
Thoracotomy is a surgical procedure involving an incision in the chest to access organs like the lungs or heart. We often encounter questions about how thoracotomy differs from other thoracic or lung surgeries. While both are chest-related procedures, thoracotomy specifically provides direct access for major operations inside the chest cavity.
Key Takeaways
- Thoracic surgery is a broader surgical field that includes operations on various chest organs.
- Lung surgery is a subset of thoracic surgery, focusing specifically on the lungs.
- The scope of thoracic surgery extends to the esophagus, trachea, and other chest structures.
- Advancements in thoracic surgery have improved patient outcomes and recovery times.
- LivHospital is at the forefront of innovative thoracic surgery practices.
The Distinct Fields of Chest Surgery
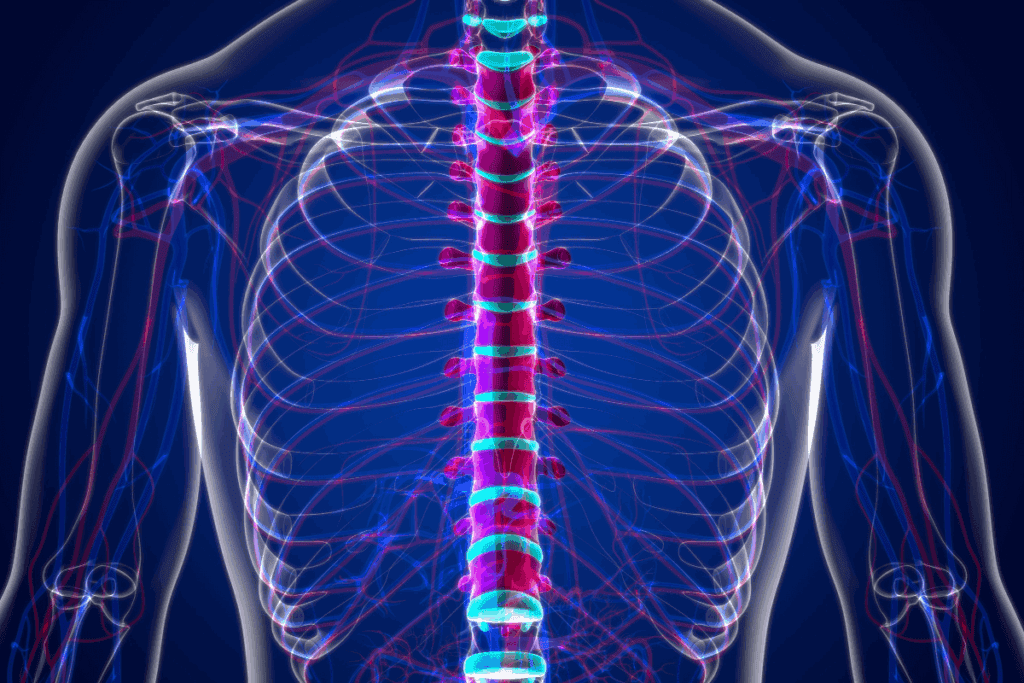
Thoracic surgery and lung surgery, while related, are distinct medical specialties with different focuses. Thoracic surgery encompasses a broad range of surgical procedures involving organs within the chest cavity, including the lungs, heart, esophagus, trachea, and diaphragm.
Defining Thoracic Surgery
Thoracic surgery, as defined by Mercy Health, involves the repair of organs located in the thorax. This includes operations on the heart, lungs, esophagus, trachea, and diaphragm. The scope of thoracic surgery is comprehensive, addressing various conditions that affect these vital organs.
Some key aspects of thoracic surgery include:
- Complex Diagnostic Procedures: Thoracic surgeons perform intricate diagnostic tests to identify conditions affecting the chest organs.
- Treatment of Various Conditions: From lung cancer to esophageal disorders, thoracic surgeons treat a wide range of diseases.
- Minimally Invasive Techniques: The use of thoracoscopic surgery and other minimally invasive methods reduces recovery time and scarring.
Defining Lung Surgery
Lung surgery, a subset of thoracic surgery, specifically focuses on surgical procedures related to the lungs. This includes lung resection, where part of the lung is removed, often due to cancer or other diseases.
Lung surgery is critical for:
- Treating Lung Cancer: Surgical removal of tumors is a primary treatment for lung cancer.
- Addressing Lung Diseases: Conditions like chronic obstructive pulmonary disease (COPD) may require surgical intervention.
