Last Updated on December 2, 2025 by Bilal Hasdemir
Nearly 300,000 women are diagnosed with breast cancer in the United States each year. Many of them undergo breast cancer surgery, including total mastectomy.total mastectomy removalTop 10 Most Painful Surgeries to Recover From (Expert List)
Having a mastectomy surgical procedure can be scary. A total mastectomy removes the whole breast. This includes the nipple, areola, and most of the breast tissue. It’s often done to treat breast cancer or to prevent it in those at high risk.
We focus on giving our patients the best care and support. We make sure they get top-notch service and expertise in breast tissue removal.
Key Takeaways
- Total mastectomy involves removing the entire breast, including the nipple and areola.
- The procedure is often used to treat or prevent breast cancer.
- Our team provides personalized care and support throughout the process.
- Understanding what is removed during a total mastectomy is key for patients.
- We emphasize premium service quality and medical expertise.
Choosing to undergo a total mastectomy is a significant and often emotional decision.

Choosing to undergo a total mastectomy is a significant and often emotional decision.
Definition of Total Mastectomy
Total mastectomy, also called simple mastectomy, involves removing the whole breast. This includes the nipple, areola, and most of the skin over it. It’s different from other mastectomies and surgeries that try to save the breast.
The main goal of total mastectomy is to remove the breast tissue with cancer. This reduces the chance of cancer coming back. We make sure our patients know what the surgery involves and what to expect during recovery.
Choosing to undergo a total mastectomy is a significant and often emotional decision.
Choosing to undergo a total mastectomy is a significant and often emotional decision.
- Large tumors or many tumors in the breast.
- Cancer that has spread a lot in the breast.
- Genetic risks for breast cancer (like BRCA1 or BRCA2 gene mutations).
- Personal preference, if saving the breast isn’t possible or wanted.
We work closely with our patients to understand their unique situation. We provide personalized care that meets their specific needs and concerns.
The Anatomy of Breast Tissue

To understand what’s removed in a total mastectomy, knowing the breast’s anatomy is key. The breast is made up of different types of tissue.
Components of Breast Tissue
The breast has glandular, fatty, and connective tissue. Glandular tissue makes milk, fatty tissue shapes the breast, and connective tissue supports it. Knowing this helps us see how breast cancer impacts the breast.
Glandular tissue forms lobules for milk production. Fatty tissue varies, affecting the breast’s size and density. Connective tissue keeps the breast’s shape and position.
How Breast Tissue is Affected by Cancer
Breast cancer can hit any tissue type, causing different cancers. Carcinomas start in glandular tissue, while others begin in fatty or connective tissue. Cancer can change the breast’s look, feel, and health.
Cancer cells can spread to other areas. Knowing how cancer affects breast tissue helps choose the right treatment, like a total mastectomy.
Understanding breast anatomy and the effects of cancer can be challenging. Our team offers full support and care for mastectomy patients. We aim to give the best treatment and guidance on their journey.
What Happens During the Procedure
The journey to recovery after a total mastectomy is complex and involves both physical healing and emotional support.
Surgical Steps Involved
The total mastectomy process has several important steps. First, the surgeon makes an incision in the breast. This allows them to reach the tissue inside.
Next, the surgeon removes the breast tissue. This might include some skin and the nipple-areola area. Sometimes, they also take out lymph nodes from the armpit.
Surgical Steps at a Glance:
| Step | Description |
| 1. Incision | Making an incision to access breast tissue. |
| 2. Tissue Removal | Removing the breast tissue, possibly including some skin and the nipple-areola complex. |
| 3. Lymph Node Removal | Removing lymph nodes from the armpit if necessary. |
Anesthesia Used During Surgery
General anesthesia is usually used during a total mastectomy. This keeps the patient comfortable and safe during the mastectomy surgical procedure. The patient will be asleep, feeling no pain or discomfort.
Our team makes sure the mastectomy operation is done with great care. They follow the highest standards of surgery. General anesthesia is common for this breast surgery procedure. It ensures the patient stays comfortable the whole time.
What is Removed in a Total Mastectomy?
Total mastectomy is a surgery that removes the whole breast, including tissue and skin. It’s a key treatment for breast cancer. We’ll explain what’s removed and why it’s important.
