Last Updated on November 13, 2025 by
The link between thrombocytosis and bleeding risk has sparked a lot of medical interest. Recent studies have questioned the idea that thrombocytosis and high platelet count could actually increase the risk of bleeding.
Essential thrombocythemia, a condition with high platelet counts, is at the heart of this debate. Research shows that while very high thrombocytosis might seem to raise bleeding risk, the actual risk is similar to those without it.
This article dives into the complexities of thrombocythemia and its effect on bleeding risk. It aims to shed light on the latest research and its implications for patient care.
It’s important to understand thrombocytosis to diagnose and treat high platelet counts. Thrombocytosis is when the platelet count in your blood is too high.
Thrombocytosis is divided into two types: primary and secondary. Primary thrombocytosis, or essential thrombocythemia (ET), is a bone marrow disorder that makes too many platelets. Secondary thrombocytosis happens due to infections, inflammation, or cancer.
Knowing if it’s primary or secondary thrombocytosis helps doctors choose the right treatment. Primary thrombocytosis is a serious condition, but secondary is often fixed once the cause is treated.
A normal platelet count is between 150,000 and 450,000 per microliter of blood. Elevated platelet counts are found through a complete blood count (CBC) test.
People with thrombocytosis have counts over 1,000,000. Such high counts can lead to blood clots and bleeding.

Primary thrombocytosis, or essential thrombocythemia (ET), is a rare disorder that makes too many platelets. It’s linked to genetic changes like JAK2, MPL, or CALR.
Secondary thrombocytosis is more common and can be caused by:
Finding out why someone has thrombocytosis is key to treating it right and avoiding problems.
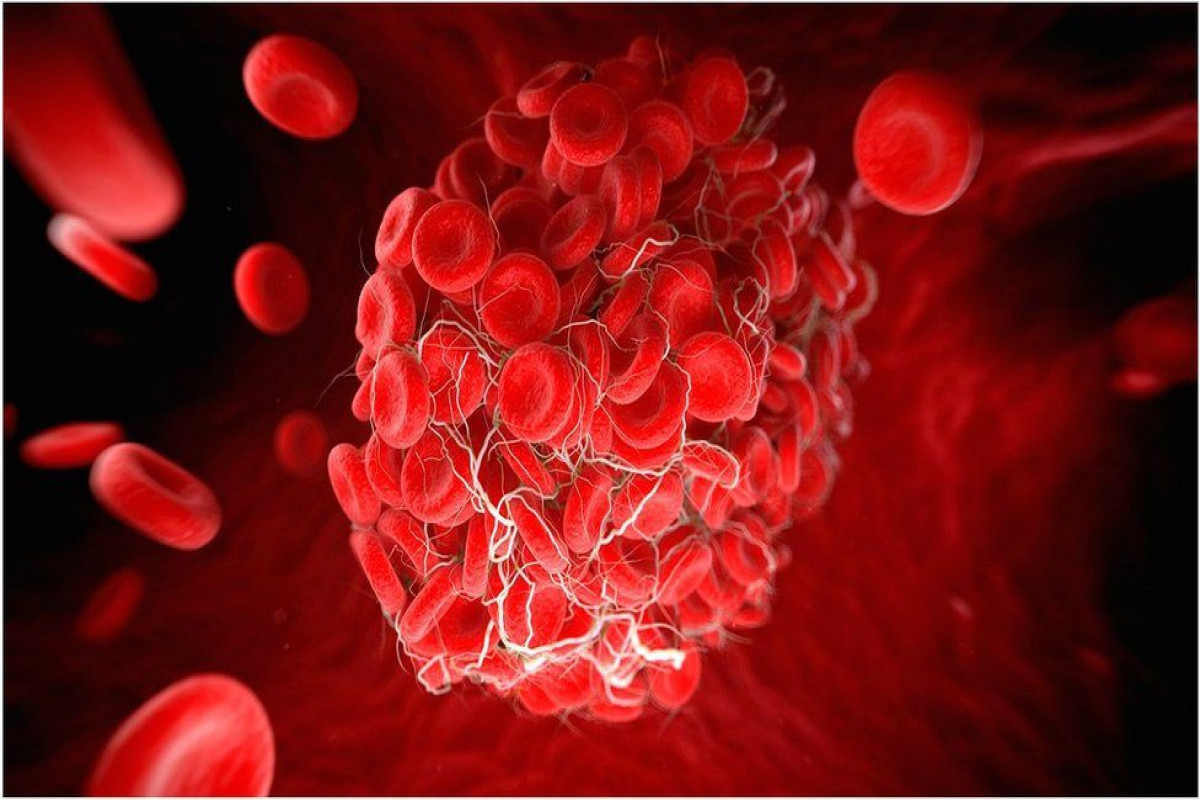
Patients with thrombocytosis face a unique challenge. They are at risk for both blood clots and bleeding. This happens because platelets play a key role in stopping bleeding.

