Last Updated on December 2, 2025 by Bilal Hasdemir

Some surgeries are more dangerous than others. A single mistake can change a patient’s life forever. These operations have a higher mortality rate because of their complexity and the patient’s health.Learn about the top riskiest surgeries and what makes them complex, including risk factors and advanced recovery care.
These high-risk surgical procedures concern both doctors and patients.Knowing the risks helps everyone make better choices.
Key Takeaways
- Surgical procedures vary in complexity and risk.
- Certain operations have a higher mortality rate.
- Understanding risks is key for informed decisions.
- Patient health greatly affects surgical outcomes.
- Doctors must carefully evaluate risks.
Understanding Surgical Risk Assessment

When we talk about surgical risk, we’re looking at how likely complications can happen during and after surgery. This is a big deal because it helps doctors get ready for what might happen. It’s all about understanding the risks to make sure patients get the best care.
How Medical Professionals Measure Surgical Risk
Doctors use special scoring systems to figure out the risk of surgery. These scores look at how sick the patient is and how hard the surgery will be. This helps doctors decide who needs more tests before surgery. Getting the risk right is important to avoid problems and make sure surgery goes well.
Common Risk Factors That Increase Surgical Danger
There are many things that can make surgery riskier. Things like how old the patient is, their health, and any health problems they have. The type and length of the surgery also matter. Spotting these risks early helps doctors take steps to prevent problems.
The Top 3 Riskiest Surgeries and Why They’re Dangerous
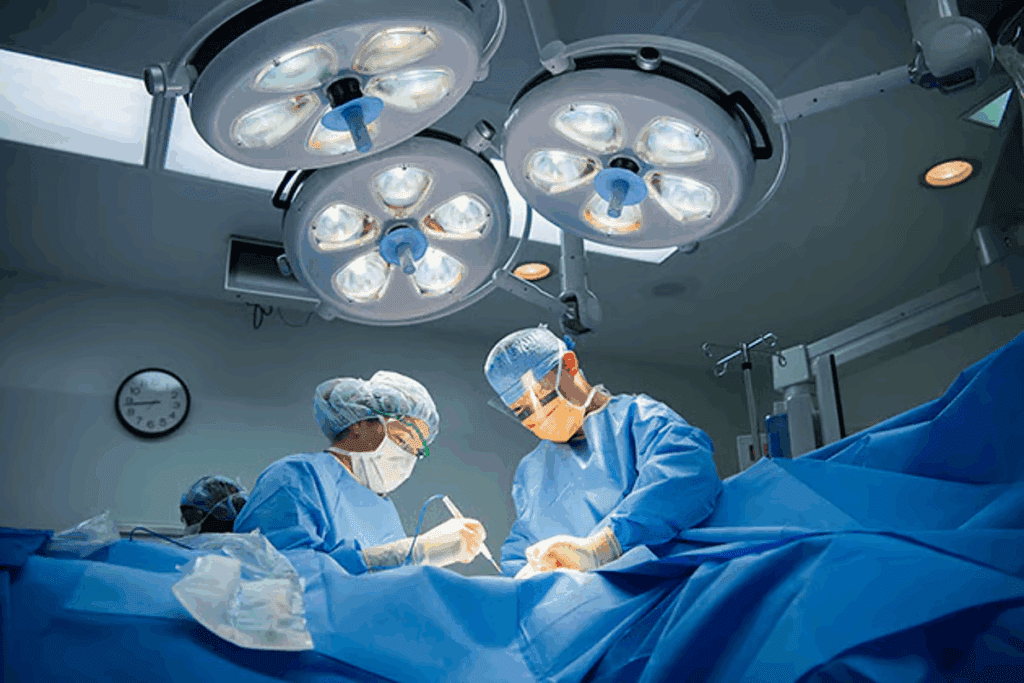
The top 3 riskiest surgeries are procedures that doctors handle with great care. They are high-risk because of their complexity and the importance of the organs involved. These surgeries need skilled surgeons and advanced medical facilities.
Mortality Rates Comparison
Looking at the mortality rates of these surgeries shows their danger level. For example, aneurysm repair and pancreatic surgery have higher death rates than other surgeries. The death rates vary, depending on the patient’s health and the surgeon’s skill.
Life-Saving Benefits Despite the Dangers
Even with the risks, these surgeries can be life-saving. For instance, removing esophageal cancer can greatly increase a patient’s survival chances. The benefits of these surgeries often outweigh the risks, making them a vital option for treating serious conditions.
Aortic Dissection Repair: The Most Dangerous Cardiovascular Surgery
Aortic dissection repair is a very risky surgery in cardiovascular medicine. It needs careful planning and skilled hands. This surgery fixes a tear in the aorta, the main artery, which can be deadly if not done right.
