Last Updated on November 20, 2025 by Ugurkan Demir

A BMT (Bone Marrow Transplant) is a special medical treatment. It replaces unhealthy bone marrow with healthy stem cells. This helps treat diseases like leukemia, lymphoma, and multiple myeloma. Learn what a transplant of bone marrow is, how it’s done, and what recovery looks like after BMT.
The term BMT means ‘bone marrow transplant.’ It’s a way to put healthy blood-making cells into the body. This replaces bone marrow that’s not making enough healthy blood cells. At Liv Hospital, we focus on the patient’s needs and medical skills in every transplant journey. We offer hope and new starts for those with serious blood diseases.
Key Takeaways
- BMT stands for Bone Marrow Transplant, a medical treatment that replaces unhealthy bone marrow with healthy stem cells.
- The procedure is used to treat various blood-related diseases, including leukemia and lymphoma.
- BMT involves infusing healthy blood-forming stem cells into the body.
- Liv Hospital provides patient-centered care and medical expertise for BMT patients.
- A BMT can offer hope and new beginnings for patients with serious blood-related diseases.
Understanding BMT: The Medical Definition and Terminology
BMT, or Bone Marrow Transplant, is a complex medical treatment for serious health issues. Patients and their families need to understand BMT. This helps them navigate the treatment’s complexities.
A BMT replaces damaged or diseased bone marrow with healthy cells. These cells can come from the patient (autologous transplant) or a donor (allogeneic transplant). This treatment is a key hope for many patients around the world.
What BMT Stands For in Medical Terms
In medical terms, BMT means Bone Marrow Transplant. It involves putting healthy bone marrow cells into the body to replace damaged ones. The terms “BMT” and “stem cell transplant” are often used together, but they’re not the same.
Knowing what BMT means is key to understanding its importance. The term shows the treatment’s complexity and its role in treating different medical conditions.
The History and Evolution of Bone Marrow Transplantation
The history of BMT started in the mid-20th century. The first successful transplant was in 1968. The field has grown a lot, thanks to new medical technologies and research.
At first, BMT was mainly for blood cancers like leukemia. Now, it also treats genetic disorders and autoimmune diseases. The treatment has improved a lot, thanks to better donor matching and care after the transplant.
Today, BMT is seen as a life-saving option for many conditions. Research keeps making the treatment safer and more effective for patients everywhere.
The Function of Bone Marrow and Why Transplants Are Necessary
Bone marrow is a spongy tissue in our bones. It makes blood cells like red, white, and platelets. Knowing this helps us see why bone marrow transplants are so important.
The Role of Bone Marrow in the Human Body
Bone marrow is key to making blood cells. Red blood cells carry oxygen, white blood cells fight infections, and platelets help blood clot. When it works right, our health stays good.
Bone marrow also has stem cells. These are the first steps in making blood cells. Keeping these stem cells healthy is vital.
When a Transplant Becomes Medically Necessary
A bone marrow transplant is needed when one’s marrow is sick or damaged. This often happens with leukemia, lymphoma, or aplastic anemia. When this happens, the marrow can’t make healthy blood cells.
Doctors decide on a transplant based on the patient’s health. For many, it’s a chance to live a healthier life without their old condition’s problems.
Thanks to new tech and understanding, bone marrow transplants are now safer and more effective. They’re a key treatment for many diseases.
Medical Conditions Treated with BMT
Bone marrow transplantation (BMT) is a key treatment for serious diseases. It’s used to treat blood cancers and bone marrow disorders. BMT’s ability to tackle different health issues makes it a vital part of modern medicine.
Blood Cancers: Leukemia and Lymphoma
BMT is a main treatment for blood cancers like leukemia and lymphoma. Leukemia is when white blood cells grow too much. Lymphoma affects the lymphatic system and comes in two main types. BMT can cure these diseases by replacing bad marrow with good cells.
Choosing BMT for leukemia or lymphoma depends on several things. These include the disease’s stage, the patient’s age, and health. We pick BMT when other treatments have not worked or are unlikely to cure.
Bone Marrow Disorders: Aplastic Anemia and Others
Bone marrow disorders, like aplastic anemia, are also treated with BMT. Aplastic anemia happens when the bone marrow can’t make blood cells. This leads to severe anemia, infections, and bleeding. BMT can fix this by replacing the bad marrow with healthy donor cells.
