Last Updated on December 1, 2025 by Bilal Hasdemir
Rhabdomyosarcoma is a rare and aggressive cancer that affects muscle tissue.Trauma causing rhabdomyosarcomaIdentifying the Most Common Trauma Surgeon Procedures It mainly happens in children and teens. A surprising fact is that rhabdomyosarcoma makes up about 3% of all childhood cancers. This makes it a big worry for families and doctors.
Studies suggest that traumatic events might trigger rhabdomyosarcoma in some cases. The exact ways this happens are not yet clear. But, knowing how trauma and rhabdomyosarcoma are linked is key to finding better treatments.
We will look into the latest research on trauma and rhabdomyosarcoma. This will give us a better understanding of this rare and complex cancer.
Key Takeaways
- Rhabdomyosarcoma is a rare and aggressive cancer affecting muscle tissue.
- Traumatic events may potentially trigger the development of rhabdomyosarcoma.
- Understanding the causes of rhabdomyosarcoma is key to effective treatment.
- Current research is exploring the link between trauma and rhabdomyosarcoma.
- Rhabdomyosarcoma accounts for a small percentage of childhood cancers.
Understanding Rhabdomyosarcoma: A Complete Overview
Rhabdomyosarcoma is a rare cancer that affects muscle cells. It’s most common in kids and teens. This cancer is a challenge to diagnose and treat, mainly because it often happens in young people.
Definition and Classification of Rhabdomyosarcoma
Rhabdomyosarcoma is classified into several subtypes based on its look under a microscope. The main types are embryonal, alveolar, and spindle cell/sclerosing rhabdomyosarcoma. Each type has its own signs and treatment plans.
The embryonal subtype is the most common in kids. It often shows up in the head and neck or in the urinary system. Alveolar rhabdomyosarcoma, on the other hand, is more common in older kids and young adults. It usually appears in the arms or legs.
“The classification of rhabdomyosarcoma is key for choosing the right treatment and predicting how well a patient will do.”
Prevalence and Demographics
Rhabdomyosarcoma makes up about 3-5% of all childhood cancers. It’s a rare but serious cancer in kids. The most cases happen in children under 10 years old.
| Age Group | Incidence Rate |
| 0-9 years | 4.5 per million |
| 10-19 years | 2.1 per million |
| 20+ years | 1.3 per million |
Common Symptoms and Presentation
The symptoms of rhabdomyosarcoma depend on where the tumor is. Common signs include a noticeable lump, pain, or swelling. Sometimes, the tumor can also cause problems like nerve damage or trouble with the urinary system.
- Pain or swelling
- Painful or painless mass
- Symptoms related to tumor location (e.g., neurological deficits, urinary obstruction)
Getting a diagnosis early is very important. It helps with treatment and better outcomes. It’s vital for doctors and families to recognize the signs and seek help quickly.
The Biology of Rhabdomyosarcoma Development

Learning about rhabdomyosarcoma’s biology is key to better treatments. We’ll look at the main factors that lead to this disease.
Cellular Origins of Rhabdomyosarcoma
Rhabdomyosarcoma starts from skeletal muscle cells. These cells get genetic changes that mess up their growth and development.
These changes are linked to muscle growth. RMS cells often show signs of muscle cell development. This shows they come from muscle cells.
Genetic Mutations Associated with RMS
Genetic changes are vital in rhabdomyosarcoma. The PAX and FOXO1 genes are often affected.
Some important genetic changes are:
- PAX3-FOXO1 fusion, common in alveolar RMS
- PAX7-FOXO1 fusion, also found in alveolar RMS
- Changes in TP53, MDM2, and other genes that control cell growth
Tumor Growth Mechanisms
Rhabdomyosarcoma tumors grow through many processes. These include:
- Uncontrolled cell growth
- Stopping cells from dying naturally
- Creating new blood vessels for the tumor
- Spreading to other parts of the body
Knowing these growth methods helps in making targeted treatments for rhabdomyosarcoma.
Established Risk Factors for Rhabdomyosarcoma
Rhabdomyosarcoma can develop due to several risk factors. These include genetic, environmental, and congenital factors. Knowing these risk factors helps us find people at higher risk. It also guides us in how to prevent it.
Genetic Predisposition
Genetics play a big role in rhabdomyosarcoma. Certain genetic syndromes, like Li-Fraumeni syndrome and Neurofibromatosis type 1, raise the risk. These syndromes often come from mutations in genes that control cell growth.