Why This Procedure Is So Complex
The aorta is delicate and vital for blood flow. Surgeons face a big challenge in fixing it. They must work fast and precisely to avoid more harm.
Mortality Statistics and Survival Rates
The death rate for this surgery depends on many things. These include the patient’s health, how bad the tear is, and how quickly and well the surgery is done. Usually, 10% to 30% of patients die soon after surgery. But, those who get quick and good care have a better chance of living.
| Category | Mortality Rate (%) | Survival Rate (%) |
| Overall | 15-25 | 75-85 |
| Type A Dissection | 20-30 | 70-80 |
| Type B Dissection | 10-20 | 80-90 |
Common Complications and Their Management
This surgery can lead to serious problems like brain damage, organ failure, and bleeding. It’s key to manage these issues well to help patients recover.
Neurological Complications
Brain problems can happen because the aorta is close to the spinal cord. Doctors use special techniques and watch brain function closely during and after surgery.
Organ Failure Risks
Organ failure is a big risk because of poor blood flow during surgery. Keeping a close eye on organ function is vital to reduce this risk.
Pancreaticoduodenectomy (Whipple Procedure): High-Risk Abdominal Surgery
The Whipple procedure is a complex and risky surgery. It’s mainly done to remove tumors or treat problems with the pancreas, bile duct, and duodenum.
The Technical Challenges of Pancreatic Surgery
Pancreatic surgery is very challenging. The pancreas is delicate and close to important structures. Surgeons must carefully navigate this complex area to avoid damage.
Post-Operative Complications and Their Frequency
Even with better surgery techniques, complications after a Whipple procedure are common. These issues can affect how well a patient recovers and their overall outcome.
Pancreatic Fistula
A pancreatic fistula is a serious problem. It happens when the pancreas connects to other organs or the skin, causing pancreatic enzyme leakage. Managing this condition is critical to prevent more issues.
Delayed Gastric Emptying
Delayed gastric emptying is another common issue. It means the stomach takes too long to empty its contents. This can cause nutritional problems and longer hospital stays.
Long-Term Survival Outcomes
The survival chances for patients after a Whipple procedure depend on the reason for the surgery. For cancer patients, better surgery and treatments have improved survival rates.
| Complication | Frequency | Management |
| Pancreatic Fistula | 20-30% | Drainage, nutritional support |
| Delayed Gastric Emptying | 15-25% | Nutritional support, medication |
Craniotomy for Complex Brain Tumors: Neurosurgical Risks
Neurosurgeons have big challenges when they do craniotomies for complex brain tumors. This is because the brain is very delicate. They remove part of the skull to get to the tumor. But, there’s a big risk of hurting other brain areas.
Navigating the Delicate Brain Tissue
The brain is a complex and sensitive organ. Surgeries on it are risky. Neurosurgeons have to carefully move through delicate tissue to get to the tumor.
They use advanced imaging and navigation systems. These tools help them find the tumor’s exact spot. They also plan the safest way to get to it.
Potential Neurological Deficits
One big risk of craniotomy for complex brain tumors is neurological deficits. These can be anything from problems with thinking to issues with moving. It all depends on where the tumor is and which brain areas are affected during surgery.
Cognitive Impairments
Cognitive impairments can affect memory, attention, and how well you can make decisions. How much these impairments affect someone can vary a lot. It depends on which brain areas are impacted.
Motor Function Deficits
Motor function deficits can cause weakness, paralysis, or problems with coordination. These issues can really affect a person’s quality of life. Often, patients need to go through rehabilitation to get their strength and functions back.
Recovery Trajectory and Rehabilitation
The recovery after a craniotomy for a complex brain tumor is long and hard. Patients usually need a big rehabilitation program. This program helps them deal with any neurological deficits and get their strength and functions back.
The recovery path can be different for everyone. It depends on things like how complex the tumor is, the patient’s health, and if there are any complications after surgery.
Key factors influencing recovery include:
- The extent of surgical intervention
- Presence of post-operative complications
- Effectiveness of rehabilitation programs
What Makes These Top Riskiest Surgeries So Dangerous
The top riskiest surgeries are very complex and pose big challenges to surgeons. They deal with detailed body parts and need exact techniques to avoid big problems.