Other disorders, like myelodysplastic syndromes and genetic diseases, may also benefit from BMT. The goal is to fix the marrow problems and improve the patient’s quality.
Other Conditions That May Benefit from BMT
BMT is also being looked at for treating other conditions. This includes multiple myeloma, a blood cancer, and genetic disorders that affect blood cell production. BMT aims to cure these conditions and improve the patient’s life.
| Condition | Description | Role of BMT |
| Leukemia | A cancer of the blood or bone marrow | Potentially curative by replacing diseased marrow |
| Lymphoma | A cancer of the lymphatic system | Provides a potentially curative option |
| Aplastic Anemia | Bone marrow failure | Restores normal bone marrow function |
Types of Bone Marrow Transplants
It’s important to know about the different bone marrow transplants. They are a big help for people with blood cancers and other serious diseases. Knowing about them helps patients and doctors make the best choices.
Autologous Transplants: Using Your Own Stem Cells
An autologous transplant uses your own stem cells. It’s often for patients with cancer, like multiple myeloma or lymphoma. The disease affects the bone marrow, but your stem cells can fix it after high-dose chemotherapy.
This method lets doctors use strong chemotherapy to kill cancer cells. But you need to have healthy stem cells collected before the treatment. You also need to be well enough for the procedure.
Allogeneic Transplants: Donor-Sourced Stem Cells
An allogeneic transplant uses stem cells from a donor. This donor can be a family member, someone unrelated, or from a registry. The donor’s stem cells replace your damaged bone marrow. This transplant can cure some diseases but has risks like graft-versus-host disease (GVHD).
Haploidentical and Cord Blood Transplants
Haploidentical transplants use stem cells from a half-matched donor, often a family member. They’re becoming more common because they work well, and more people can donate. Cord blood transplants use stem cells from a newborn’s umbilical cord. Both offer hope for patients without a fully matched donor.
These newer transplants give more options to patients. They offer hope to those who didn’t have a suitable donor before.
| Type of Transplant | Source of Stem Cells | Key Characteristics |
| Autologous | Patient’s own cells | Less risk of GVHD, suitable for certain cancers |
| Allogeneic | Donor cells | Potential cure, risk of GVHD, requires HLA matching |
| Haploidentical | Half-matched donor cells | Increasingly popular, wider donor availability |
| Cord Blood | Umbilical cord cells | Alternative for patients without a matched donor |
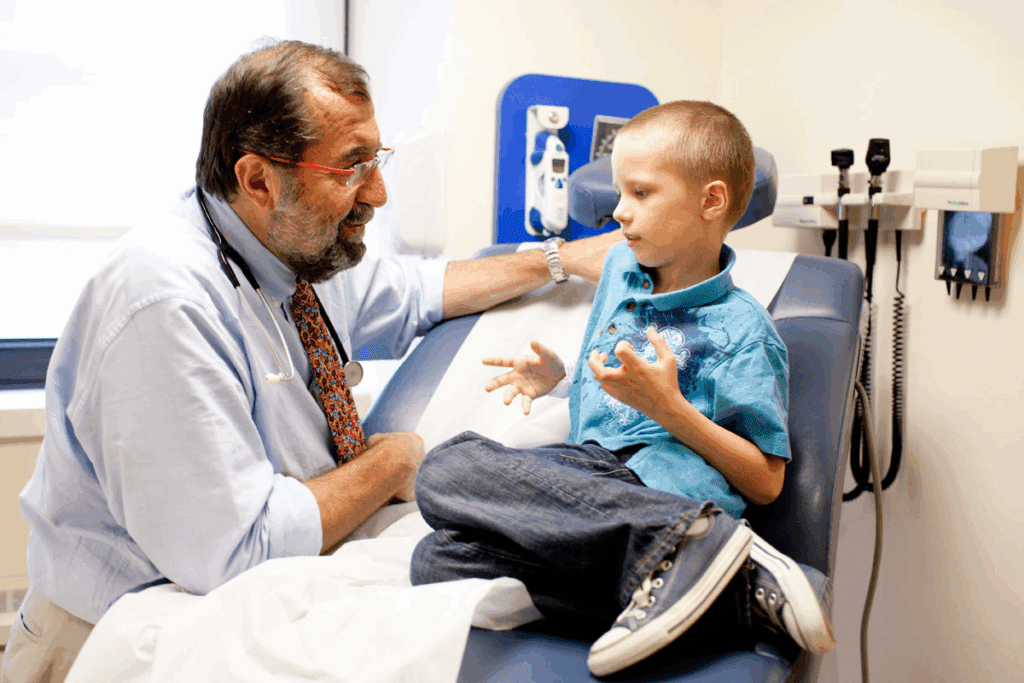
The Donor Selection Process for BMT
The success of a bone marrow transplant (BMT) depends a lot on choosing the right donor. This process is key to the transplant’s success and the patient’s health.