Environmental Exposures
Some environmental factors may increase rhabdomyosarcoma risk. While not as clear as genetics, ionizing radiation and chemical exposures are possible risks. For example, ionizing radiation in kids can raise cancer risk, including rhabdomyosarcoma.
Congenital Anomalies
Certain birth defects may also raise rhabdomyosarcoma risk. These defects might increase cancer risk, but the exact reasons are not yet clear. Ongoing research aims to understand this link better.
Trauma Causing Rhabdomyosarcoma: Examining the Hypothesis
To understand if trauma can cause rhabdomyosarcoma, we need to look at history, current studies, and case reports. The idea that injury might lead to this rare cancer has sparked debate and interest.
Historical Perspectives on Trauma and Cancer
For centuries, doctors have wondered if injury can cause cancer. Early studies hinted at a possible link between injury and tumors. But these early findings were mostly based on stories, not solid research.
In the late 1800s and early 1900s, doctors reported cases of sarcomas, like rhabdomyosarcoma, at injury sites. These reports helped build the idea that injury might start or help tumors grow.
Current Scientific Understanding
Now, scientists are studying the link between trauma and rhabdomyosarcoma with better methods. They’re looking into how trauma might lead to cancer through biological processes.
Research shows that trauma can cause long-term inflammation, which is a cancer risk. This involves the immune system, cell repair, and genetic changes that might lead to cancer.
| Mechanism | Description | Potential Role in Cancer |
| Chronic Inflammation | Prolonged inflammatory response following trauma | May contribute to oncogenesis |
| Genetic Mutations | DNA damage during cellular repair post-trauma | Could lead to cancer-causing mutations |
| Immune System Dysregulation | Trauma-induced changes in immune function | May impair cancer surveillance |
Case Reports and Anecdotal Evidence
Many case reports show rhabdomyosarcoma after big injuries. These stories are interesting but not strong evidence because they’re based on individual experiences.
Looking at these cases, the time from injury to cancer diagnosis varies a lot. This makes it hard to say for sure if injury causes cancer. Yet, these stories keep the conversation going about a possible link.
Scientific Evidence: Can Physical Trauma Initiate Cancer?
Recent studies have found a link between physical trauma and cancer. This is seen in trauma-induced tumors. We’ll look at how trauma affects cells, the role of inflammation, and DNA damage and repair.
Cellular Response to Trauma
Physical trauma sets off a healing process in the body. This involves many cell types, like immune cells and stem cells. The first step is inflammation, key to healing.
The body’s response to trauma is complex. Growth factors and cytokines help cells grow and change. But, this can lead to genetic mistakes if not controlled.
Inflammation and Cancer Development
Inflammation is both good and bad after trauma. It helps clear damaged cells but can also lead to cancer. Chronic inflammation can create a cancer-friendly environment.
Studies show that inflammation can damage DNA and help cancer grow. It can also promote blood vessel growth and cell movement. So, it’s important to understand the right amount of inflammation.
DNA Damage and Repair Mechanisms
DNA damage is a key step in cancer. Trauma can damage DNA directly or indirectly through inflammation. The body tries to fix this damage, but mistakes can lead to cancer.
How well the body repairs DNA damage varies. It depends on genetics and the environment. This affects the risk of cancer after trauma.
| Mechanism | Description | Impact on Cancer Development |
| Cellular Response to Trauma | Activation of immune cells, fibroblasts, and stem cells | Increased cell turnover, possible genetic errors |
| Inflammation | Release of inflammatory mediators | DNA damage, angiogenesis, enhanced cell migration and invasion |
| DNA Damage and Repair | Direct and indirect DNA damage, repair mechanisms | Mutations leading to tumorigenesis if repair is erroneous |
In conclusion, trauma can lead to cancer through cell response, inflammation, and DNA damage. Understanding these processes helps us see the risk of trauma-induced tumors. It’s key for prevention and early detection.
Research Studies on Trauma-Cancer Correlation
Many studies have looked into if trauma can lead to cancer. We’ll dive into what we know, focusing on big studies, lab findings, and what’s missing in research.
Epidemiological Studies
Big studies have checked if trauma is linked to cancer, like rhabdomyosarcoma. They look at lots of people to find patterns. Some say trauma might raise the risk of certain cancers, like soft tissue sarcomas.
But, it’s hard to say for sure if trauma causes cancer. Other things, like genes or the environment, might play a part too.