Anatomical Complexity and Surgical Challenges
Anatomical complexity is a big reason these surgeries are risky. For example, surgeries on vital organs like the brain, heart, or liver are very tough. Surgeons have to carefully move through complex anatomy, avoiding key areas to prevent serious harm.
| Surgical Procedure | Anatomical Complexity | Surgical Challenges |
| Aortic Dissection Repair | High | Navigating the aortic wall |
| Pancreaticoduodenectomy (Whipple Procedure) | Very High | Reconstructing digestive tract |
| Craniotomy for Complex Brain Tumors | Extremely High | Preserving brain function |
Physiological Stress on Multiple Body Systems
These surgeries also put a lot of stress on the body, affecting many systems. The body’s reaction to surgery can cause inflammation, immune response, and even organ failure. Managing these responses well is key to avoiding complications after surgery.
The stress of surgery can also make existing health problems worse. So, it’s very important to carefully check the patient before surgery and take good care of them after.
Other High-Risk Surgical Procedures Just Below The Top Three
There are other surgeries that are very risky, even if they’re not in the top three. Operations like esophagectomy, multi-organ transplantation, and complex spinal reconstructions are very complex. They come with big risks.
Esophagectomy for Esophageal Cancer
Esophagectomy is a surgery to remove part of the esophagus. It’s often done for esophageal cancer. This surgery is very complex and risky. Risks include leakage, breathing problems, and even death.
The recovery is long and hard. Patients need a lot of care after surgery.
Multi-Organ Transplantation
Multi-organ transplantation is when you replace several organs at once. This could be liver and kidney or heart and lung transplants. It’s a very complex surgery.
It requires matching organs perfectly and managing immunosuppression carefully. This makes it a high-risk procedure.
Complex Spinal Reconstructions
Complex spinal reconstructions fix severe spinal problems or stabilize the spine after injury. These surgeries are very technical. They carry risks like nerve damage, infection, and hardware failure.
The recovery is long, with a big rehabilitation period. It’s a challenging surgery.
Even though they’re not in the top three, these surgeries are very risky. It’s important for patients and doctors to understand the risks and benefits. This helps make better decisions.
The Critical Role of Surgeon Experience in High-Risk Operations
The surgeon’s experience is key in high-risk operations. Surgeons with lots of experience can better handle the unexpected. They are ready for the challenges that come up during these surgeries.
Volume-Outcome Relationship in Complex Surgery
There’s strong evidence for the volume-outcome relationship in complex surgery. Hospitals and surgeons with more experience in certain procedures have better results. This shows how important experience and volume are in high-risk surgeries.
Research shows that surgeons who do more complex surgeries have fewer complications. They also have better survival rates for their patients. This is because they have honed their skills, perfected their techniques, and provide better care before and after surgery.
Choosing Between Specialized Centers and General Hospitals
Choosing between specialized centers and general hospitals matters for high-risk operations. Specialized centers, with their high-volume experience and teams, are often better for complex surgeries.
Patients in high-risk operations might do better at specialized centers. These places have surgeons with lots of experience in similar surgeries. While general hospitals are convenient and accessible, high-risk surgeries need the expertise of specialized centers.
How Modern Technology Is Reducing Risks in Major Surgery
Modern technology lets surgeons do complex operations with more precision and safety. New technologies have changed surgery, making it safer and better for patients.
Minimally Invasive Alternatives to Open Procedures
Minimally invasive alternatives are big steps forward from old open surgeries. They use smaller cuts, causing less damage and helping patients heal faster. Laparoscopic and robotic-assisted surgeries are now common, cutting down on risks and recovery times.
These new surgeries have many benefits. They lead to less blood loss, lower infection risks, and less pain after surgery. For instance, laparoscopic cholecystectomy is now a go-to for removing gallbladders, making open surgery less common.
Advanced Imaging and Navigation Systems
Advanced imaging and navigation systems are key in modern surgery. They give surgeons real-time data and detailed anatomy, helping them navigate complex areas. Tools like intraoperative MRI and CT scans help find and remove tumors more accurately.
Navigation systems, using 3D visualization, help surgeons understand anatomy and plan their moves. This is super important in neurosurgery and orthopedic surgeries, where being precise is everything.
- Improved accuracy in tumor removal
- Enhanced visualization of anatomical structures
- Real-time feedback during surgery
Anesthesia Considerations in High-Risk Surgical Cases
In high-risk surgeries, anesthesia is key. It needs careful management to avoid problems. Anesthesiologists play a big role in keeping patients safe during and after surgery.
They must know the patient’s health history and the surgery’s needs. Anesthesiologists must watch the patient’s vital signs closely to avoid issues like low blood pressure or breathing problems.
