Last Updated on November 13, 2025 by
Which antibiotic is best? Explore effective thrombocytopenia treatment options and amazing new strategies for increasing platelet count.
Thrombocytopenia is when you have too few platelets, which can cause bleeding. Some medicines, like antibiotics, can make this worse. We’ll look into why antibiotics aren’t usually the first choice and what else you can try.

Some drugs, like hydroxyurea, can lower platelet counts, raising the risk of bleeding. It’s key to know what causes thrombocytopenia and how to treat it. At LivHospital, we choose targeted treatments over antibiotics. This shows our commitment to caring for each patient in a way that’s right for them.
Key Takeaways
- Antibiotics are not a standard treatment for thrombocytopenia and can sometimes cause or worsen the condition.
- Alternative treatments focus on addressing the underlying cause of low platelet count.
- Medications like hydroxyurea can temporarily affect platelet counts.
- Targeted therapies are often preferred over antibiotics for managing thrombocytopenia.
- Liv Hospital advocates for personalized, ethical care in treating thrombocytopenia.
Understanding Thrombocytopenia: Definition, Causes, and Symptoms
Thrombocytopenia, or low platelet count, is a condition that can come from many sources. These include autoimmune disorders, certain medications, and infections. Platelets are key for blood clotting. Without enough, you might bleed more easily and face other health issues.
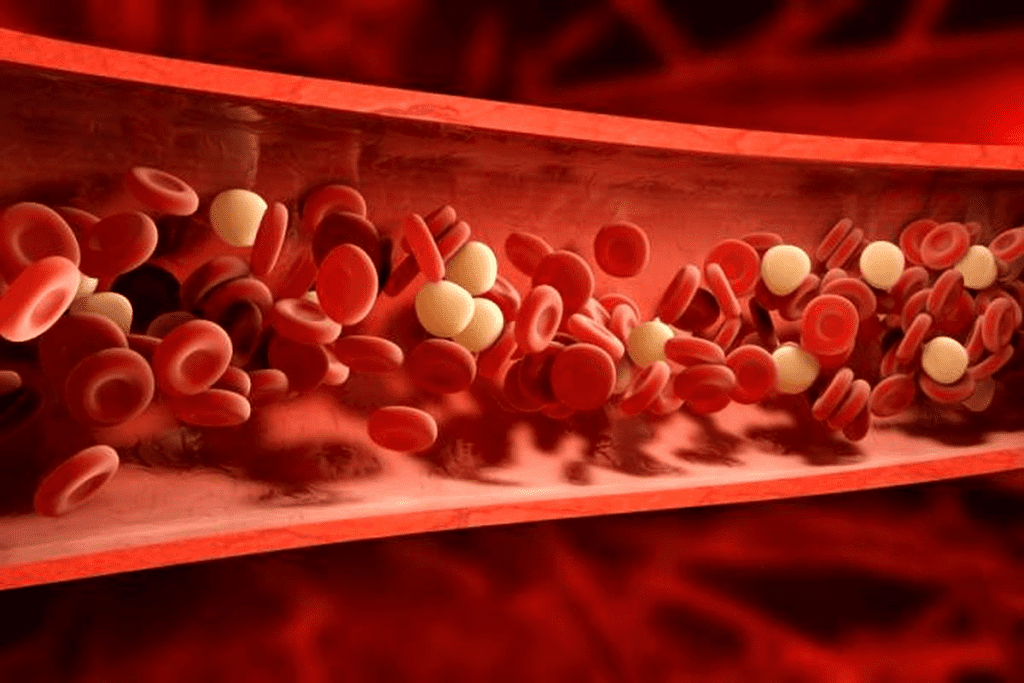
What Defines Low Platelet Count
A normal platelet count is between 150,000 and 450,000 per microliter of blood. If it drops below 150,000, you have thrombocytopenia. Counts under 50,000 are considered moderate, and under 20,000 are severe.
Primary vs. Secondary Thrombocytopenia
Thrombocytopenia can be either primary or secondary. Primary is often due to the immune system attacking platelets. Secondary is caused by other health issues, medications, or infections that harm platelet production or destruction.
For example, infections like sepsis or viruses can cause secondary thrombocytopenia by damaging the bone marrow. Some medications, like antibiotics, can also cause it by affecting the bone marrow or triggering an immune response against platelets.