Laboratory Research Findings
Lab work has given us clues on how trauma might lead to cancer. It shows that injuries can cause inflammation and damage, which might help tumors grow. For example, studies on rhabdomyosarcoma point to genetic changes and changes in cells.
Also, lab tests show trauma can change how cells act, possibly starting or growing cancer. This shows the link between trauma and cancer is complex, with many factors at play.
Limitations in Current Research
Even with progress, there are big gaps in our knowledge. Many studies use old data or animal models, which might not fully capture human experiences. Also, cancer types and how people react to trauma vary a lot.
To move forward, we need more studies that follow people over time. We should include different groups and consider many factors. This will help us truly understand the link between trauma and cancer, leading to better prevention and treatment.
Childhood Cancer Causes: Focus on Rhabdomyosarcoma
It’s key to know what causes rhabdomyosarcoma in kids to find better treatments. Rhabdomyosarcoma is the top soft tissue sarcoma in children. It’s shaped by many factors.
Age-Related Incidence Patterns
Rhabdomyosarcoma can happen at any age in childhood. But, its occurrence changes with age. There are two main times when it’s more common: early childhood and during the teenage years.
These patterns show that different things might cause rhabdomyosarcoma at different times in a child’s life. For example, embryonal rhabdomyosarcoma, common in young kids, might be linked to genes or things before birth.
Developmental Factors in Pediatric RMS
How a child develops affects rhabdomyosarcoma. This includes genetics, the environment, and things that happen before or at birth.
- Genetic changes, like in the TP53 gene, can raise the risk of rhabdomyosarcoma.
- Exposure to certain chemicals or radiation might also play a role, though the link is not as clear.
Differences Between Adult and Childhood RMS
Rhabdomyosarcoma in adults and kids shares some traits but also has big differences. These differences affect how it’s treated and how well it responds to treatment.
- Kids with rhabdomyosarcoma usually have a better chance of recovery than adults. This is because of how the tumors behave and respond to treatment.
- The types of rhabdomyosarcoma also vary by age. Kids often get embryonal RMS, while teens and adults get alveolar RMS more.
These differences highlight the need for treatments that are tailored to a child’s age.
The Role of Inflammation in Post-Traumatic Cancer Development
It’s important to understand how inflammation can lead to cancer after trauma. This knowledge helps us find better ways to prevent and treat cancer. Inflammation is a natural response to injury, but it can go wrong and cause cancer.
Acute vs. Chronic Inflammation
Inflammation can be either acute or chronic. Acute inflammation happens quickly in response to injury or infection. It brings immune cells to the injured area fast. Chronic inflammation, on the other hand, lasts a long time and can damage tissues and even lead to cancer.
Here are the main differences between acute and chronic inflammation:
- Duration: Acute inflammation is short, while chronic inflammation can last for years.
- Effects on Tissue: Acute inflammation usually heals the tissue, but chronic inflammation can cause lasting damage.
- Cancer Risk: Chronic inflammation increases the risk of cancer because it exposes tissues to inflammation for a long time.
Inflammatory Mediators and Oncogenesis
Inflammatory mediators, like cytokines and prostaglandins, are key in cancer development. They can help cancer grow by:
- Causing genetic changes through reactive oxygen species (ROS).
- Helping cells grow and live longer.
- Creating new blood vessels for the tumor to grow.
Potential Therapeutic Implications
Knowing how inflammation leads to cancer after trauma opens up new treatment options. These could include:
- Anti-inflammatory therapies: Targeting inflammation to stop cancer before it starts.
- Antioxidant therapies: Lowering oxidative stress to protect DNA.
- Immunotherapies: Boosting the immune system to fight cancer cells.
By exploring these options, we can lower the risk of cancer after trauma and help patients recover better.
Trauma-Induced Tumors: Mechanisms and Evidence
It’s important to know how trauma can lead to tumors. This knowledge helps in preventing and treating these conditions. The link between physical trauma and tumors, like sarcomas, is a big focus in medical studies.
Proposed Pathways from Injury to Malignancy
There are several ways trauma might cause tumors. These include chronic inflammation, genetic damage, and problems with how cells repair themselves. Studies show that injury affects both the local tissue and the body’s overall response.
Chronic inflammation is a big player in cancer development. When tissues get hurt, the body’s first response is inflammation. If this goes on too long, it can cause genetic problems and lead to tumors.
