Last Updated on December 2, 2025 by Bilal Hasdemir
Every year, millions in the U.S. face life-threatening injuries needing quick medical help. In these urgent times, a trauma care specialist can be the key to saving lives trauma surgeon.
A trauma surgeon is a medical expert ready to handle severe injuries. They focus on emergency surgery for patients with critical injuries. Their fast decisions can greatly affect a patient’s recovery.
The job of a trauma surgeon is both tough and fulfilling. It demands surgical talent, quick thinking, and a caring heart.
Key Takeaways
- A trauma surgeon is a medical specialist who treats life-threatening injuries.
- Trauma surgeons provide emergency surgical care to critically injured patients.
- The role of a trauma surgeon is critical in emergency medical situations.
- Trauma surgeons must make swift decisions that impact patient outcomes.
- The work of a trauma surgeon requires a blend of surgical skill and compassion.
Defining the Trauma Surgeon Role
The role of a trauma surgeon is complex. They do more than just surgery. They also lead in trauma care. Trauma surgeons give expert care for acute injuries and work with other teams for full treatment.
Core Functions and Responsibilities
Trauma surgeons check and fix patients with severe injuries. They do emergency surgeries and care for patients after surgery. They also work with other doctors to improve patient care. Their main tasks are:
- Checking injury severity and choosing the right treatment
- Doing surgeries to fix damaged parts
- Working with other doctors to plan treatments
As part of the surgical trauma team, trauma surgeons are key in emergencies. They need to make quick decisions and handle stress well.
Difference Between Trauma Surgeons and Other Specialists
Trauma surgeons are different from other surgeons because they focus on acute injuries. They handle injuries from accidents and violence. Unlike general surgeons, trauma surgeons deal with a wide range of injuries.
Specialist | Primary Focus | Key Responsibilities |
Trauma Surgeon | Acute injury management | Emergency surgery, trauma care protocols |
General Surgeon | General surgical procedures | Elective surgeries, general patient care |
Critical Care Physician | Critical care management | Post-operative care, life support management |
A study on trauma care says, “The trauma surgeon’s role is key in first checking and treating injured patients. They need special skills and judgment”
(This quote shows how important trauma surgeons are in patient care.).
In short, trauma surgeons have many duties. They need skills in surgery, leadership, and teamwork with other doctors.
The Evolution of Trauma Surgery as a Specialty