Common Symptoms and Warning Signs
The symptoms of thrombocytopenia depend on how severe it is. Common signs include:
- Easy or excessive bruising
- Petechiae, which are small, pinpoint spots on the skin
- Nosebleeds or bleeding gums
- Prolonged bleeding from cuts
- Fatigue and weakness
In severe cases, thrombocytopenia can cause dangerous bleeding. Spotting these symptoms early is key for getting the right treatment.
Knowing the causes and symptoms of thrombocytopenia is vital for managing it well. Healthcare providers can then focus on the right treatment. This might involve managing an underlying disease, changing medications, or specific treatments for thrombocytopenia.
The Misconception: Antibiotics as Thrombocytopenia Treatment
Thrombocytopenia treatment focuses on the root cause, not antibiotics. This condition, or low platelet count, can stem from many sources. It’s key to know the cause for effective treatment.
Clarifying the Relationship Between Antibiotics and Platelets
Antibiotics fight bacterial infections. Yet, some can lead to drug-induced thrombocytopenia. This is when a drug causes a big drop in platelets. For example, vancomycin and linezolid have been linked to this issue.
The link between antibiotics and platelets is complex. Antibiotics can treat infections that might cause thrombocytopenia. But, some can also lower platelet counts. It’s vital to consider the risks and benefits when using antibiotics for patients with thrombocytopenia.
Why Antibiotics Are Not Recommended for Treating Low Platelets
Antibiotics aren’t a standard treatment for thrombocytopenia. They don’t directly fix the low platelet count’s cause. In some cases, they might even make it worse.
- Antibiotics don’t work against viral infections or immune disorders that cause thrombocytopenia.
- Some antibiotics can cause thrombocytopenia as a side effect.
- Other medications, like corticosteroids or immunoglobulins, are usually used to treat thrombocytopenia.
The Role of Antibiotics in Managing Underlying Infections
Antibiotics aren’t used to treat thrombocytopenia itself. But, they might be needed for underlying bacterial infections. It’s important to treat these infections to avoid further problems.
If an infection is thought to be causing thrombocytopenia, doctors might prescribe antibiotics. The choice of antibiotic must be thoughtful, considering the risks and benefits, even for those with a history of drug-induced thrombocytopenia.
Understanding the complex relationship between antibiotics and thrombocytopenia helps doctors make better treatment choices for their patients.
Drug-Induced Thrombocytopenia: When Medications Lower Platelet Counts
Certain medications can affect platelet counts in complex ways. They can either reduce platelet production or increase their destruction. It’s important to understand this to manage patients on such medications.
Mechanisms of Medication-Induced Platelet Destruction
Medications can lower platelet counts in different ways. Some drugs may harm the bone marrow, reducing platelet production. Others can trigger an immune response, causing platelet destruction. For example, some antibiotics can lead to an immune reaction that destroys platelets.
Key mechanisms include:
- Direct bone marrow suppression
- Immune-mediated platelet destruction
- Increased platelet clearance
Common Medications That Cause Thrombocytopenia
Many medications can lead to thrombocytopenia. These include antibiotics, anticonvulsants, and chemotherapy drugs. For instance, hydroxyurea, a chemotherapy drug, can temporarily lower platelet counts. It’s vital for doctors to keep an eye on platelet counts in patients on these drugs.
Recovery Timeline After Discontinuing Causative Drugs
The time it takes for platelet counts to recover after stopping the drug varies. Usually, counts start to go back up within a few days to a week. But in some cases, it might take longer. It’s important to keep monitoring platelet counts to ensure recovery and manage any complications.
Factors influencing recovery include:
- The specific medication involved
- The duration of exposure to the medication
- The patient’s overall health and bone marrow function
Antibiotics Known to Cause Thrombocytopenia
Some antibiotics can lead to thrombocytopenia, affecting how platelets are made or destroyed. This is a big worry for those taking these drugs. We’ll look at which antibiotics cause this problem and why.
Vancomycin: Mechanism and Risk Factors
Vancomycin, a type of antibiotic, can cause thrombocytopenia in some. It happens when the body attacks platelets. Vancomycin-dependent antibodies are often to blame. It’s key to watch platelet counts in those taking it. Long-term use and high doses increase the risk.