“The chronic inflammatory response is a key factor in the development of cancer, as it can lead to the production of reactive oxygen species that damage DNA and promote genetic mutations.”
Animal Models of Trauma-Related Cancer
Animal studies have been key in understanding trauma and cancer. These studies let researchers control factors and look at how trauma leads to tumors.
A study found that mice with muscle injuries were more likely to get sarcomas. This supports the idea that trauma can lead to cancer under certain conditions.
| Study | Animal Model | Findings |
| Study A | Mice with muscle injury | Increased incidence of sarcomas |
| Study B | Rats with bone fracture | Development of osteosarcomas |
Distinguishing Features of Trauma-Associated Sarcomas
Trauma-related sarcomas are thought to have unique traits. These might include different genetic changes, where the tumor grows, and who gets them.
Genetic profiling shows that trauma-related sarcomas have special mutations. These might be connected to the body’s inflammatory and repair responses after injury.
Knowing these differences helps doctors diagnose and treat trauma-related sarcomas better. This could lead to better results for patients.
Psychological Trauma and Cancer: Is There a Connection?
We look into if traumatic events can lead to cancer. We focus on stress hormones and how they affect our immune system. Research suggests that psychological trauma might play a role in cancer development.
Stress Hormones and Immune Function
Stress hormones like cortisol and adrenaline help us react to trauma. But, being exposed to them for a long time can weaken our immune system. This might make it easier for cancer to grow.
Stress hormones can harm our immune system in many ways. For example, cortisol can lower the production of cytokines, which fight infections and cancer. Also, long-term stress can cause inflammation, which is a risk factor for cancer.
Psychoneuroimmunology Research
Psychoneuroimmunology (PNI) studies how our mind affects our immune system. PNI research has shown that psychological trauma can weaken our immune system. This could make us more likely to get cancer.
Studies in PNI have found that stress can change how our immune system works. This makes us more vulnerable to infections and cancer. This research helps us understand the link between trauma and cancer.
Holistic Perspectives on Cancer Development
Looking at cancer from a holistic view means considering physical, emotional, and environmental factors. Psychological trauma can deeply affect our health and might increase our cancer risk.
A holistic approach to cancer includes managing stress and supporting mental health. Research shows that people with strong social support and good stress management have a lower cancer risk. This approach is supported by studies on well-being and cancer prevention.
| Factor | Impact on Cancer Risk | Potential Mechanism |
| Chronic Stress | Increased | Immune suppression, inflammation |
| Social Support | Decreased | Enhanced immune function, stress reduction |
| Stress Management | Decreased | Reduced stress hormones, improved immune response |
Misattribution: When Cancer Is Discovered After Trauma
Trauma and cancer diagnosis can seem to happen together, but it’s not always clear why. When trauma strikes and then cancer is found, people wonder if the trauma caused the cancer. We need to look at the evidence carefully and consider many factors to figure out if there’s a link.
Coincidence vs. Causation
It’s important to know if trauma and cancer are just coincidental or if trauma actually caused the cancer. Coincidence means the cancer was there before the trauma. Causation means the trauma made the cancer happen.
To see if trauma caused cancer, we look at when the trauma and cancer happened, how bad the trauma was, and the person’s health history.
The Role of Increased Medical Attention
After trauma, people get a lot of medical checks. This can find cancers that were there but not noticed before.
More medical checks mean people might find cancer right after trauma. This can make it seem like trauma caused the cancer, when it might have been there all along.
Pre-existing Tumors Revealed by Trauma
Sometimes, trauma can make a hidden tumor show up. For example, a hit to a tumor area can cause pain or swelling. This leads to a diagnosis.
It’s key to understand that trauma just made a hidden tumor show up, not cause it. This matters a lot for treatment and legal issues.
Diagnostic Challenges: Distinguishing Trauma Effects from Early RMS
Diagnosing rhabdomyosarcoma (RMS) is tricky because it looks like trauma. Both can show similar signs, making it hard to figure out what’s wrong.
Similar Presenting Symptoms
Both trauma and RMS can cause pain, swelling, and stiffness. For example, trauma swelling might look like a tumor. Or, an RMS tumor might seem like trauma.