The field of trauma surgery has grown a lot over time. It has changed because of new discoveries and better ways to treat injuries. This change is because doctors needed to find ways to help patients faster and more effectively.
Historical Development of Trauma Care
At first, doctors who were not trauma experts treated injured people. But, during World War II, things started to change. New surgery methods and organized care systems were set up.
- Development of specialized trauma centers
- Advancements in surgical techniques, such as damage control surgery
- Improvements in critical care practices
Modern Advancements in the Field
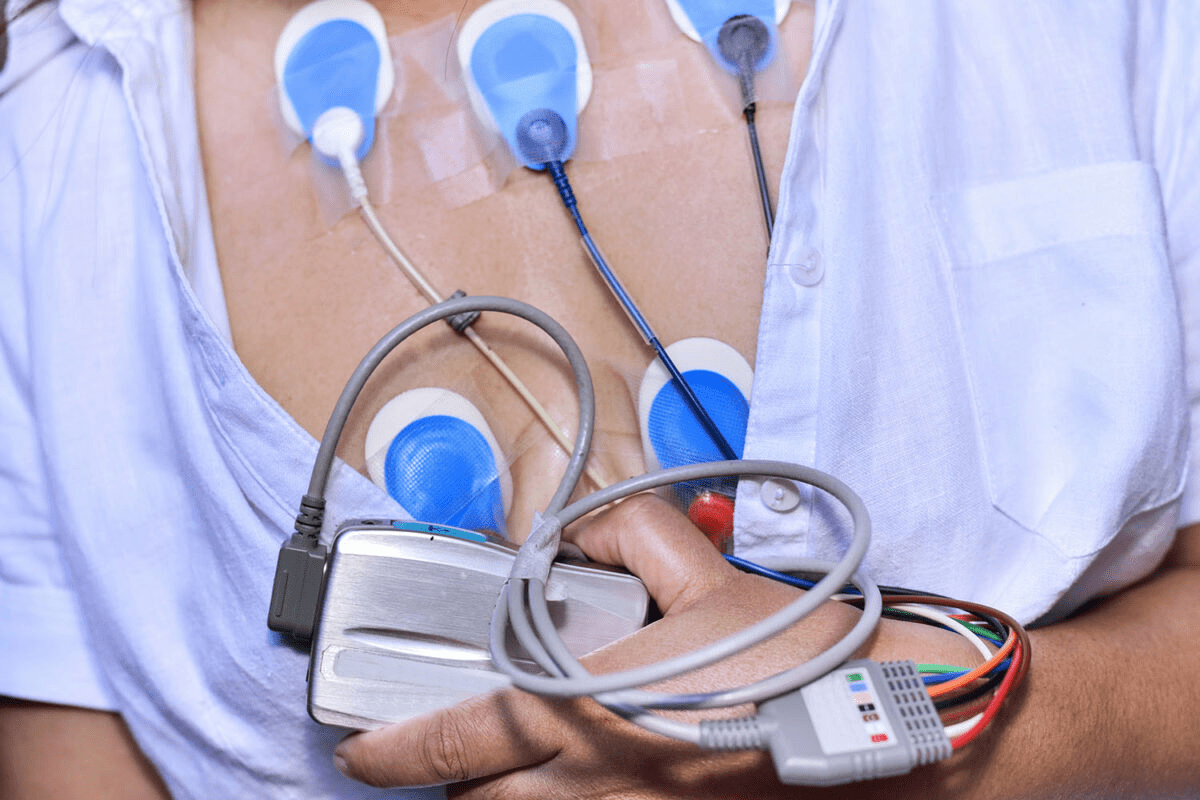
Today, trauma surgery keeps getting better thanks to new technology and techniques. Doctors use minimally invasive approaches and technological innovations like telemedicine and advanced imaging. These help patients get better faster.
- Enhanced imaging capabilities
- Improved surgical instrumentation
- Better critical care management protocols
These changes have made trauma surgery a more important field. Now, trauma surgeons can give better care to those who are very sick or hurt.
Education and Training Path for Trauma Surgeons
The path to becoming a trauma surgeon is long and challenging. It involves many stages of hard work and learning. It takes a lot of time, effort, and dedication.
Undergraduate and Medical School Requirements
The journey starts with a strong background in sciences like biology, chemistry, or physics. Then, aspiring trauma surgeons must finish four years of medical school. They earn a Doctor of Medicine (M.D.) or Doctor of Osteopathic Medicine (D.O.) degree.
During medical school, students learn a lot about medicine. They get a broad understanding of medical principles and practices.
Surgical Residency Training
After medical school, the next step is a surgical residency program. This can last from five to seven years. Residents learn surgical techniques and patient care under experienced surgeons.
Trauma and Critical Care Fellowship
After the residency, aspiring trauma surgeons do a trauma and critical care fellowship. This training lasts one to two years. It focuses on managing critically ill patients and trauma surgery.
This fellowship gives the needed skills for trauma environments. Trauma surgeons also need strong critical thinking, leadership, and communication skills. These are key for working well with others and making quick, accurate decisions.
Understanding the long education and training path shows the commitment needed to be a trauma surgeon. The high standards and specialized training prepare them for critical care situations.
Essential Skills and Qualities of a Trauma Surgeon
To succeed, trauma surgeons need technical skills, critical thinking, and leadership. This field is complex and demanding. It requires a special mix of abilities to handle various injuries and conditions.