Bone marrow from a close relative is usually the first choice for BMT. This is because relatives share more genetic markers. Siblings or parents are more likely to match well.
Why Bone Marrow Collected From a Close Relative Is Often Preferred
A relative is often the first choice for a donor. This is because they might share more genes. This similarity can lower the risk of graft-versus-host disease (GVHD).
Genetic similarity between the donor and the recipient can significantly improve transplant outcomes.
HLA Matching and Compatibility Factors
HLA matching is key to matching the donor and recipient. Human Leukocyte Antigen (HLA) typing checks for genetic markers important for the immune system. A close match is vital for avoiding GVHD and ensuring the transplant works.
The process tests for several HLA loci to check compatibility. The closer the match, the lower the risk of complications.
The National Marrow Donor Program and Donor Registries
For those without a family donor, donor registries are essential. The National Marrow Donor Program (NMDP) is a big registry. It helps patients from different backgrounds find a match.
The NMDP and other registries work hard to find donors for patients. They help make sure patients have access to as many possible donors.
Modern Methods of Stem Cell Collection
The field of bone marrow transplantation (BMT) has changed a lot. New ways of collecting stem cells are key to this change. These methods make the process better and less painful for patients.
Peripheral Blood Stem Cell Collection: The 95% Solution
Studies show that over 95 percent of BMTs now use peripheral blood stem cell collection. This method moves stem cells into the blood for collection. It’s a big step forward, making the process less harsh than old methods.
To start, special drugs are given to move stem cells into the blood. When there are enough stem cells, the collection begins. This method is precise but preferred for its success and shorter recovery times.
Traditional Bone Marrow Harvesting Techniques
Even though new methods are common, traditional bone marrow harvesting techniques are sometimes used. This old method takes bone marrow from the hipbone under anesthesia. It’s more invasive and takes longer to recover, but it’s an option when new methods can’t be used.
Advances in Reducing Patient Discomfort During Collection
New ways of collecting stem cells have made the process better and less painful. Improvements in how stem cells are mobilized and collected have helped a lot. We’re seeing more ways to make the process comfortable and safe for patients.
These new methods are a big leap forward in BMT. They improve patient results and open up more treatment options. As technology keeps getting better, we’ll see even more progress in stem cell collection, helping BMT patients even more.
The Transplant of Bone Marrow: Step-by-Step Procedure
Bone marrow transplantation is a complex process. It requires careful preparation and execution. We will guide you through the key steps involved in this life-saving treatment.
Pre-Transplant Evaluation and Preparation
Before a bone marrow transplant, patients must undergo a thorough evaluation. This checks their overall health and if they’re suitable for the procedure. Tests include checking organ function, infectious disease screening, and cancer status, if applicable.
We also prepare patients psychologically. We provide them with detailed information about what to expect during and after the transplant.