Common symptoms that may be confused include:
- Pain or tenderness in the affected area
- Swelling or a palpable mass
- Limited range of motion or weakness
Imaging and Diagnostic Techniques
Advanced imaging is key to telling trauma from RMS apart. MRI and CT scans help see how big the injury or tumor is.
| Imaging Technique | Use in Trauma | Use in RMS Diagnosis |
| MRI | Assesses soft tissue damage | Evaluates tumor extent and involvement |
| CT Scan | Evaluates bone fractures and internal injuries | Assesses tumor size and metastasis |
Biopsy is the best way to confirm RMS, by looking at tissue under a microscope.
Importance of Thorough Medical History
Knowing a patient’s medical history is key to telling trauma from RMS. Doctors need to look at past injuries, other health issues, and family health history.
A detailed medical history can provide clues that help in making an accurate diagnosis.
In conclusion, diagnosing RMS needs a close look at symptoms, imaging, and medical history. This helps doctors tell it apart from trauma effects.
Treatment and Prognosis of Rhabdomyosarcoma
Medical research has made big strides in treating rhabdomyosarcoma, a cancer mostly found in kids. These advances have greatly boosted survival rates. We’ll look at the latest treatments, what affects a patient’s outcome, and why ongoing care is key.
Standard Treatment Protocols
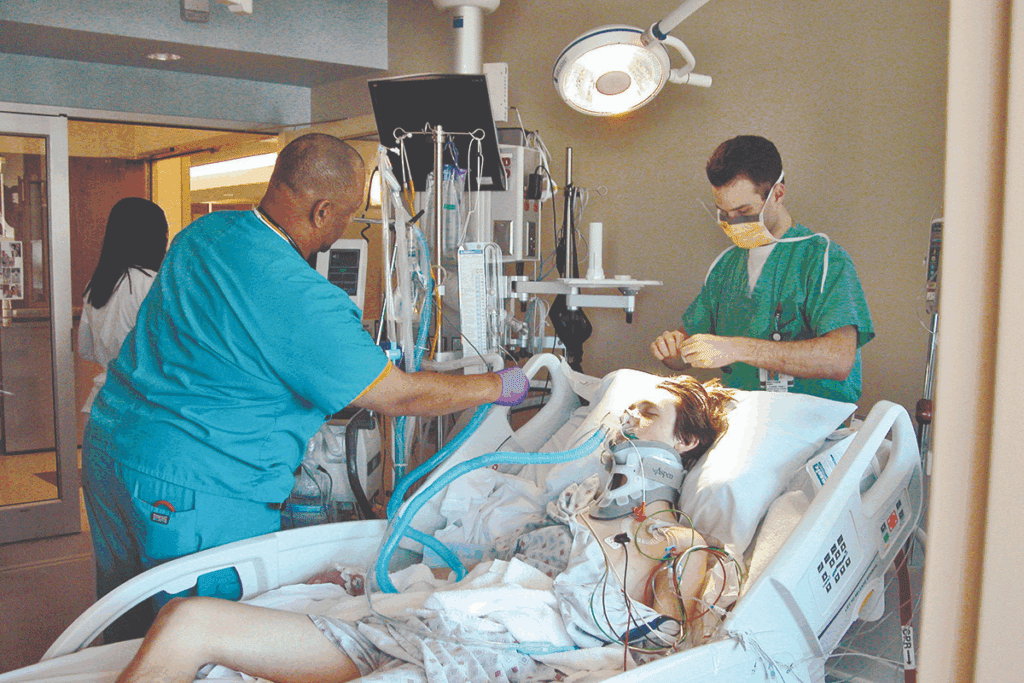
Treating rhabdomyosarcoma often means using surgery, chemotherapy, and radiation together. The plan is made just for each patient. It considers the tumor’s size, location, and the patient’s health.
Chemotherapy is a big part of fighting rhabdomyosarcoma. It helps stop the cancer from spreading and makes tumors smaller. Multi-agent chemotherapy regimens have been shown to work better in studies.
Survival Rates and Prognostic Factors
Thanks to better treatments and early detection, more kids are surviving rhabdomyosarcoma. The cancer’s type, how far it has spread, and the patient’s age are key factors. These help doctors predict how well a patient will do.
Those with localized disease usually have a better chance of beating the cancer. How well a patient responds to treatment also plays a big role in their long-term survival.
Long-term Follow-up Considerations
After treatment, ongoing care is vital for rhabdomyosarcoma patients. This care watches for late effects like second cancers, growth problems, and fertility issues.
A detailed follow-up plan is made for each patient. It’s based on their treatment history and needs. This way, any problems can be caught and treated quickly.