Technical Surgical Abilities
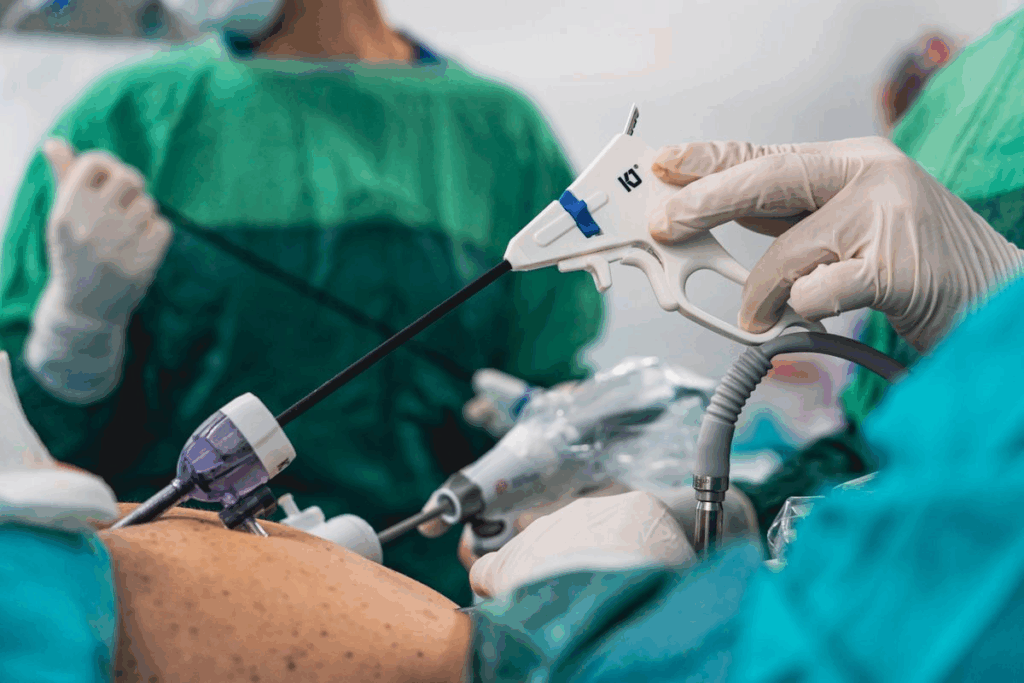
Trauma surgeons must be skilled in advanced surgical techniques. They need to know how to do damage control surgery and use minimally invasive methods. Their skills are key to making fast decisions and working well under pressure.
Critical Thinking Under Pressure
Critical thinking is essential for trauma surgeons. They work in high-stress situations where quick decisions are needed. Being able to assess situations, prioritize, and make sound judgments is vital for good trauma care.
Leadership and Communication Skills
Leadership and communication are critical for trauma surgeons. They must lead the trauma team well, communicate clearly with others, and care for patients and their families with compassion.
Skill | Description | Importance in Trauma Surgery |
Technical Surgical Abilities | Proficiency in surgical techniques and decision-making. | High |
Critical Thinking | Ability to assess situations and make sound judgments under pressure. | High |
Leadership and Communication | Ability to lead teams and communicate effectively. | High |
A Day in the Life of a Trauma Surgeon
A trauma surgeon’s day is packed with tasks. They handle administrative duties, hospital rounds, and emergency responses. Their job demands precision and quick decision-making.
Hospital Rounds and Administrative Duties
The day starts early for a trauma surgeon. They check on patients who have had surgery or are being treated for injuries. They review patient progress, update treatment plans, and talk with other doctors.
They also do administrative work like looking over patient charts and updating records. This is a big part of their day.
Emergency Response Protocols
Trauma surgeons must be ready to act fast in emergencies. When a trauma patient comes in, they quickly figure out what to do. They work with the team to keep the patient stable.
This job needs effective communication and rapid decision-making.
On-Call Responsibilities and Challenges
Being on call is a big part of their job. They must be ready to respond to emergencies anytime. This can be tough, both physically and emotionally.
Their schedule can be unpredictable, with long hours and little sleep. It’s a demanding job.
Duty | Description | Frequency |
Hospital Rounds | Checking on patients, assessing progress, and planning treatment | Daily |
Emergency Response | Responding to trauma emergencies, prioritizing treatment, and coordinating care | As needed |
Administrative Duties | Reviewing patient charts, updating records, and other administrative tasks | Daily |
Being a trauma surgeon is both tough and rewarding. It requires medical skills, leadership, and the ability to work well under pressure. Their work is vital to a trauma center, making a big difference in patients’ lives.
Types of Trauma Cases and Injuries Treated
Surgical treatment for trauma covers many injuries. This includes blunt force trauma and multi-system trauma. Trauma surgeons are ready for all kinds of cases, from simple to complex.
Blunt Force Trauma Management
Blunt force trauma happens when a force hits the body but doesn’t go through it. It can cause a lot of internal damage. This injury is common in car accidents, falls, and sports.
Doctors use imaging like CT scans to see the damage. Then, they decide if surgery is needed.
Common injuries from blunt force trauma include:
- Spleen injuries
- Liver lacerations
- Fractures of major bones
Penetrating Injury Treatment
Penetrating injuries, like gunshot wounds or stabbings, need quick action. They can cause a lot of internal damage. Doctors first stabilize the patient and then fix the damage surgically.