- Repairing Lung Damage: Trauma or infection can necessitate surgical repair of lung tissue.
Key Anatomical Differences
The distinction between thoracic and lung surgery lies in the anatomical focus. Thoracic surgery involves a broader range of organs within the chest, while lung surgery is specialized to the lungs. Understanding these differences is crucial for both surgeons and patients to ensure appropriate care.
Key anatomical differences include:
- Organ Involvement: Thoracic surgery includes operations on multiple chest organs, not just the lungs.
- Surgical Approaches: The surgical techniques and approaches can vary significantly between thoracic and lung surgery.
- Complexity and Specialization: Both fields require specialized training, but thoracic surgery encompasses a wider range of procedures.
The Comprehensive Scope of Thoracic Surgery
Thoracic surgery encompasses a broad range of procedures that extend far beyond lung surgery alone. At UC San Diego Health, our thoracic surgeons perform operations on various organs within the chest cavity, including the lungs, esophagus, trachea, chest wall, diaphragm, and mediastinum.
Organs Treated in Thoracic Surgery
The scope of thoracic surgery is vast, covering a range of procedures on vital structures within the thorax. Our thoracic surgeons are trained to operate on multiple organs and systems, including:
- The esophagus, where conditions like esophageal cancer or achalasia may require surgical intervention.
- The trachea, where procedures might be necessary to address tracheal stenosis or other obstructive conditions.
- The chest wall, where tumors or deformities may need to be corrected surgically.
- The diaphragm, where conditions such as diaphragmatic hernias require repair.
- The mediastinum, where tumors or cysts may necessitate surgical removal.
As noted by a leading thoracic surgeon,
“The complexity and diversity of thoracic surgery require a multidisciplinary approach to patient care.”
Common Non-Lung Thoracic Procedures
Beyond lung surgery, there are several common thoracic procedures that our surgeons perform. These include:
- Esophagectomy for esophageal cancer or severe dysmotility disorders.
- Tracheal resection and reconstruction for tracheal stenosis or tumors.
- Chest wall resections and reconstructions for tumors or deformities.
- Diaphragmatic hernia repairs can be performed using minimally invasive techniques.
- Mediastinal tumor resections often require precise surgical planning.
These procedures highlight the breadth of thoracic surgery and the need for skilled, experienced surgeons who can navigate complex anatomical structures and varied pathological conditions.
Lung Surgery: Specialized Procedures and Indications
Lung surgery is a vital medical specialty that involves various procedures to diagnose and treat lung diseases. We perform these surgeries to address a range of conditions, from lung cancer to chronic obstructive pulmonary disease (COPD).
Major Types of Lung Operations
Lung surgery includes several major types of operations, each with its specific indications and benefits. The most common procedures include:
- Lobectomy: Removing a lobe of the lung, often performed for lung cancer.
- Pneumonectomy: Removing an entire lung, typically done for advanced lung cancer.
- Wedge Resection: Removing a small section of the lung, often used for diagnosing or treating small lung nodules.
Medical Conditions Requiring Lung Surgery
Various medical conditions require lung surgery, including:
- Lung Cancer: Surgery is often the primary treatment for early-stage lung cancer.
- COPD and Emphysema: Surgical interventions like lung volume reduction surgery can help improve symptoms.
- Lung Nodules: Surgery may be necessary to diagnose or remove potentially cancerous nodules.
According to Mercy Health, lung surgery is a critical treatment option for these conditions, offering patients a chance for improved outcomes and quality of life.
Diagnostic vs. Therapeutic Lung Procedures
Lung surgery can be both diagnostic and therapeutic. Diagnostic procedures help identify the nature of lung conditions, while therapeutic procedures aim to treat the disease.
For instance, a wedge resection can be diagnostic by removing a nodule for pathological examination. In contrast, a lobectomy is typically therapeutic, aiming to remove cancerous tissue entirely.
We use advanced diagnostic tools and techniques to determine the most appropriate surgical approach for each patient, ensuring the best possible outcomes.
Thoracotomy: The Traditional Open Chest Approach
The traditional open chest approach, known as thoracotomy, involves a significant incision to access the lungs and other chest organs. This method has been a cornerstone of thoracic surgery for decades, providing surgeons with direct access to the chest cavity.