Platelets are vital for stopping bleeding. They stick to injuries, clump together, and form a plug. This plug is then strengthened by fibrin, preventing too much blood loss.
The key functions of platelets include:
High platelet counts in thrombocytosis can cause both clotting and bleeding. This is due to several reasons.
Some of the factors contributing to this paradox include:
A study on essential thrombocythemia found that extreme thrombocytosis increases bleeding risk. This shows the complex link between platelet count and bleeding risk.
“The management of thrombocytosis requires a nuanced understanding of the balance between clotting and bleeding risks.”
” Expert in Hematology
It’s important to understand how platelets work and the factors behind the paradox in thrombocytosis. This knowledge helps in managing patients better.
When platelet counts go over 1,000 x 10^9/L, patients face a high risk of bleeding. This is often linked to myeloproliferative neoplasms, like essential thrombocythemia (ET). ET is a blood disorder that can turn into cancer.
Extreme thrombocytosis means having more than 1,000 x 10^9/L platelets. It’s rare and usually found in those with myeloproliferative neoplasms. Knowing the difference between thrombocytosis and thrombocythemia is key. Thrombocythemia is linked to these neoplasms.
This condition can cause both blood clots and bleeding. It’s important to find out why it’s happening to treat it right.
Acquired von Willebrand syndrome (AVWS) happens with high platelet counts. The platelets take up von Willebrand factor (VWF), leaving less in the blood. This makes it harder for platelets to stick together, raising the risk of bleeding.
Key factors contributing to AVWS include:
Lab tests are key in figuring out bleeding risk in patients with high platelet counts. These include:
Understanding extreme thrombocytosis and AVWS helps doctors manage bleeding risks. Lab tests are vital in making treatment plans and reducing risks.
A study with 451 patients with essential thrombocythemia sheds light on bleeding risks. This condition, with high platelet counts, can lead to both blood clots and bleeding.
The study looked at patients with essential thrombocythemia, a rare blood disorder. It found managing high platelet counts is complex. Patients face risks of blood clots and bleeding.
The study lasted a long time, giving a detailed look at patient outcomes. It tracked major and minor bleeding, and other complications of essential thrombocythemia.
The study found a big difference in major bleeding between groups. 21% of patients in one group had major bleeding, while 13% in another did. This shows how different patients with thrombocytosis face different risks.
The researchers looked at many factors. They considered platelet counts, other health issues, and treatments.
The study also looked at minor bleeding. It found 16% of patients in one group had minor bleeding, compared to 15% in the other. This shows the overall risk of bleeding in essential thrombocythemia patients.
The researchers did statistical tests to understand their findings. They found important insights into what affects bleeding risk in thrombocytosis.
The study’s results help in managing patients with high platelet counts. It shows the need for a detailed approach to reduce risks. It supports personalized treatment plans based on each patient’s situation.
The study adds to the growing evidence on thrombocytosis and bleeding risk. As research goes on, doctors will get better at managing essential thrombocythemia. This will help lower the chance of bad outcomes.
It’s important to know what increases bleeding risk in thrombocytosis. This condition has too many platelets, which can paradoxically lead to more bleeding. Several factors can complicate this situation.
Antiplatelet therapy is a big risk for bleeding in thrombocytosis patients. Antiplatelet medications aim to stop blood clots but can cause more bleeding. It’s key to watch these patients closely.
