At Liv Hospital, we know how important it is to spot cardiac problems right away. Complete 3rd degree AV block is a serious issue where the heart’s electrical signals don’t talk to each other. This means someone needs help fast.
It’s key to know the 7 main signs of a third heart block ECG. Our team is skilled in finding these signs. We focus on our patients, making sure they get the best care. We also help patients from other countries with our top-notch services.
Knowing about 3rd degree heart block helps doctors make quick, smart choices. This can save lives.
Key Takeaways
- Complete 3rd degree AV block is a serious cardiac condition requiring urgent attention.
- Liv Hospital’s expertise is key in spotting the 7 main signs of third heart block ECG.
- Getting the diagnosis right is vital for top-notch heart care.
- We put our patients first, helping international patients with full care.
- Spotting third-degree AV block is critical for quick medical help.
What Is Third Degree Heart Block?
Third-degree atrioventricular (AV) block is a serious heart issue. It happens when electrical signals from the atria can’t reach the ventricles. This causes a complete break between the atrial and ventricular beats, which is very dangerous if not treated quickly.
Definition and Basic Concepts
Third-degree heart block, or complete AV block, means the electrical system between the atria and ventricles doesn’t work. The atria and ventricles beat on their own. The atria are controlled by the sinoatrial (SA) node, and the ventricles by an escape pacemaker. Doctors use an electrocardiogram (ECG) to spot this, showing AV dissociation.
Prevalence and Clinical Significance
Third-degree AV block is rare but very urgent. It’s more common with age, mainly in those with heart disease. It’s serious because it can lead to slow heart rate, heart failure, and even sudden death if not treated.
It’s key for doctors to know about third-degree heart block. They need to spot and treat it fast to help patients. Quick action can make a big difference in recovery.
Pathophysiology of Complete AV Block
The cardiac conduction system’s complex workings are disrupted in complete AV block. This leads to significant clinical effects. To grasp this condition, we must first look at the normal cardiac conduction system and how complete AV block impacts it.
Normal Cardiac Conduction System
The normal cardiac conduction system is a complex network. It includes the sinoatrial (SA) node, atrioventricular (AV) node, and the His-Purkinje system. The SA node acts as the heart’s natural pacemaker, sending electrical impulses to the AV node.