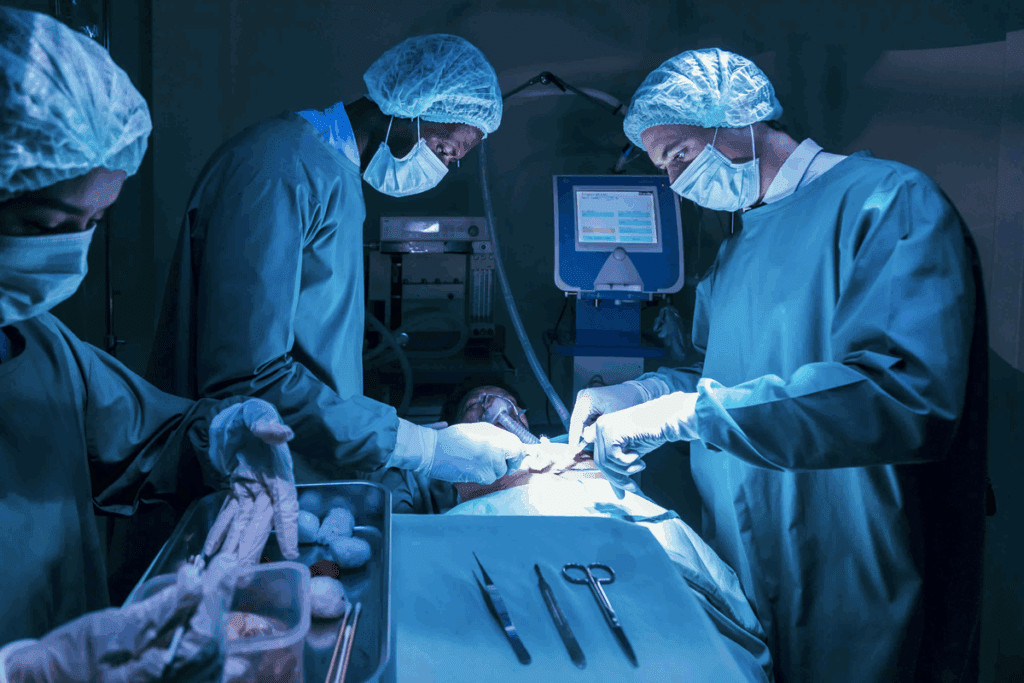
The Surgical Process
During a thoracotomy, the patient is typically placed under general anesthesia to ensure comfort and minimize pain. We make an incision between the ribs, which may involve cutting through some of the muscle tissue to gain access to the chest cavity. The size and location of the incision can vary depending on the specific procedure and the patient’s condition.
Key steps in the thoracotomy procedure include:
- Preparation for surgery, including administering anesthesia and positioning the patient.
- Making the incision and accessing the chest cavity.
- Performing the necessary surgical intervention, such as removing a lung tumor or repairing damaged tissue.
- Closing the incision, which may involve suturing or stapling the tissue.
Indications for Open Thoracotomy
Thoracotomy is often indicated for conditions that require direct access to the lungs or other organs within the chest cavity. Some of the common reasons for performing a thoracotomy include:
- Removing tumors or cancerous tissues from the lungs or surrounding areas.
- Repairing damaged or diseased tissues, such as in cases of traumatic injury.
- Draining fluid or removing infected tissue from the chest cavity.
Recovery Timeline and Considerations
Recovery from a thoracotomy can be a lengthy process, often requiring several weeks to months for full recovery. We emphasize the importance of post-operative care, including pain management and pulmonary rehabilitation, to help patients regain their strength and improve lung function.
Key considerations during recovery include:
- Managing post-operative pain effectively.
- Participating in pulmonary rehabilitation to improve lung function.
- Monitoring for potential complications, such as infection or respiratory issues.
By understanding the process, indications, and recovery requirements for thoracotomy, patients can better prepare themselves for this significant surgical intervention.
Lung Resection Techniques and Their Applications
Lung resection is a critical surgical intervention used to treat various lung conditions, including lung cancer. The type of resection performed depends on the extent and location of the disease. At institutions like UC San Diego Health, various lung resection surgeries are performed, including lobectomy, pneumonectomy, and segmentectomy, using both open and minimally invasive techniques.
Lobectomy: Removing a Lung Lobe
A lobectomy involves the removal of a lung lobe and is one of the most common surgical procedures for lung cancer. “Lobectomy has been shown to offer the best chance of cure for early-stage lung cancer patients,” as noted in surgical oncology guidelines and thoracic surgery practices. We perform lobectomies using both traditional open surgery and minimally invasive techniques, allowing patients to benefit from the most appropriate approach based on their condition.