Diabetes and other health issues can raise bleeding risk in thrombocytosis. Diabetes mellitus can mess with platelet function and increase vascular risks. Other health problems can make things worse.
Some genetic changes can make bleeding risk higher in thrombocytosis patients. Mutations in JAK2, CALR, and MPL genes can affect bleeding and clotting risks. Knowing these genetic factors helps tailor care for each patient.
Age and gender also play a part in bleeding risk in thrombocytosis. Older people might face higher risks due to more health issues and less body strength. Women might also have a higher risk of bleeding in some cases.
In summary, bleeding risk in thrombocytosis comes from many angles. It’s vital to understand these factors well. This knowledge helps in creating better care plans to reduce bleeding risks for these patients.
Essential thrombocythemia is a unique myeloproliferative neoplasm. It is caused by the growth of megakaryocytes, leading to a higher risk of blood clots and bleeding. Managing this condition is challenging because it involves balancing the risk of blood clots against the risk of bleeding.
ET is known for having too many platelets, usually over 450 x 10^9/L. Doctors diagnose it by looking at symptoms, lab results, and ruling out other diseases. Genetic mutations, like JAK2, CALR, or MPL, are key in ET. They affect how the disease shows up and how it progresses.
ET symptoms can vary a lot. Some people might not show any signs for a long time. Others might have blood clots or bleeding right away. The risk of these problems depends on age, past clotting issues, and other health risks.
People with ET face risks of both bleeding and blood clots. The reasons for these risks are complex, involving platelet counts, platelet function, and blood vessel health. Blood clots are more common in ET, with deep vein thrombosis and pulmonary embolism being big concerns. But, bleeding can also happen, like in the gut or through bleeding, more in those with very high platelet counts or on certain treatments.
The outlook for ET patients varies. Some have a mild course, while others face serious problems from clots or bleeding. Regular check-ups and a personalized treatment plan are key to reducing these risks. Genetic changes, like JAK2 V617F, can affect how the disease progresses or turns into a more serious condition.
Managing ET needs a full approach, balancing clot risk with bleeding risk. Understanding ET and its factors helps doctors create better treatment plans. This can lead to better outcomes for patients.
Managing thrombocytosis requires a detailed plan to lower bleeding risks. This includes using treatments that reduce platelet counts, carefully choosing antiplatelet drugs, and closely watching high-risk patients.
Cytoreductive therapies aim to lower platelet counts to safe levels. This reduces the chance of bleeding. Hydroxyurea is often the first choice because it works well. Anagrelide is an alternative for those who can’t take hydroxyurea.
The right treatment depends on the patient’s age, health, and other bleeding or clotting risks.
Aspirin is used to prevent blood clots in thrombocytosis patients. But, it can increase bleeding risk. For very high platelet counts, the bleeding risk might be too high.
High-risk patients need regular checks. This includes complete blood counts (CBCs) to track platelet levels. It’s also important to watch for signs of bleeding, like gastrointestinal bleeding or easy bruising.
Before surgery or procedures, special steps are taken to avoid bleeding. This might mean changing treatments or medications. It’s key for doctors and surgeons to work together closely.
With these strategies, doctors can greatly lower bleeding risks in thrombocytosis patients. This improves their health outcomes.
It’s important to understand thrombocytosis and its effects on patients. Knowing the difference between thrombocythemia and essential thrombocythemia helps predict risks. This knowledge is key to managing patients with high platelet counts.
Studies have found that very high platelet counts can cause bleeding problems. Doctors need to watch for signs of bleeding, like antiplatelet therapy and certain genetic changes. These factors can raise the risk of bleeding in patients with thrombocytosis.
To lower bleeding risks, doctors use treatments like reducing platelet counts and monitoring closely. By grasping the differences between thrombocytosis and thrombocythemia, healthcare teams can create better treatment plans. This approach helps improve patient outcomes.
The study of thrombocytosis shows the importance of a detailed care plan. This plan must consider the cause of high platelet counts and the associated risks. This way, doctors can provide better care for their patients.
Subscribe to our e-newsletter to stay informed about the latest innovations in the world of health and exclusive offers!