Linezolid and Its Effects on Bone Marrow
Linezolid, another antibiotic, can lower platelet counts by affecting bone marrow. This makes it hard for the body to make enough platelets. Regular blood count checks are vital, more so for those with bone marrow issues or on it for a long time.
“The risk of thrombocytopenia associated with linezolid is higher in patients with renal insufficiency or those receiving concomitant medications that affect bone marrow.”
Beta-Lactams and Immune-Mediated Platelet Destruction
Beta-lactam antibiotics, like penicillins and cephalosporins, can also cause thrombocytopenia. This happens when the drug marks platelets for destruction. Stopping the drug is usually the first step to treat this.
Other Antimicrobials with Documented Thrombocytopenic Effects
Antibiotics like sulfonamides and rifampicin can also cause thrombocytopenia. The reasons vary, from immune attacks to bone marrow issues. Knowing these side effects helps catch and manage them early.
Diagnosing the Underlying Cause of Low Platelet Count
It’s key to find out why someone has thrombocytopenia to choose the right thrombocytopenia treatment. Doctors use lab tests and check-ups to figure out the cause.
Essential Laboratory Tests and Evaluations
Lab tests play a big role in finding out why someone has low platelets. These tests include:
- Complete Blood Count (CBC): This test checks the platelet count and other blood cells.
- Blood Smear: It looks at the shape of platelets and other blood cells.
- Bone Marrow Tests: These tests check how platelets are made in the bone marrow. This is important for thrombocytopenia drugs that might affect bone marrow.
These tests help find out if the low platelet count is because of not making enough, destroying them, or they’re stuck somewhere.
Bone Marrow Examination: When It’s Necessary
A bone marrow test is very important in some cases of low platelets. It’s needed when:
- The cause of low platelets is not clear after first tests.
- There’s a thought that the bone marrow might not be working right or has something stuck in it.
This test checks if the bone marrow can make platelets. It helps pick the right low platelet medicine.
Identifying Drug-Induced vs. Immune Thrombocytopenia
Telling drug-induced from immune thrombocytopenia is very important for the right treatment.
- Drug-Induced Thrombocytopenia: This happens when certain medicines, like some antibiotics, cause low platelets. Finding and stopping the bad drug helps.
- Immune Thrombocytopenia: This is when the body’s immune system attacks platelets. Doctors look for antibodies against platelets to diagnose it.
Knowing the cause helps doctors give the best thrombocytopenia treatment. This might mean changing medicines, using drugs to calm the immune system, or other treatments.
Evidence-Based Thrombocytopenia Treatment Options
Patients with thrombocytopenia have many treatment options. These choices depend on the cause of low platelets, how severe it is, and the patient’s health.
Corticosteroids: Mechanism and Efficacy Rates
Corticosteroids are often the first choice for immune thrombocytopenia (ITP). They help by reducing the immune system’s attack on platelets. Prednisone is a common corticosteroid, used at high doses first and then lowered as platelets increase. Many studies show they can raise platelet counts in many patients.
Intravenous Immunoglobulin (IVIG): When It’s Indicated
IVIG is used when a quick increase in platelets is needed, like in severe bleeding or before surgery. It blocks the spleen from removing antibody-tagged platelets. This is great for patients needing a fast response or who didn’t get better with corticosteroids.
Anti-D Immunoglobulin for Rh-Positive Patients
For Rh-positive patients with ITP, anti-D immunoglobulin is a good option. It binds to the RhD antigen on red blood cells, helping to protect platelets from the immune system. It’s used for patients who didn’t get better with corticosteroids or IVIG.
These treatments offer hope for patients with thrombocytopenia. They provide effective ways to manage this condition.
Second-Line Treatments for Refractory Thrombocytopenia
For patients with refractory thrombocytopenia, second-line treatments offer alternative solutions when initial therapies fail. These treatments are key for managing the condition in patients who don’t respond to first-line therapies.
Thrombopoietin Receptor Agonists: A Promising Approach
Thrombopoietin receptor agonists have shown significant promise in treating refractory thrombocytopenia. They have response rates over 65% at one month in clinical trials. These medications stimulate the production of platelets in the bone marrow.