Breast Tissue and Skin Removal
In a total mastectomy, the main goal is to take out the breast tissue. This includes the part that makes milk. The nipple and areola, which are part of the breast, are also removed. Sometimes, extra skin around the breast is taken off too, depending on the cancer’s size or other issues.
Removing the breast tissue is key to getting rid of cancer cells. The aim is to make sure all cancerous tissue is gone to stop cancer from spreading. How much skin is removed can change based on the surgery and the patient’s situation.
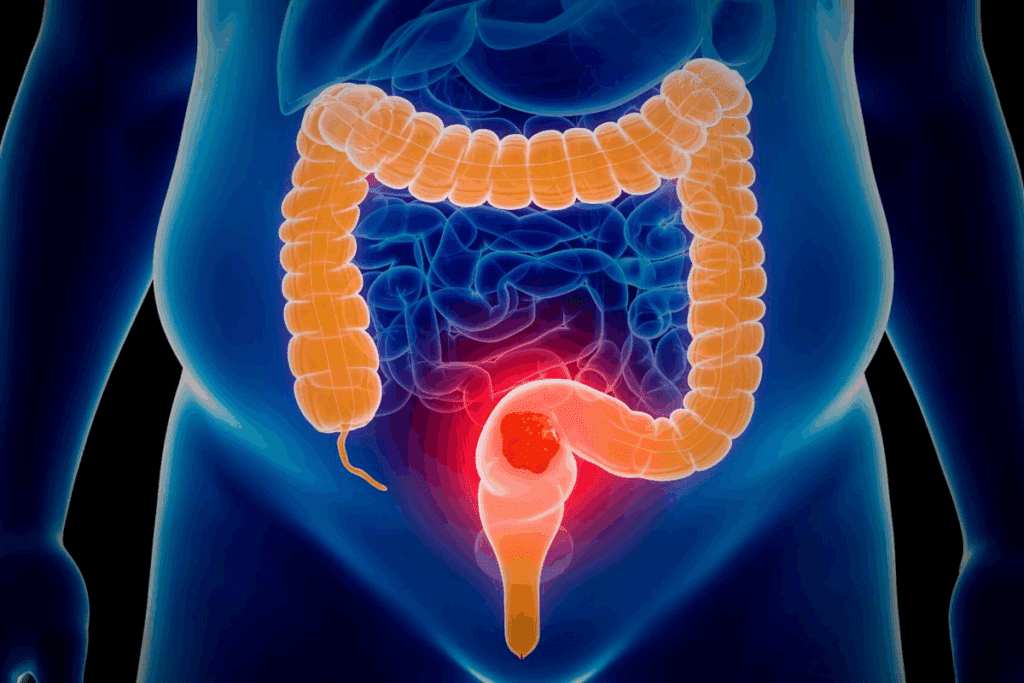
Lymph Nodes and Their Importance
Lymph nodes are important for our immune system. They catch harmful stuff, like cancer cells. In breast cancer, the lymph nodes under the arm are very important. During a total mastectomy, some of these nodes might be taken out to check if cancer has spread.
Checking and removing lymph nodes is vital for knowing the cancer’s stage. This info helps decide the best treatment, like if chemo or radiation is needed. How many lymph nodes are removed depends on the patient’s situation and cancer stage.
We know removing lymph nodes and breast tissue affects recovery and health. Our team is here to give full care and support during treatment.
Differences Between Total Mastectomy and Other Types
When it comes to breast cancer surgery, knowing the differences is key. Total mastectomy, or simple mastectomy, removes the whole breast. This includes the nipple, areola, and most of the skin.
We’ll look at how total mastectomy compares to other surgeries like lumpectomy and partial mastectomy. We’ll highlight the main differences and what they mean for patients.
Comparison with Lumpectomy
Lumpectomy, or breast-conserving surgery, takes out the tumor and a bit of tissue. But it keeps most of the breast. Total mastectomy, on the other hand, removes the whole breast.
The main differences are:
| Characteristics | Total Mastectomy | Lumpectomy |
| Extent of Tissue Removal | Entire breast removed | Only cancerous tumor and surrounding tissue removed |
| Breast Preservation | No | Yes, most of the breast is preserved |
| Follow-up Treatment | May not require radiation if mastectomy is performed | Often followed by radiation therapy |
Comparison with Partial Mastectomy
Partial mastectomy removes more tissue than lumpectomy but less than total mastectomy. It’s also called segmental mastectomy or quadrantectomy.