Pneumonectomy: Complete Lung Removal
In some cases, a pneumonectomy, which involves the removal of an entire lung, is necessary. This procedure is typically performed for more extensive lung cancer or when the disease involves major pulmonary vessels. While it’s a more complex surgery, advancements in surgical techniques have improved outcomes for patients undergoing pneumonectomy.
Segmentectomy and Wedge Resections
For patients with smaller tumors or limited lung function, segmentectomy or wedge resections may be considered. These procedures involve removing the diseased portion of the lung while preserving as much healthy lung tissue as possible. “These conservative resections are crucial for maintaining lung function in patients with limited reserve,” highlighting the importance of tailored surgical approaches. We utilize these techniques to provide the best possible outcomes for our patients.
We understand that each patient’s condition is unique, and the choice of lung resection technique depends on various factors, including the stage and location of the disease, as well as the patient’s overall health. Our team is committed to providing personalized care and utilizing the most appropriate surgical techniques to ensure the best possible outcomes.
Lung Nodule Removal: Procedures and Approaches
The removal of lung nodules is a critical procedure in the diagnosis and treatment of lung cancer. At Mercy Health, we utilize advanced diagnostic tools and minimally invasive surgical techniques for lung nodule removal, ensuring precise and effective care for our patients.
Diagnostic Workup for Lung Nodules
Diagnosing lung nodules involves a comprehensive approach, starting with imaging tests such as CT scans and PET scans. “Early detection of lung nodules is crucial for effective treatment,” emphasizes the importance of thorough diagnostic workup. We employ a range of diagnostic tools to determine the nature of lung nodules, guiding our treatment decisions.
The diagnostic process typically includes:
- Imaging tests (CT scans, PET scans)
- Biopsy procedures
- Review of medical history and risk factors
Surgical Techniques for Nodule Removal
Surgical techniques for lung nodule removal have evolved significantly, with a focus on minimally invasive procedures. Thoracoscopic surgery, also known as VATS (Video-Assisted Thoracoscopic Surgery), is a key approach, offering benefits such as smaller incisions, less pain, and quicker recovery times.
- Lobectomy
- Wedge resection
- Segmentectomy
Post-Surgical Monitoring and Follow-up
After lung nodule removal surgery, careful monitoring and follow-up are essential for ensuring the best outcomes. We provide comprehensive post-surgical care, including pain management and pulmonary rehabilitation programs, to support our patients’ recovery.
“Follow-up care is crucial for detecting any potential recurrence and managing long-term health.” Our team works closely with patients to develop a personalized follow-up plan, addressing their unique needs and concerns.
Minimally Invasive Thoracic Surgery Revolution
Minimally invasive thoracic surgery has revolutionized the field, offering patients less invasive alternatives to traditional open surgery. This shift has significantly impacted patient care, reducing recovery times and complications associated with more invasive procedures.
Video-Assisted Thoracoscopic Surgery (VATS)
Video-Assisted Thoracoscopic Surgery, or VATS, has emerged as a cornerstone of minimally invasive thoracic surgery. This technique involves making small incisions through which a camera and surgical instruments are inserted, allowing surgeons to perform complex procedures with greater precision and less trauma to the patient.
VATS offers several benefits, including reduced postoperative pain, shorter hospital stays, and less risk of complications compared to traditional open thoracotomy. We have seen a significant increase in the adoption of VATS for various thoracic procedures, from lung biopsies to more complex resections.
Robotic-Assisted Thoracic Surgery
Robotic-assisted thoracic surgery represents another significant advancement in the field of minimally invasive surgery. By enhancing the surgeon’s capabilities with robotic technology, we can achieve even greater precision and dexterity during complex procedures.
The robotic system provides high-definition 3D visualization and allows for more intricate dissections, which can be particularly beneficial in delicate areas. While still evolving, robotic-assisted thoracic surgery has shown promising results in improving patient outcomes and expanding the range of minimally invasive options available.
Comparative Outcomes with Traditional Approaches
Studies have shown that minimally invasive techniques like VATS and robotic-assisted surgery compare favorably to traditional open surgery in terms of patient recovery and complication rates. According to recent research, the adoption of these techniques has significantly reduced hospital stays and postoperative complication rates.
By choosing the most appropriate surgical approach for each patient, we can optimize outcomes and improve the quality of care. As technology continues to evolve, we expect to see further advancements in minimally invasive thoracic surgery, leading to even better patient care.