Using thrombopoietin receptor agonists is a targeted way to increase platelet counts. They activate the thrombopoietin receptor. This enhances megakaryopoiesis, the process by which megakaryocytes mature and release platelets.
| Treatment | Response Rate | Mechanism of Action |
| Thrombopoietin Receptor Agonists | 65%+ at 1 month | Stimulates platelet production in bone marrow |
| Rituximab | Two-thirds initial response; 20-39% durable remissions | Targets B-cells, reducing antibody production |
Rituximab: Targeting B-Cells for Remission
Rituximab is another second-line treatment option. It offers an initial response in about two-thirds of patients. But, durable remissions are seen in only 20-39% of cases. This medication depletes B-cells, which are involved in the autoimmune destruction of platelets.
The effectiveness of rituximab in treating refractory thrombocytopenia shows the immune system’s role in the condition. By reducing autoantibody production, rituximab can help decrease platelet destruction.
Other Immunosuppressive Approaches
Other immunosuppressive therapies may also be considered for refractory thrombocytopenia. These treatments aim to reduce the immune system’s attack on platelets, increasing platelet counts.
While these treatments can be effective, they also carry risks and side effects. Careful patient selection and monitoring are essential to maximize benefits and minimize adverse effects.
Surgical Management: Splenectomy for Thrombocytopenia
In cases of thrombocytopenia where medical treatments fail, splenectomy offers a cure. This surgery removes the spleen. It’s a treatment for patients with immune thrombocytopenia (ITP) who don’t respond to initial treatments.
86% Initial and 53% Durable Response Rates
Studies show splenectomy works well, with about 86% of patients seeing a big jump in platelet count right after surgery. Around 53% of these patients keep seeing improvements over time. This means their condition gets better and stays that way.
The spleen plays a big role in destroying platelets and making antibodies against them. Taking out the spleen stops platelet destruction and lowers antibody production. This helps patients a lot.
Patient Selection and Contraindications
Not every patient with thrombocytopenia is right for splenectomy. Choosing the right patients is key. We look at how severe their symptoms are, how long they’ve had the illness, and how they’ve done with other treatments. We also check for any health issues that might make surgery risky.
It’s important to pick patients who will likely get better from the surgery and who face fewer risks. We check their overall health, look for infections, and think about possible complications.
Long-Term Considerations After Spleen Removal
After the surgery, patients need ongoing care to watch for problems like infections and blood clots. We also have to think about the long-term effects of having too many platelets and if they might need blood thinners.
Patients also need to know about the risks of not having a spleen. This includes getting sick easier and needing special shots and antibiotics to stay safe.
By knowing the good and bad of splenectomy, we can give better care to patients with thrombocytopenia. This helps them live better lives.
Emergency Management of Severe Thrombocytopenia
When platelet counts drop too low, doctors must act fast to stop serious bleeding. Severe thrombocytopenia is a serious condition that needs quick action. We will look at emergency strategies, like platelet transfusions and how to stop bleeding.
Platelet Transfusions: Indications and Limitations
Platelet transfusions are key in treating severe thrombocytopenia. They quickly raise platelet counts, lowering bleeding risks. Doctors decide to transfuse platelets based on the patient’s count, health, and if they’re bleeding.
Transfusions are usually for counts under 10,000/μL or if someone is bleeding. The aim is to get the platelet count up to a safe level to stop or prevent bleeding.
Controlling Active Bleeding in Thrombocytopenic Patients
Stopping active bleeding is vital in severe thrombocytopenia. Methods include applying pressure, using hemostatic agents, and sometimes surgery. The right method depends on the bleeding site and how bad it is. Also, fixing the thrombocytopenia cause is key to avoid more bleeding.
Managing bleeding in thrombocytopenic patients needs a team effort. Hematologists, surgeons, and others work together. Hemostatic agents and platelet transfusions can save lives in these cases.
American Society of Hematology Guidelines for Thrombocytopenia Treatment
The American Society of Hematology has made big changes in how we treat thrombocytopenia. Their guidelines help doctors give patients the best care based on science.
First-Line Treatment Recommendations
The American Society of Hematology says corticosteroids should be the first choice for treating Immune Thrombocytopenia (ITP). Corticosteroids help by reducing how much the immune system attacks platelets. This helps many patients see their platelet counts go up.
Here are some important things to know about corticosteroid treatment:
- Doctors usually start with prednisone at 0.5 to 2 mg/kg/day.
- They check how well the treatment is working after 2-4 weeks.
- Slowly reducing the dose of corticosteroids helps avoid side effects.