These impulses then travel to the ventricles through the His-Purkinje system. This coordinated electrical activity ensures the atria and ventricles contract in sync. This is key for efficient heart function.
Mechanism of Conduction Failure
In complete AV block, electrical impulses from the atria to the ventricles are completely blocked. This can happen due to various reasons, like degenerative changes or ischemic damage. It can also be caused by certain medications.
As a result, the atria and ventricles beat independently. This loss of coordinated contractions is a major issue. The ventricles often use a subsidiary pacemaker to maintain a rate.
Anatomical Locations of Block
Complete AV block can occur at different spots in the conduction system. These include:
- The AV node
- The Bundle of His
- The bundle branches
Knowing where the block is helps figure out the cause and how to manage it.
Understanding the pathophysiology of complete AV block is key. It helps us interpret ECG findings and develop the right treatment plans.
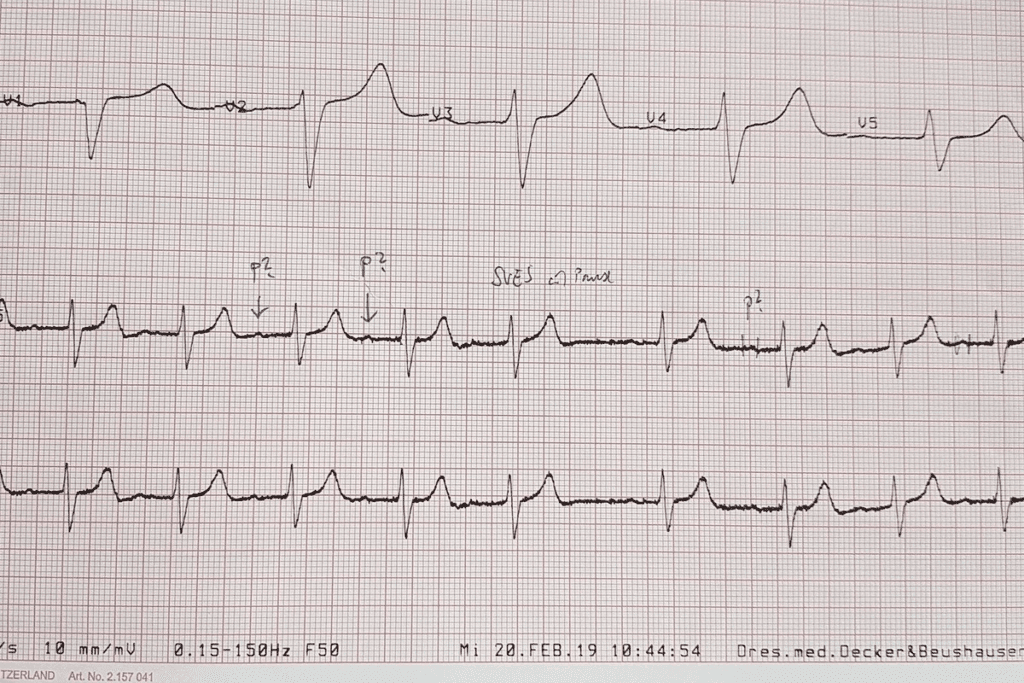
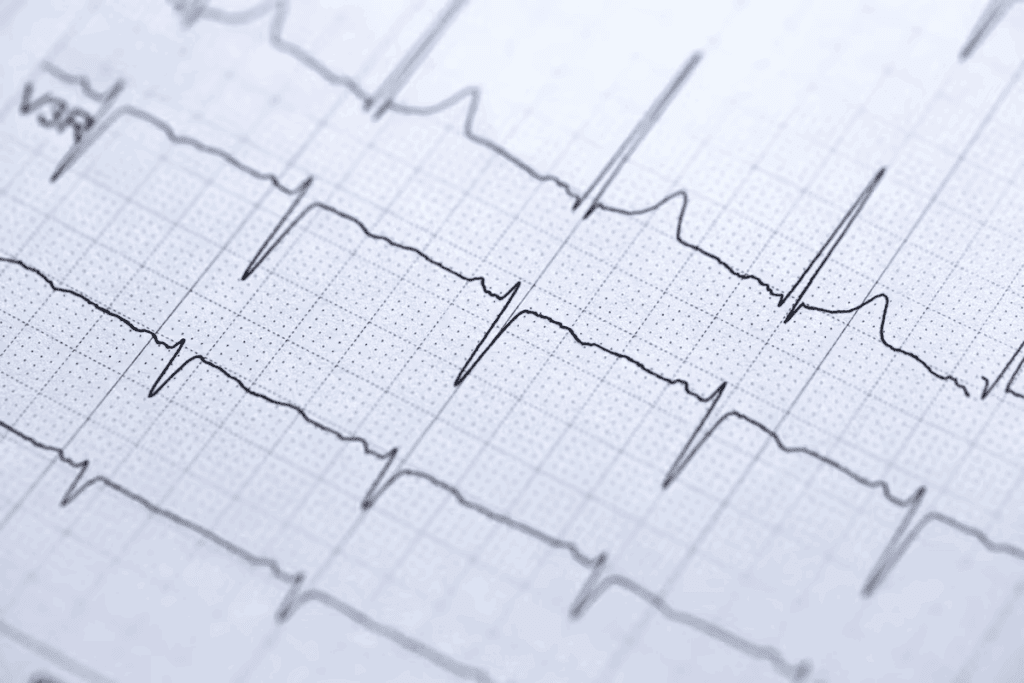
Third Heart Block ECG: Diagnostic Criteria
Spotting third-degree heart block on an ECG means looking for no coordination between heart beats. This issue stops the heart’s normal rhythm, showing clear signs on an ECG.
Complete AV Dissociation
Third-degree heart block is marked by complete AV dissociation. This means the heart’s upper and lower chambers beat on their own. On an ECG, you’ll see P waves and QRS complexes that don’t match up.
“In third-degree AV block, the atria and ventricles beat independently, resulting in a loss of synchrony between the P waves and QRS complexes,” as noted by cardiology experts. This dissociation is a key sign.
P Wave and QRS Relationship
Normally, P waves lead to QRS complexes on an ECG, showing the signal’s path. But in third-degree heart block, P waves and QRS complexes don’t follow each other. This happens because the electrical signal is blocked at the AV node.
Rhythm Pattern Recognition
Spotting the rhythm is key to diagnosing third-degree heart block. The ECG will show regular intervals for P and R waves. Yet, the P waves and QRS complexes won’t be linked. This creates a unique “dissociated” rhythm that points to third-degree AV block.
Knowing these signs helps doctors spot third-degree heart block on an ECG. They can then take the right steps to manage it.