The main differences are:
| Characteristics | Total Mastectomy | Partial Mastectomy |
| Extent of Tissue Removal | Entire breast removed | A significant portion, but not all, of the breast removed |
| Impact on Breast Appearance | Significant change or loss of breast | Some change in breast shape or size |
| Reconstruction Options | Often followed by reconstruction surgery | May or may not require reconstruction, depending on the extent of removal |
It’s important for patients to understand these differences. This helps them make informed decisions about their treatment. We’re here to provide care and support every step of the way.
The journey to recovery after a total mastectomy is complex and involves both physical healing and emotional support.
Choosing to undergo a total mastectomy is a significant and often emotional decision.
Typical Recovery Timeline
After a total mastectomy, your body starts to heal. This healing time can vary for everyone. Knowing what to expect can make your recovery better.
The recovery time can last from weeks to months. In the first 2-4 weeks, your body recovers from the surgery. This is the initial healing phase.
- Immediate post-surgery recovery (1-2 weeks): Focus on managing pain, resting, and following post-operative instructions.
- Early recovery phase (2-4 weeks): Gradually increase activity levels, attend follow-up appointments, and monitor for any signs of complications.
- Late recovery phase (4-6 weeks and beyond): Continue to improve physically, consider rehabilitation or physical therapy if recommended, and emotionally adjust to changes.
Managing Pain and Discomfort
Managing pain is key for a comfortable recovery. We use a mix of medication and other methods to help with pain.
| Pain Management Strategies | Description | Benefits |
| Medication | Prescribed pain relief medication to manage post-surgical pain. | Effective in reducing pain, allowing for easier recovery. |
| Rest and Relaxation | Getting plenty of rest and avoiding strenuous activities. | Helps the body heal faster, reduces discomfort. |
| Follow-up Care | Regular check-ups with healthcare providers to monitor healing. | Ensures any complications are caught early, supports overall recovery. |
Emotional Impact of Total Mastectomy
Choosing to undergo a total mastectomy is a significant and often emotional decision.
Psychological Effects
The effects on the mind can be deep. Patients might see their body differently, which can hurt their self-confidence. They might feel sad or miss a part of themselves, like a loss of femininity or identity. It’s key for patients to recognize these feelings and look for help.
Everyone reacts differently to a mastectomy. Some might feel really upset, while others might feel free, if it’s part of fighting breast cancer. Getting support from doctors, loved ones, and friends is very important.
Support Systems
There are many ways to get help with the emotional side of a mastectomy. These include:
- Professional counseling to deal with tough feelings.
- Support groups to share stories and find common ground.
- Online places for info, advice, and connection.
- Family and friends for emotional support and help with daily tasks.
“The support I got from my family and the support group was priceless. It helped me face the emotional side of my mastectomy and come out stronger.”
A breast cancer survivor
By understanding the emotional side of a mastectomy and using the help available, patients can move forward in their healing journey.
Aftercare and Follow-up
The journey doesn’t end with the surgery. Aftercare and follow-up appointments are key to watch healing and catch any issues early. We know recovery can be tough, and we’re here to help every step of the way.
Importance of Follow-up Appointments
Follow-up appointments after breast surgery are very important. They let us check how you’re healing, remove any stitches or drains, and look for any complications. These visits also give you a chance to talk about any worries or questions you have about getting better.
Regular follow-up helps us catch any problems quickly, making sure you get the best results. We ask that you stick to your follow-up appointments to help your recovery go smoothly.
Self-Care Tips Post-Surgery
Self-care is also a big part of getting better after surgery. Here are some self-care tips to help with healing:
- Rest and avoid doing too much
- Eat a balanced diet to help your body heal
- Drink lots of water to stay hydrated
- Use pain medicine as told to manage pain
- Watch the surgical area for any signs of infection
The journey to recovery after a total mastectomy is complex and involves both physical healing and emotional support.
Long-term Effects of Total Mastectomy
It’s important for patients to know what to expect after a total mastectomy. This surgery can lead to big changes in how you feel and live. These changes can affect your daily life and how you move.
Physical Changes to Expect
Patients may see many physical changes after a total mastectomy. These can include scarring, changes in how you feel sensations, and lymphedema if lymph nodes are taken out. How much these changes affect you can depend on your surgery and your body.