Anesthesia-Related Complications in Complex Surgery
Complications can happen for many reasons. These include the patient’s health, the anesthesia type, and the surgery’s complexity. Some common issues are:
- Respiratory problems, such as trouble breathing or failure
- Cardiovascular issues, including low blood pressure or heart stoppage
- Nerve damage or neuropathic pain
Modern Anesthetic Management Techniques
New ways to manage anesthesia have improved safety in high-risk surgeries. These include advanced monitoring, personalized anesthesia plans, and new ways to give anesthesia.
These modern methods help reduce risks and speed up recovery. A leading anesthesiologist said,
“The key to successful anesthesia management lies in careful planning, precise execution, and continuous monitoring.”
Patient Preparation and Selection for High-Risk Procedures
Success in high-risk procedures depends a lot on how well patients are prepared and selected. These surgeries carry big risks, so it’s key to make sure patients are as healthy as possible before, during, and after. This helps lower the chances of problems.
Pre-Operative Risk Reduction Strategies
Reducing risks before surgery is very important. Doctors check the patient’s health, including any ongoing health issues, diet, and habits like smoking or drinking. They might work on managing health problems, give advice on eating better, or help patients quit smoking.
| Risk Factor | Pre-Operative Strategy | Benefit |
| Smoking | Smoking cessation programs | Reduced pulmonary complications |
| Poor Nutrition | Nutritional counseling | Improved wound healing |
| Uncontrolled Diabetes | Optimization of glucose control | Reduced infection risk |
The Informed Consent Process for Dangerous Operations
The informed consent process is very important for high-risk surgeries. It means telling patients all about the surgery’s risks and benefits, other options, and what they can expect. This way, patients know what’s happening and can decide what’s best for them.
By focusing on patient preparation and selection, doctors can make high-risk surgeries safer and more successful. This not only keeps patients safer but also makes healthcare work better overall.
Conclusion
High-risk surgeries, like aortic dissection repair and craniotomy for brain tumors, need careful planning. These complex surgeries can save lives if done right.
Assessing surgical risk is key in preparing patients for these operations. Knowing what makes a surgery risky helps doctors lower these risks. This improves how well patients do after surgery.
Surgeries with high risks need skilled surgeons and the latest technology. Things like surgeon experience and new anesthesia methods help make these surgeries safer.
Getting ready for surgery is also important. Patients need to know the risks and benefits of their surgery. This helps them make smart choices about their treatment.
In the end, understanding the risks of high-risk surgeries is essential. With good planning and care, these surgeries can have good outcomes. Focusing on risk assessment and patient preparation can make care better for those facing these complex surgeries.
FAQ
What are the top riskiest surgeries?
The riskiest surgeries include aortic dissection repair, the Whipple procedure, and craniotomy for complex brain tumors. These are high-risk due to their complexity and high mortality rates.
What factors contribute to surgical risk?
Surgical risk depends on the patient’s health, age, and any existing conditions. The complexity of the surgery also plays a big role in increasing the risk of complications and death.
What is the mortality rate for aortic dissection repair?
The death rate for aortic dissection repair varies. It depends on the patient’s health and the surgery’s complexity. It’s one of the highest among heart surgeries.
What are the common complications of pancreatic surgery?
Pancreatic surgery complications include bleeding, infection, and pancreatic fistula. These can greatly affect recovery and survival chances.
How does surgeon experience impact outcomes in high-risk surgery?
Experienced surgeons have better results in high-risk surgeries. They have lower complication rates due to their skill and knowledge of complex procedures.
What role does modern technology play in reducing surgical risks?
Modern tech, like minimally invasive surgery and advanced imaging, reduces risks. It causes less tissue damage and improves accuracy.
What are the anesthesia considerations in high-risk surgical cases?
Anesthesia in high-risk surgeries depends on the patient’s health and the surgery’s complexity. Experienced anesthesiologists manage these risks carefully.
How can patients prepare for high-risk surgical procedures?
Patients should prepare by improving their health and getting a thorough check-up before surgery. Being well-informed about the procedure’s risks and benefits is also key.
What is the importance of informed consent in high-risk surgery?
Informed consent is vital in high-risk surgery. It ensures patients know the risks and benefits, helping them make informed decisions.
Are there any other high-risk surgical procedures beside the top three?
Yes, other risky surgeries include esophagectomy for esophageal cancer, multi-organ transplantation, and complex spinal reconstructions. These also carry significant risks and complications.
What is the significance of anatomical complexity in high-risk surgery?
Anatomical complexity is a big factor in high-risk surgery. It increases the risk of complications and makes the surgery more challenging for the surgeon.
How does physiological stress impact patients undergoing high-risk surgery?
Physiological stress can greatly affect patients in high-risk surgery. It increases the risk of complications and impacts recovery and outcome.
References
National Center for Biotechnology Information. Evidence-Based Medical Insight. Retrieved from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4191488/