Statistical Landscape of Thoracic Surgery in America
As we examine the statistical landscape of thoracic surgery in America, we uncover trends that are reshaping patient care. The field of thoracic surgery is complex, with a wide range of procedures and techniques being employed across the country.
Annual Procedure Volumes and Trends
The volume of thoracic surgeries performed annually in the U.S. is substantial, with more than 49,000 adult thoracic surgeries taking place every year. This number highlights the importance of thoracic surgery in treating various conditions, including lung cancer and other thoracic diseases.
Recent studies have shown a shift in the types of procedures being performed, with a notable increase in minimally invasive thoracic surgical techniques. This trend is driven by the benefits these techniques offer, including reduced recovery times and fewer complications.
Adoption Rates of Minimally Invasive Techniques
The adoption of minimally invasive techniques, such as Video-Assisted Thoracoscopic Surgery (VATS), has been on the rise. Data indicates that about 33% of non-small cell lung cancer surgeries now utilize VATS, marking a significant shift towards less invasive procedures.
This trend is expected to continue as more surgeons become trained in these techniques and as technology continues to advance. The benefits of minimally invasive surgery, including less pain and shorter hospital stays, are driving this change.
Impact on Hospital Stays and Complication Rates
The impact of these trends on patient outcomes is significant. Studies have shown that patients undergoing minimally invasive thoracic surgery tend to have shorter hospital stays and fewer post-operative complications compared to those undergoing traditional open surgery.
By analyzing these statistics, we can better understand the current state of thoracic surgery in America and anticipate future developments in the field. As the healthcare landscape continues to evolve, staying informed about these trends will be crucial for both healthcare providers and patients.
Recovery and Rehabilitation After Chest Surgery
Chest surgery recovery is not just about healing the wound; it’s about restoring overall health and functionality. At UC San Diego Health, we emphasize the importance of a comprehensive plan for restoring health after chest surgery, including state-of-the-art diagnosis and physical rehabilitation.
Immediate Post-Operative Care
The initial recovery phase after chest surgery is critical. Patients are closely monitored in the post-anesthesia care unit (PACU) for any immediate complications and are given pain management medication as needed. Our team ensures that patients are comfortable and stable before being transferred to a regular hospital room.
During this phase, monitoring for potential complications such as bleeding, infection, or respiratory issues is paramount. Our healthcare providers are trained to identify and manage these complications promptly.
Pain Management Strategies
Effective pain management is a cornerstone of post-operative care. We employ a multimodal approach to pain management, which may include epidural anesthesia, patient-controlled analgesia (PCA), and oral pain medications. This approach helps in minimizing pain while reducing the risk of opioid dependency.
Personalized pain management plans are developed for each patient, taking into account their medical history, the type of surgery performed, and their pain tolerance. Our goal is to ensure that patients are comfortable enough to participate in their recovery process, including early mobilization and pulmonary rehabilitation exercises.
Pulmonary Rehabilitation Programs
Pulmonary rehabilitation plays a vital role in helping patients regain their lung function and overall physical strength after chest surgery. These programs are tailored to the individual’s needs and typically include a combination of exercise training, education on lung health, and nutritional counseling.
Our pulmonary rehabilitation programs are designed to improve patients’ quality of life by enhancing their ability to perform daily activities and reducing symptoms such as shortness of breath. By focusing on comprehensive care, we help patients achieve the best possible outcomes after chest surgery.
Multidisciplinary Approach to Thoracic Surgical Care
At the heart of successful thoracic surgery is a multidisciplinary team that coordinates care with precision and compassion. We believe that a comprehensive approach is essential for delivering high-quality care to patients undergoing thoracic surgery.
The Thoracic Surgery Team
Our thoracic surgery team is composed of highly skilled professionals, including thoracic surgeons, anesthesiologists, nurses, and other support staff. Effective communication and collaboration among team members are critical to ensuring that patients receive seamless care.
- Thoracic surgeons with expertise in both traditional and minimally invasive techniques
- Anesthesiologists specializing in thoracic anesthesia
- Nurses and care coordinators who provide personalized support throughout the treatment journey
Coordination with Oncology and Pulmonology
Coordination with other specialties, particularly oncology and pulmonology, is vital in providing comprehensive care for thoracic surgery patients. We work closely with these teams to develop treatment plans that address the unique needs of each patient.