Medical and Legal Perspectives on Trauma-Induced Sarcomas
The study of trauma-induced sarcomas is complex. It involves both medical and legal views. We must look at many factors to understand these tumors fully.
Medicolegal Case Reviews
Medicolegal case reviews are key in linking trauma to cancer. They examine medical and legal records. This helps us understand if trauma caused a sarcoma.
A study showed that timing is important in these cases. It helps us guide future assessments.
Expert Testimony in Cancer Causation
Experts give opinions in legal cases about cancer. They look at the evidence and medical knowledge. Their views must be based on the latest science.
Expert opinions are vital in these cases. They help legal teams make better decisions.
Compensation and Insurance Considerations
Getting compensation for sarcoma caused by trauma is a big issue. Legal decisions affect insurance claims and compensation. We must handle these issues with care.
When trauma-induced sarcoma is proven, dealing with insurance is complex. It requires knowing both medical and legal sides. This includes understanding how insurance companies evaluate claims.
Conclusion: Current Understanding of Trauma and Rhabdomyosarcoma
Looking into the link between trauma and rhabdomyosarcoma shows it’s complex. Some studies hint at a possible connection between physical trauma and rhabdomyosarcoma. But, the proof is not strong enough yet.
Research on trauma and rhabdomyosarcoma has given us mixed answers. Some studies say trauma might start or speed up tumors in some people. But, we don’t know for sure how trauma affects cancer growth.
We need to keep studying to understand rhabdomyosarcoma better. This will help us find better ways to diagnose and treat this rare cancer. More research will help us help those fighting this tough disease.
FAQ
What is rhabdomyosarcoma, and how common is it?
Rhabdomyosarcoma is a rare cancer that affects muscle tissue. It’s most common in kids and teens. About 3% of all childhood cancers are rhabdomyosarcoma.
Can trauma cause rhabdomyosarcoma?
Research is ongoing on trauma and rhabdomyosarcoma. There’s no clear proof that trauma directly causes this cancer. Yet, some studies hint that physical trauma might play a role in some cases.
What are the established risk factors for rhabdomyosarcoma?
Known risks include genetic predisposition, certain environmental exposures, and birth defects. Knowing these risks helps identify who might be at higher risk.
How does inflammation contribute to cancer development after trauma?
Inflammation is key in the body’s trauma response. Chronic inflammation can damage DNA and raise cancer risk. It creates a tumor-friendly environment by releasing inflammatory mediators.
What is the difference between acute and chronic inflammation in the context of cancer development?
Acute inflammation is a short-term injury or infection response. Chronic inflammation lasts longer and is linked to cancer. It causes ongoing DNA damage and tissue changes.
Can psychological trauma contribute to cancer development?
Studies in psychoneuroimmunology show psychological trauma can harm immune function. This might affect cancer development. Stress hormones from trauma can weaken the body’s fight against cancer cells.
How is rhabdomyosarcoma diagnosed, and what are the challenges in distinguishing it from trauma effects?
Diagnosing rhabdomyosarcoma uses imaging, biopsy, and histopathology. Telling early RMS from trauma effects is hard. This is why a detailed medical history and thorough diagnosis are key.
What are the treatment options for rhabdomyosarcoma, and what are the survival rates?
Treatments include surgery, chemotherapy, and radiation. Survival rates depend on age, tumor location, and stage. Children have a 70% to 80% chance of survival.
Are there any medicolegal considerations in cases where cancer is discovered after trauma?
Cases involving trauma and cancer might need legal reviews and expert opinions. Compensation and insurance issues can be complex.
What is the current understanding of the relationship between trauma and rhabdomyosarcoma?
There’s no direct link between trauma and rhabdomyosarcoma. Yet, trauma might increase cancer risk in some cases. More research is needed to understand this link.
What are the proposed pathways from injury to malignancy in trauma-induced tumors?
Proposed pathways include chronic inflammation, DNA damage, and genetic mutations from injury. These can lead to tumor growth.
How do developmental factors influence the incidence of rhabdomyosarcoma in children?
Developmental changes, like gene expression and cellular differentiation, affect rhabdomyosarcoma in kids. This makes it more common in certain age groups.
References:
- Wen, Y., et al. (2022). Chronic inflammation, cancer development and its therapeutic targeting. Frontiers in Pharmacology, 13, 1040163.https://www.frontiersin.org/articles/10.3389/fphar.2022.1040163/full