7 Key Features on 3rd Degree Block ECG Strips
It’s important to know the 7 key features of 3rd degree block ECG strips for accurate diagnosis. Third degree heart block, or complete AV block, stops electrical signals between the atria and ventricles. This leads to unique ECG patterns that help doctors diagnose the condition.
Independent Atrial and Ventricular Rates
One key sign of third degree heart block on an ECG is independent atrial and ventricular rates. The atria beat faster than the ventricles, and they beat on their own.
Regular PP and RR Intervals
Even with the blockage, both atrial and ventricular rhythms stay regular. This means the time between P waves (PP intervals) and QRS complexes (RR intervals) stays the same.
More P Waves Than QRS Complexes
On a 3rd degree block ECG strip, you’ll see more P waves than QRS complexes. This is because the atrial rate is higher than the ventricular rate. This is a key difference from other AV block types.
Variable PR Intervals
The PR interval, from the start of the P wave to the QRS complex, changes because of the independent rhythms. This change is a key sign that the AV node isn’t working right.
Other important features include no consistent P wave to QRS complex relationship, a ventricular rate of 40-60 bpm, and a ventricular escape rhythm. Spotting these signs on an ECG is critical for diagnosing third degree heart block and deciding on treatment.
Junctional Escape Rhythm in Third Degree AV Block
In third-degree AV block, the heart’s electrical system is badly damaged. This often leads to a junctional escape rhythm. This rhythm is vital for keeping the heart working when normal electrical signals are blocked.
Narrow QRS Complex Characteristics
A junctional escape rhythm has narrow QRS complexes. This shows that the heart’s ventricles are activated through the normal electrical pathway. This narrow QRS is key to telling junctional rhythms apart from ventricular ones, which have wider QRS complexes.
Typical Rate of 40-60 BPM
The heart rate in a junctional escape rhythm is usually between 40 to 60 beats per minute. This rate is faster than a ventricular escape rhythm but slower than a normal heart rate. The stable rate of a junctional escape rhythm is important for keeping the heart pumping well in third-degree AV block.
Stability and Reliability Factors
Many things affect how stable and reliable a junctional escape rhythm is. These include the cause of the third-degree AV block, any heart disease, and the patient’s overall health. Key factors that help keep junctional escape rhythms stable include:
- The health of the AV node and surrounding tissue
- Any imbalances in electrolytes or medications that could affect heart signals
- The patient’s overall health and ability to handle the changed heart rhythm
It’s important to understand junctional escape rhythms in third-degree AV block for diagnosis and treatment. By knowing the signs of this rhythm, doctors can decide if patients need treatments like pacing.
Ventricular Escape Rhythms and Their Implications
Ventricular escape rhythms are a big deal when the heart’s main pacing system fails. This happens when the AV node can’t send signals. Then, the heart starts beating on its own, but not very well.
Wide QRS Complex Features
Ventricular escape rhythms show up as wide QRS complexes, bigger than 120 ms. This is because the heart’s ventricles start the beat. A doctor said, “The wide QRS complex is a sign of a serious heart problem that needs quick action.”
Slower Rates and Hemodynamic Impact
These rhythms make the heart beat slower, between 20-40 beats per minute. This can cause big problems like dizziness and fatigue. A study found, “The slow heart rate can really affect how well the heart works.”
Risk of Rhythm Failure
Ventricular escape rhythms can fail, leading to heart rate problems. This is a big worry, as it can happen when the heart is stressed or with some medicines. It’s important to watch them closely and act fast if needed.
We need to remember that ventricular escape rhythms are not okay. They need careful watching to avoid serious issues.
Causes and Clinical Contexts
Knowing why third-degree heart block happens is key to treating it well. This condition stops electrical signals between the heart’s chambers. It can cause slow heart rates and serious health risks.
Acute Myocardial Infarction
Heart attacks are a big reason for third-degree heart block. When a heart attack happens, blood flow to the heart stops. This can harm the heart’s electrical system. About 5-8% of heart attack patients get third-degree heart block.
Degenerative Conduction Disease
Degenerative conduction disease also leads to third-degree heart block. It’s when the heart’s electrical system gets worse over time, often due to aging. As more people get older, this problem will likely become more common.
Medication-Induced AV Block
Some medicines can cause third-degree heart block by affecting the heart’s rhythm. Drugs like beta-blockers and certain anti-arrhythmics can slow the heart too much. It’s important to watch patients on these medicines closely.