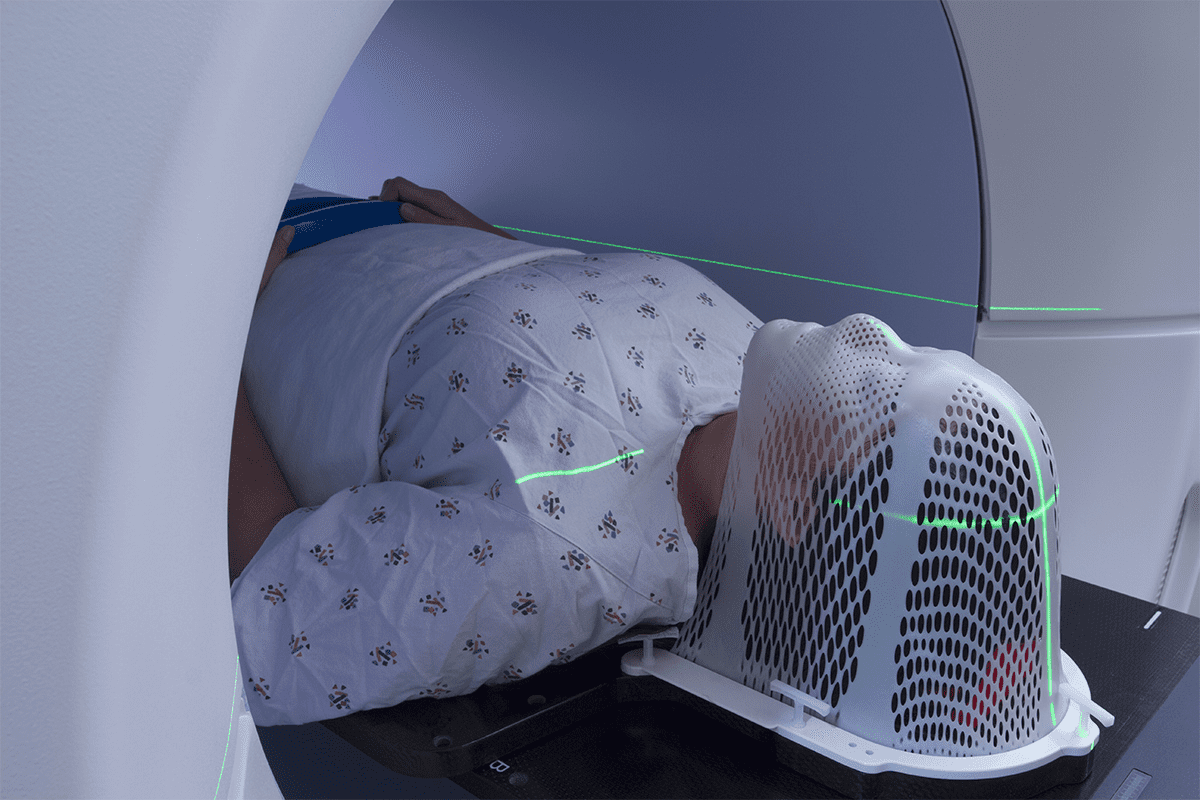
Conditioning: Chemotherapy and Radiation
The conditioning regimen is a critical step. It involves administering high-dose chemotherapy and/or radiation therapy. This process aims to eradicate diseased cells and suppress the immune system to prevent rejection of the new marrow.
While conditioning is intense, we take measures to manage side effects. We ensure patient comfort throughout the process.
The Actual Transplantation Process
The bone marrow transplant infusion is a relatively straightforward process. It’s similar to a blood transfusion. The collected stem cells are infused into the patient’s bloodstream through a central line.
This procedure is typically painless. Some patients may experience mild discomfort or an allergic reaction. We monitor these closely.
Is BMT Painful? What Patients Experience During the Procedure
While the transplant infusion itself is generally painless, patients may experience discomfort during the conditioning phase. Side effects like mucositis or gastrointestinal issues can cause discomfort.
We provide supportive care to manage these side effects. We ensure that patients remain as comfortable as possible throughout their treatment.
By understanding the step-by-step process of bone marrow transplantation, patients can better prepare themselves for this potentially life-saving treatment. Our team is dedicated to providing the highest level of care and support throughout every stage of the transplant process.
Post-Transplant Care and Recovery
Post-transplant care is key after a bone marrow transplant. It involves watching over patients closely. This ensures a smooth recovery and helps avoid complications.
The Critical First 100 Days After BMT
The first 100 days after a transplant are very important. We watch how the new bone marrow works. This helps us catch any problems early.
During this time, we focus on a few key things:
- Monitoring Blood Counts: We check blood counts often to see if the bone marrow is making healthy cells.
- Infection Prevention: Patients stay isolated to avoid infections. They might also get antibiotics or antifungals.
- Managing Side Effects: We work hard to control side effects like nausea, tiredness, and GVHD.
Managing Side Effects and Possible Complications
Handling side effects and complications is vital for recovery. Some common issues include:
- Graft-versus-host disease (GVHD), when the donor’s immune cells attack the body.
- Infections, because the immune system is weakened.
- Damage to organs like the liver or lungs.
We help patients manage these issues with medicine, lifestyle changes, and other treatments.
Long-term Follow-up Care for BMT Patients
Long-term care is important for BMT patients. It helps catch late effects and keeps them healthy. This includes regular check-ups and watching for signs of relapse.