Treatment Algorithm Based on Patient Factors
Choosing the right treatment for thrombocytopenia depends on many things. These include the cause of the low platelets, how bad the symptoms are, and the patient’s overall health. For example, those with severe bleeding might need stronger treatments like intravenous immunoglobulin (IVIG) or platelet transfusions.
Here are some factors to consider in a treatment plan:
- How low the platelet count is: Those with very low counts might need more intense treatment.
- Is there bleeding? Active bleeding or a high risk of it means quicker action is needed.
- What’s causing the low platelets? The treatment can change based on the cause, like ITP or drug side effects.
Recent Updates in Clinical Practice Guidelines
The American Society of Hematology keeps updating its guidelines. They do this to keep up with new research and findings. The latest changes focus on tailoring treatments to fit each patient’s needs and risks.
Some recent changes include:
- More emphasis on thrombopoietin receptor agonists for hard-to-treat ITP.
- Guidance on using rituximab for those who don’t respond to first treatments.
- Advice on watching for and managing side effects of long-term treatments.
Special Considerations for Antibiotic Use in Thrombocytopenic Patients
Patients with thrombocytopenia need careful antibiotic treatment. Some antibiotics can make their condition worse. It’s important to weigh the benefits and risks of each antibiotic.
Monitoring Requirements During Antimicrobial Therapy
Antibiotics must be watched closely in thrombocytopenic patients. Regular blood tests are key to catch any problems early. This helps keep platelet counts in check.
Key Monitoring Parameters:
- Platelet count
- White blood cell count
- Hemoglobin levels
- Signs of bleeding or bruising
Safer Antibiotic Choices for At-Risk Individuals
Not all antibiotics are the same for thrombocytopenic patients. Some are safer than others. For example, penicillins and cephalosporins are often okay. But, some antibiotics might increase the risk of low platelets.
| Antibiotic Class | Risk Level | Examples |
| Penicillins | Low | Amoxicillin, Ampicillin |
| Cephalosporins | Low | Ceftriaxone, Cefepime |
| Vancomycin | Moderate to High | Vancomycin |
| Linezolid | High | Linezolid |
When to Discontinue Suspected Causative Antibiotics
If a patient gets thrombocytopenia on antibiotics, check if the antibiotic caused it. If it did, stop the antibiotic. Then, switch to a safer one if needed.
Living with Chronic Thrombocytopenia: Practical Management
Chronic thrombocytopenia brings its own set of challenges. It needs a special management plan to lower risks and improve life quality. We will look at effective ways to manage this condition.
Bleeding Precautions in Daily Activities
People with chronic thrombocytopenia must be careful in their daily lives to avoid bleeding. Simple steps can greatly reduce injury risk.
- Use gentle touch when handling objects to avoid bruising.
- Avoid contact sports and activities that may lead to falls or collisions.
- Wear protective gear such as helmets and knee pads when engaging in potentially risky activities.
Being cautious and prepared helps avoid bleeding. It also keeps individuals independent.
Dietary Considerations and Supplements
Eating a balanced diet full of essential nutrients is key for health, including platelet production. Some foods and supplements can support platelet health.
| Nutrient | Food Sources | Potential Benefits |
| Iron | Red meat, spinach, fortified cereals | Supports healthy red blood cell production |
| Vitamin B12 | Meat, fish, poultry, dairy products | Essential for the production of platelets |
| Folate | Leafy greens, legumes, fortified cereals | Critical for preventing low platelet count |
Always talk to a healthcare provider before taking supplements. They can interact with medicines or cause problems in some people.
Physical Activity Guidelines and Restrictions
While some activities should be avoided, gentle exercises are good. They help keep physical health and lower risks of complications.
- Engage in low-impact activities such as walking, swimming, or yoga.
- Avoid heavy lifting and bending.
- Monitor your body’s response to exercise and adjust as needed.
Choosing the right physical activities wisely helps enjoy exercise benefits. It also reduces risks for those with chronic thrombocytopenia.
When to Seek Immediate Medical Care for Thrombocytopenia
Thrombocytopenia is a condition where you have low platelets. Sometimes, you need to see a doctor right away. We’ll talk about when you should get help fast and why checking in regularly is important.