- Collaboration with oncologists to integrate surgical, chemotherapy, and radiation therapy plans
- Coordination with pulmonologists to optimize lung function and manage respiratory care
Patient-Centered Decision Making
At our institution, we prioritize patient-centered decision making, ensuring that patients are fully informed and involved in decisions about their care. We take the time to discuss treatment options, risks, and benefits with our patients, empowering them to make informed choices.
LivHospital exemplifies a multidisciplinary approach through continuous improvement in care coordination, patient experience, and innovation. By adopting a similar model, we can ensure that our patients receive the highest quality care.
Conclusion: Advancements Shaping the Future of Thoracic and Lung Surgery
As we conclude our exploration of thoracic and lung surgery, it’s clear that advancements in surgical techniques and technology are continually improving patient outcomes. The use of minimally invasive techniques and robotic-assisted surgery is on the rise, reflecting a commitment to innovation and improved patient care.
We have seen significant developments in thoracic surgery, including the adoption of robotic systems like the da Vinci Surgical System and the Revo-i robotic surgical system, which features haptic feedback technology. These advancements are shaping the future of lung surgery, enabling more precise and less invasive procedures.
The future of lung surgery looks promising, with ongoing innovations in minimally invasive techniques and robotic-assisted surgery. As these technologies continue to evolve, we can expect to see further improvements in patient care and outcomes. Our discussion has highlighted the importance of a multidisciplinary approach to thoracic surgical care, ensuring that patients receive comprehensive support throughout their treatment journey.
FAQ
What is the difference between thoracic surgery and lung surgery?
Thoracic surgery is a broader field that encompasses operations on various chest organs, including the lungs, esophagus, trachea, and other structures within the thorax. Lung surgery, on the other hand, is a subset of thoracic surgery that focuses specifically on the lungs.
What is a thoracotomy?
A thoracotomy, also known as open chest surgery, is a traditional surgical approach that involves making a significant incision to access the chest cavity. This allows surgeons to perform operations on the lungs, heart, and other chest structures.
What is lung resection?
Lung resection is a surgical procedure that involves removing a portion of the lung, often to treat lung cancer or other conditions. The type of resection performed depends on the extent and location of the disease, and can include lobectomy, pneumonectomy, segmentectomy, or wedge resections.
What is the purpose of removing a lung nodule?
Removing a lung nodule is often performed to diagnose and treat lung cancer. The diagnostic workup for lung nodules typically involves imaging studies and biopsies, and surgical removal is often necessary to determine the nature of the nodule.
What is minimally invasive thoracic surgery?
Minimally invasive thoracic surgery refers to surgical techniques that use smaller incisions and specialized instruments to perform operations on the chest organs. This can include video-assisted thoracoscopic surgery (VATS) and robotic-assisted thoracic surgery.
What is the recovery process like after chest surgery?
Recovery after chest surgery typically involves immediate post-operative care, pain management, and pulmonary rehabilitation programs to help patients regain their health and functionality. The specific recovery process can vary depending on the type of surgery and individual patient needs.
What is the role of a thoracic surgery team?
A thoracic surgery team is a multidisciplinary group of specialists who work together to provide comprehensive care to patients undergoing thoracic surgery. This team may include surgeons, oncologists, pulmonologists, and other healthcare professionals.
What is invasive surgery?
Invasive surgery refers to surgical procedures that involve making incisions or inserting instruments into the body to diagnose or treat a medical condition. Thoracic surgery, including lung surgery, is a type of invasive surgery.
What is thoracoscopic surgery?
Thoracoscopic surgery, also known as video-assisted thoracoscopic surgery (VATS), is a minimally invasive surgical technique that uses a camera and specialized instruments to perform operations on the chest organs through small incisions.
What is a lung operation?
A lung operation, also known as lung surgery, refers to surgical procedures that involve operating on the lungs, such as removing lung nodules, performing lobectomies, or conducting other types of lung resections.
What does thoracic mean?
Thoracic refers to the chest or thorax, which is the region of the body that contains the heart, lungs, and other vital organs. Thoracic surgery involves operating on the organs and structures within this region.
References
- National Cancer Institute. (2023). Lung cancer treatment (PDQ®)–Patient version. U.S. Department of Health and Human Services.https://www.cancer.gov/types/lung/patient/lung-treatment-pdq
- Centers for Disease Control and Prevention. (2022). Lung cancer and surgical treatments overview.https://www.cdc.gov/cancer/lung/basic_info/treatment.htm
,