Long-term care includes:
- Regular Follow-ups: We schedule appointments to check on patients’ health and catch problems early.
- Late Effects Monitoring: We screen for late transplant effects, like secondary cancers or organ problems.
- Supportive Care: We offer emotional and psychological support to patients and their families.
Comprehensive post-transplant care greatly improves BMT patient outcomes. It also enhances their quality of life.
Success Rates and Bone Marrow Cure
It’s important to know how well BMT works to see if it can cure diseases. A bone marrow transplant can cure some diseases and put others into remission. The success of BMT depends on many things, like the disease, the patient’s age and health, and the transplant type.
Factors Affecting BMT Outcomes and Survival Rates
Several key factors influence the outcomes of BMT. These include:
- The type of transplant: autologous, allogeneic, or haploidentical
- The patient’s overall health and age
- The stage and type of the underlying disease
- The degree of HLA matching between donor and recipient
These factors can greatly affect how well BMT works. For example, younger patients with fewer health problems usually do better.
Disease-Specific Success Rates and Statistics
Disease-specific success rates give us important information about BMT outcomes. For example:
- For certain types of leukemia, BMT can offer a cure rate of up to 50% in some cases.
- Patients with aplastic anemia have shown significant improvement in survival rates following BMT.
- For multiple myeloma, BMT can extend survival and improve quality of life.
These statistics show that BMT can be a life-saving treatment option.
Quality of Life After Successful BMT
Successful BMT can greatly improve a patient’s quality of life. Many patients can go back to their normal activities and feel healthier. But, some may face long-term side effects, such as:
- Chronic graft-versus-host disease (GVHD)
- Increased risk of infections
- Hormonal imbalances
It’s important to have long-term follow-up care to manage these side effects and ensure the best quality of life.
We know that every patient’s experience is different, and outcomes can vary. But BMT is getting better, and it offers hope to those facing serious diseases.
Conclusion: The Future of Bone Marrow Transplantation
Looking ahead, bone marrow transplantation (BMT) is set for big improvements. New research and technologies will make treatments safer and more effective. This means better chances for patients to survive and thrive.
Already, BMT has seen big strides in success rates. As we learn more about the immune system and genetics, we’ll see even better treatments. These advancements will help patients live better lives after BMT.
The future of BMT depends on ongoing improvements in techniques and care. We’re excited for the future, where patients will receive even better care and have better outcomes. This progress will be driven by discoveries and innovations in the field.
FAQ
What does BMT stand for in medical terms?
BMT stands for Bone Marrow Transplant. It’s a treatment that replaces a patient’s bone marrow with healthy stem cells.
What is the purpose of a bone marrow transplant?
A bone marrow transplant aims to replace damaged or diseased marrow. This helps the body make healthy blood cells again.
What conditions are treated with BMT?
BMT treats blood-related diseases like leukemia and lymphoma. It also helps with multiple myeloma, aplastic anemia, and some genetic disorders.
What are the different types of bone marrow transplants?
There are several types. These include autologous (using the patient’s own stem cells), allogeneic (from a donor), haploidentical (from a half-matched donor), and cord blood transplants (from a newborn’s umbilical cord).
Why is bone marrow collected from a close relative often preferred?
Using a close relative’s bone marrow is often preferred. This is because it’s more likely to be genetically compatible. This reduces the risk of complications and improves transplant success.
What is HLA matching, and why is it important?
HLA matching is a test to check if the donor and patient are compatible. It’s key to reducing the risk of complications and ensuring a successful transplant.
How are stem cells collected for BMT?
Stem cells are collected through peripheral blood stem cell collection. This involves mobilizing stem cells into the bloodstream. Traditional bone marrow harvesting is also used, but less often.
Is BMT painful?
The transplant process itself is usually painless, like a blood transfusion. But patients might feel some discomfort during the procedure. This is managed with proper care.
What is the success rate of BMT?
BMT success rates vary. They depend on the disease, the patient’s age and health, and the transplant type. Looking at disease-specific success rates can give insights into possible outcomes.
What is the future of bone marrow transplantation?
The future of BMT looks bright. Ongoing research aims to improve outcomes and reduce complications. This could lead to better survival rates and quality of life for patients.
References
- Fuchs, E. J., & Appelbaum, F. R. (2023). Hematopoietic stem cell transplantation. StatPearls Publishing. https://www.ncbi.nlm.nih.gov/books/NBK536951/