secretory | 12-18mm |
Physiological Variations Among Women
Endometrial thickness varies a lot among women. Age, hormonal balance, and reproductive health play a role. These factors can affect how thick the endometrium gets.
Some women might have a 12mm or more endometrial thickness. Others might have about 8mm. Both can be normal, depending on individual factors.
Thickened Heterogeneous Endometrium: When to Be Concerned
A thickened or heterogeneous endometrium on ultrasound can cause worry. It’s important to understand when this is a sign of something serious. We’ll look at what makes it abnormal, possible causes, and what it means for your health.
Defining Abnormal Endometrial Thickness
What’s considered abnormal endometrial thickness varies with the menstrual cycle. In the proliferative phase, more than 14 mm is usually a red flag. For the secretory phase, over 18 mm is concerning. But, these numbers can change based on many factors and the situation.
Several things affect what’s seen as abnormal thickness. These include:
- Age and whether you’re menopausal
- Any unusual bleeding from the uterus
- Details seen on the ultrasound, like heterogeneity and masses
Causes of Endometrial Thickening
There are many reasons for endometrial thickening, from normal changes to serious problems. Some common reasons include:
- Hormonal Imbalances: Too much estrogen, like in PCOS, can cause thickening.
- Endometrial Hyperplasia: This is when the endometrium grows too much, often due to hormones.
- Endometrial Polyps: These are benign growths that can make the endometrium thicker.
- Adenomyosis: When endometrial tissue grows into the muscle wall, causing thickening.
- Malignancy: In some cases, thickening can be a sign of endometrial cancer, more common in postmenopausal women.
A thickened or inhomogeneous endometrium on ultrasound needs more checking. We must find out why it’s happening and how to treat it.
Diagnostic Approaches for Abnormal Endometrial Findings
When we find abnormal endometrial thickness or heterogeneity, we need to check further. This is to find out what’s causing it.
Follow-up Imaging Studies
Follow-up imaging studies are key for watching abnormal endometrial findings. Transvaginal ultrasound is often used. It helps measure endometrial thickness and check its texture.
In some cases, we might suggest saline infusion sonography (SIS) or magnetic resonance imaging (MRI). These help give more detailed info about the endometrium.
Endometrial Sampling Techniques
Endometrial sampling is a vital tool for checking abnormal findings. Methods like endometrial biopsy or dilation and curettage (D&C) help get tissue samples. These are then checked under a microscope.
- Endometrial biopsy is a simple procedure done in an outpatient setting.
- D&C is more invasive and done under anesthesia. It allows for a deeper look at the endometrium.
When to Seek Medical Attention
Women should see a doctor if they have abnormal uterine bleeding, pelvic pain, or unusual ultrasound results.
Early diagnosis is key to managing abnormal endometrial findings well. We advise women to talk to their healthcare provider. They can decide the best steps based on the woman’s needs and risks.
Conclusion
Knowing about endometrial thickness is key for keeping reproductive health in check, mainly for premenopausal women. We’ve looked into the usual thickness of the endometrium at different times in the menstrual cycle. We’ve also talked about what can make measuring thickness tricky.
Thickening of the endometrium before menopause is a big deal for reproductive health. Knowing what’s normal can help spot problems early. It’s important to know when to get more tests to manage and treat issues quickly.
By understanding normal and abnormal endometrial thickness, women and doctors can tackle any issues together. Regular health checks and screenings are essential to keep an eye on endometrial health. This way, any problems can be caught and fixed right away.
FAQ
What is considered a normal endometrial thickness in premenopausal women?
In premenopausal women, endometrial thickness changes throughout the cycle. It starts at 1-4mm during menstruation. It can grow up to 18mm during the secretory phase.
How does endometrial thickness change throughout the menstrual cycle?
Endometrial thickness grows with hormonal changes. It starts at 1-4mm during menstruation. It then grows to 5-7mm in the early proliferative phase. It can reach up to 11mm in the late proliferative phase. It peaks at up to 18mm during the secretory phase.
What is the significance of a thin endometrium during menstruation?
A thin endometrium during menstruation is usually normal. But, it might be linked to reproductive issues. These include trouble conceiving or a higher risk of miscarriage.
What factors can affect the accuracy of endometrial thickness measurements?
Several factors can impact measurement accuracy. These include the quality of the ultrasound image and the operator’s skill. Uterine abnormalities or other conditions can also distort the endometrium.
When is a thickened or heterogeneous endometrium considered abnormal?
A thickened or heterogeneous endometrium is abnormal if it’s outside the expected range for the menstrual cycle stage. It’s also abnormal if it’s linked to symptoms like abnormal bleeding or pelvic pain.
What are the possible causes of endometrial thickening?
Endometrial thickening can be caused by hormonal imbalances, endometrial hyperplasia, polyps, and cancer. Other conditions can also cause it.
What diagnostic approaches are used to evaluate abnormal endometrial findings?
To evaluate abnormal findings, doctors use follow-up imaging studies. These include ultrasound or MRI. They also use endometrial sampling techniques like biopsy or dilation and curettage.
When should I seek medical attention for concerning symptoms or findings related to endometrial thickness?
Seek medical attention for abnormal bleeding, pelvic pain, or other concerning symptoms. Also, if your healthcare provider finds an abnormality on ultrasound or other imaging studies.
What is the role of ultrasound in assessing endometrial thickness?
Ultrasound is a non-invasive imaging technique. It’s used to assess endometrial thickness and detect abnormalities like thickening or heterogeneity.
Can age impact endometrial thickness?
Yes, age can affect endometrial thickness. Hormonal changes and reproductive status with age influence endometrial thickness measurements.
What is considered a normal endometrial thickness during the proliferative phase?
During the proliferative phase, normal endometrial thickness is 5-7mm in the early phase. It can reach up to 11mm in the late phase.
What is inhomogeneous endometrium?
Inhomogeneous endometrium means the endometrium looks uneven or irregular on ultrasound. It can be normal or a sign of an underlying condition.
Is an endometrial thickness of 6mm or 8mm considered normal?
An endometrial thickness of 6mm or 8mm can be normal. It depends on the menstrual cycle stage and individual factors.
What is the normal range for endometrial thickness in perimenopause?
In perimenopause, the normal range for endometrial thickness varies. It’s similar to premenopausal women, but hormonal changes can cause some variations.
References
National Center for Biotechnology Information. Normal Endometrial Thickness: Ultrasound Measurement Interpretation. Retrieved from https://pmc.ncbi.nlm.nih.gov/articles/PMC5768977/