Warning Signs of Dangerous Bleeding
If you have thrombocytopenia, watch out for signs of serious bleeding. These include:
- Severe bruising or purpura
- Nosebleeds that won’t stop
- Bleeding gums or mouth sores
- Blood in urine or stool
- Headaches or confusion, which could indicate intracranial bleeding
If you see any of these, get medical help fast. Prompt thrombocytopenia treatment can really help if you’re bleeding a lot.
Follow-up Monitoring and Long-Term Management
Seeing your doctor regularly is key to managing thrombocytopenia. They’ll check your platelet count and adjust your thrombocytopenia drugs if needed. It’s also important to learn about low platelet medicine and its side effects.
For long-term care, you might need to make some lifestyle changes. This could mean avoiding sports, being gentle with your teeth, and being careful with sharp objects.
By knowing the warning signs and keeping up with doctor visits, people with thrombocytopenia can live full lives. They can also reduce the risks of bleeding.
Conclusion
Thrombocytopenia is a complex condition that needs a detailed approach to manage. We’ve looked at different treatments, like corticosteroids and IVIG, and surgeries like splenectomy. We also talked about lifestyle changes to help manage symptoms and prevent problems.
Good treatment for thrombocytopenia often mixes these methods, based on the patient’s needs. At LivHospital, we aim to give top-notch care to those with thrombocytopenia. Our team works with patients to create custom treatment plans, using the newest itp medications and therapies.
Knowing about thrombocytopenia’s causes, symptoms, and treatments helps patients manage their condition better. We think giving world-class healthcare with full support is key to the best patient results.
FAQ
What is thrombocytopenia, and how is it defined?
Thrombocytopenia is when you have too few platelets in your blood. This can cause bleeding problems. It’s when your platelet count is below 150,000 per microliter of blood.
What are the primary causes of thrombocytopenia?
There are two main types of thrombocytopenia. Primary is when your body attacks and destroys platelets. Secondary is caused by things like medicines, infections, and other health issues.
Are antibiotics a standard treatment for thrombocytopenia?
No, antibiotics aren’t a usual treatment for thrombocytopenia. Some antibiotics can even make it worse. They’re used to fight infections that might be causing the low platelet count, but they’re not the main treatment.
Which medications can cause thrombocytopenia?
Some medicines, like vancomycin and linezolid, can lower platelet counts. Other drugs that might cause this problem include heparin, certain anticonvulsants, and some chemotherapy drugs.
How is drug-induced thrombocytopenia diagnosed?
Doctors use tests and look at your medical history to find out if a drug is causing it. They might stop the drug and check your platelet count again to see if it helps.
What are the treatment options for immune thrombocytopenia (ITP)?
For ITP, doctors might use corticosteroids, IVIG, or anti-D immunoglobulin. If these don’t work, they might try thrombopoietin receptor agonists, rituximab, or other treatments to boost platelet production.
When is splenectomy considered for thrombocytopenia treatment?
Doctors might suggest a splenectomy if other treatments don’t work well. It depends on how severe the thrombocytopenia is and if there are any risks.
How can patients with thrombocytopenia manage their condition in daily life?
People with thrombocytopenia should be careful to avoid injuries and follow a healthy diet. They should also keep up with regular check-ups and manage their condition long-term.
What are the warning signs of dangerous bleeding in thrombocytopenia patients?
Signs of serious bleeding include big bruises, nosebleeds, and bleeding in the gut or brain. If you see these, get medical help right away.
How are platelet transfusions used in the emergency management of severe thrombocytopenia?
Platelet transfusions quickly raise platelet counts in severe cases. The decision to give them depends on how bad the bleeding is and the platelet count.
What are the American Society of Hematology guidelines for thrombocytopenia treatment?
The American Society of Hematology has guidelines for treating thrombocytopenia. They include first-line treatments, treatment plans based on patient factors, and updates to their guidelines.
References
- Zheng, X. L., et al. (2025). 2025 focused update of the 2020 ISTH guidelines for thrombotic thrombocytopenic purpura. Journal of Thrombosis and Haemostasis. https://pubmed.ncbi.nlm.nih.gov/40533296/
- Wadhwa, A., & Gernsheimer, T. (2023). Immune thrombocytopenia: An update on pathophysiology and treatment. American Journal of Hematology, 98(5), 560-571. https://onlinelibrary.wiley.com/doi/10.1002/ajh.27448