Other Etiologies
Other reasons for third-degree heart block include surgery, infections like Lyme disease, and diseases like sarcoidosis. Congenital heart disease can also cause it, either at birth or later.
| Cause | Description | Clinical Context |
| Acute Myocardial Infarction | Damage to the heart muscle due to blocked blood flow | Emergency setting, high-risk patients |
| Degenerative Conduction Disease | Progressive deterioration of the heart’s electrical system | Aging population, chronic management |
| Medication-Induced AV Block | Certain drugs affecting the heart’s conduction | Patients on beta-blockers, calcium channel blockers |
| Other Etiologies | Includes cardiac surgery, infections, and infiltrative diseases | Varies depending on the underlying cause |
In conclusion, third-degree heart block can come from many health issues. Doctors need to understand these causes to treat it well and help patients get better.
Emergency Management and Treatment
Managing third-degree heart block is a complex task. It involves many steps to keep the patient stable and prevent more problems. Quick action is key to better results.
Immediate Interventions
The first thing to do is check if the patient is stable. Patients with serious bradycardia or symptoms need fast help. Atropine might be given, but it works differently for everyone.
Temporary Pacing Techniques
Temporary pacing is a big help for third-degree heart block. There are two main ways: transcutaneous pacing and transvenous pacing. Transcutaneous pacing is easy and quick, but transvenous pacing is more stable.
Indications for Permanent Pacemaker
Most people with third-degree heart block need a permanent pacemaker. The choice depends on the cause, symptoms, and the patient’s health.
Medication Management
While waiting for pacing, medicines like atropine or isoproterenol can help raise the heart rate. But, they’re not a permanent fix.
| Treatment Option | Indications | Benefits |
| Atropine | Symptomatic bradycardia | Temporary increase in heart rate |
| Transcutaneous Pacing | Significant bradycardia, hemodynamic instability | Rapid, non-invasive pacing |
| Permanent Pacemaker | Third-degree heart block with symptoms or significant bradycardia | Long-term rhythm stabilization |
Handling third-degree heart block well needs a team effort. It includes quick actions, temporary pacing, and sometimes, a permanent pacemaker.
Conclusion
Third degree heart block, also known as complete 3rd degree AV block, is a serious heart condition. It happens when the heart’s electrical signals from the atria and ventricles don’t work together. We’ve talked about the main signs seen on an ECG, like different heart rates and regular intervals.
This condition is very serious because it can cause big problems with blood flow and even lead to heart failure. It’s important to treat it quickly to help the patient. Doctors use different methods like temporary pacing, medicine, and sometimes a permanent pacemaker.
To sum up, third degree heart block is a complex issue that needs a deep understanding of its signs, how serious it is, and how to treat it. By knowing these things, doctors can give the right care fast. This helps patients get better and live healthier lives.
FAQ
What is third degree heart block?
Third degree heart block is a serious heart condition. It happens when there’s no connection between the heart’s electrical signals.
What are the ECG characteristics of third degree heart block?
ECG signs of third degree heart block include no connection between heart signals. You’ll see regular heartbeats but not in sync with each other.
How is third degree heart block diagnosed on an ECG?
Doctors use an ECG to spot third degree heart block. They look for no connection between heart signals and check the rhythm.
What is the significance of junctional escape rhythm in third degree AV block?
Junctional escape rhythm is key in third degree AV block. It helps keep the heart rate steady, usually between 40-60 beats per minute.
What are the implications of ventricular escape rhythms in third degree heart block?
Ventricular escape rhythms can affect heart function. They’re slower and may lead to rhythm failure, needing quick medical help.
What are the causes of third degree heart block?
Third degree heart block can be caused by heart attacks, aging, or certain medicines. Other reasons also exist.
How is third degree heart block managed in an emergency setting?
In emergencies, doctors act fast. They use temporary pacing, medicines, and might suggest a permanent pacemaker.
What is the clinical significance of third degree heart block?
Third degree heart block is very serious. It can cause big problems if not treated quickly, making it very important to act fast.
How does third degree AV block affect the cardiac conduction system?
Third degree AV block messes up the heart’s electrical system. It stops the heart’s signals from working together properly.
References:
- Camasão, D. B., & Mantovani, D. (2021). The mechanical characterization of blood vessels and their substitutes in the continuous quest for physiologically relevant performances: A critical review. Mechanics Research Communications, 114, 103655. https://www.sciencedirect.com/science/article/pii/S2590006421000144



