- Scarring: The scar from the surgery can be big and take time to heal.
- Changes in Sensation: You might feel numbness or different sensations in your chest.
- Lymphedema: If lymph nodes are removed, you might get swelling in your arm, called lymphedema.
Lifestyle Adjustments Necessary
After a total mastectomy, you’ll need to make some lifestyle changes. You might need to change how you dress, what you do every day, and even how you exercise. Physical therapy can help you get stronger and move better.
- Clothing Choices: You might want to wear clothes that fit your new body better.
- Exercise Regimens: Start with gentle exercises, but always listen to your doctor’s advice.
- Emotional Support: Joining support groups can offer emotional support and helpful tips.
| Aspect | Pre-Mastectomy | Post-Mastectomy |
| Physical Activity | Normal activity level | May need to adjust intensity and type of exercise |
| Clothing | Normal clothing choices | May prefer prosthetic or reconstructive options |
| Emotional Well-being | Variable | May require additional support and counseling |
The Role of Reconstruction Surgery
Choosing to undergo a total mastectomy is a significant and often emotional decision.
Options for Breast Reconstruction
There are many breast reconstruction options to consider. These include:
- Implant-based reconstruction: This uses saline or silicone implants to make a new breast.
- Autologous tissue reconstruction: This method uses your own tissue, often from the abdomen, back, or buttocks, to build the breast.
- Combination reconstruction: Some people might choose a mix of implant and autologous tissue reconstruction.
Timing of Reconstruction After Mastectomy
Deciding when to have reconstruction surgery is also important. You can choose between:
- Immediate reconstruction: Done right after the mastectomy.
- Delayed reconstruction: Scheduled later, after treatments like chemotherapy or radiation therapy.
When thinking about mastectomy and reconstruction, talk to your healthcare team. This includes a plastic surgeon. They can help you decide what’s best for you, based on your health, body type, and what you prefer.
Resources for Patients Considering Mastectomy
Patients thinking about or going through total mastectomy have many resources to help them. We offer full care and connect them with important support groups.
Support Networks
Support groups for breast cancer patients are a safe place to share and get emotional support. They are available both in-person and online, meeting different needs and likes.
Educational Resources
There are many educational materials on mastectomy, like online resources and printed guides from trusted organizations. These help patients understand their situation and treatment choices. We suggest checking out these resources to make informed care decisions.
Using these resources, patients can go through their treatment with confidence and support.
FAQ
Choosing to undergo a total mastectomy is a significant and often emotional decision.
A total mastectomy is a surgery that removes the whole breast. This includes the tissue, nipple, and areola.
Choosing to undergo a total mastectomy is a significant and often emotional decision.
It’s often used to treat breast cancer, when the cancer is widespread. It’s also a choice for those at high risk of breast cancer.
What is the difference between a total mastectomy and a lumpectomy?
A total mastectomy removes the whole breast. A lumpectomy takes out just the tumor and some nearby tissue.
Will I need to have lymph nodes removed during a total mastectomy?
Yes, if cancer has reached the lymph nodes. Removing them helps in planning treatment and understanding the cancer’s stage.
What type of anesthesia is used during a total mastectomy?
General anesthesia is used. It keeps you comfortable during the surgery.
How long does it take to recover from a total mastectomy?
Recovery time varies, but it’s usually weeks to months. Pain can be managed with medicine and other methods.
Can I have reconstruction surgery after a total mastectomy?
Yes, reconstruction is an option. The timing and type depend on your health and preferences.
What are the long-term effects of a total mastectomy?
You might experience scarring and numbness. There can also be emotional and psychological impacts. Lifestyle changes may be needed.
Are there support systems available for patients undergoing total mastectomy?
Yes, there are support groups, communities, and educational materials. They help with the treatment and recovery journey.
How important are follow-up appointments after a total mastectomy?
Follow-up appointments are very important. They help ensure a smooth recovery and check for cancer recurrence.
What self-care tips are recommended after a total mastectomy?
Rest well, manage pain, and follow a healthy lifestyle. These tips promote overall well-being.
Can I undergo breast reconstruction surgery immediately after total mastectomy?
Immediate reconstruction is possible for some. It depends on your health and the extent of the mastectomy.
National Center for Biotechnology Information. Evidence-Based Medical Insight. Retrieved from https://www.ncbi.nlm.nih.gov/books/NBK538212/