Type of Injury | Common Complications | Treatment Approach |
Gunshot Wounds | Bleeding, Organ Damage | Surgical exploration, Damage control |
Stabbing Injuries | Infection, Internal Bleeding | Wound exploration, Repair of damaged structures |
Multi-System Trauma Approach
Multi-system trauma affects many body systems or organs. Handling these cases needs a team effort from different medical fields. The trauma team checks the patient, sorts injuries by severity, and plans a detailed treatment.
Success comes from teamwork. This includes surgeons, intensivists, nurses, and more.
Understanding Trauma Centers and Their Classification
Trauma centers are key in healthcare, sorted by their treatment resources. The level of care they offer ranges from Level I, the highest, to Level V, for initial care before transfer. This classification helps ensure patients get the right care.
Level I Trauma Centers: Capabilities and Requirements
Level I trauma centers handle the most severe cases. They have 24/7 trauma surgeons and a wide range of specialists. These centers must meet specific case volume and research requirements.
Their staffing for trauma surgeons is strict. This ensures patients get top-notch care.
Level II-V Trauma Centers: Differences and Limitations
Level II centers offer 24/7 care but have less specialty coverage than Level I. Level III centers stabilize patients before transfer. Levels IV and V provide basic care.
Knowing these differences is key for effective trauma care.
Trauma Surgeon Staffing Standards
Staffing for trauma surgeons varies by center level. Level I centers need trauma surgeons available at all times. Lower levels have different needs based on their capabilities and case volume.
In summary, trauma center classification is vital for patient care. It determines the resources available for treatment. Understanding these classifications and staffing standards is essential for optimal care.
The Trauma Team: Collaborative Emergency Response
Trauma teams are key in emergency care, acting fast and accurately in urgent cases. Their success comes from who they are and how well they work together.
Key Team Members and Their Roles
The trauma team has many healthcare experts. Important roles include:
- Trauma surgeons: They do surgeries and lead the team.
- Emergency medicine physicians: They first check and stabilize patients.
- Nurses: They are critical care, operating room, and nurse practitioners. They are essential in patient care.
- Anesthesiologists: They handle airways and give anesthesia.
- Radiologists: They do and read imaging studies.
Effective communication among these members is key for the best patient results.
Communication and Coordination Protocols
Having clear communication rules is vital for the team’s success. These include:
Protocol | Description | Benefits |
SBAR (Situation, Background, Assessment, Recommendation) | A structured way to share important info. | Makes things clearer and cuts down on mistakes. |
Closed-loop communication | Makes sure info is confirmed and understood. | Prevents misunderstandings and makes sure tasks are done. |
Regular training and simulation exercises help make these rules stick. This ensures the team works well together, even when it’s tough.
Advanced Trauma Surgery Techniques
Advanced trauma surgery techniques have changed how we handle trauma cases. New surgical methods have greatly improved patient care in trauma situations.
Damage Control Surgery Principles
Damage control surgery is key for severely injured patients. It quickly stops bleeding and contamination. Then, it focuses on resuscitation and final repairs. The main goal is to keep the patient stable and avoid more problems.
Key principles of damage control surgery include:
- Rapid assessment and control of life-threatening injuries
- Temporary closure of wounds to prevent infection
- Resuscitation in the intensive care unit (ICU) before definitive surgery
Minimally Invasive Approaches in Trauma
Minimally invasive surgery (MIS) is vital in trauma care. It cuts down recovery time and reduces pain after surgery. Laparoscopy and thoracoscopy allow for treating injuries with smaller cuts.
The table below shows the benefits of minimally invasive approaches in trauma surgery:
Technique | Benefits |
Laparoscopy | Reduced risk of infection, less postoperative pain |
Thoracoscopy | Less invasive, quicker recovery |
Technological Innovations in Trauma Care
Technological advancements have greatly influenced trauma surgery. Innovations like 3D printing, robotics, and advanced imaging have improved diagnosis and surgery precision.
The future of trauma surgery is bright. Ongoing research and development aim to improve patient care and outcomes even more.
What Does a Trauma Surgeon Do Beyond the Operating Room?
Trauma surgeons do much more than just operate. They play a vital role in patient care, going beyond the operating room. Their duties are wide-ranging and critical for patient recovery and well-being.
Critical Care Management
One of their main jobs is critical care management. After surgery, patients need close monitoring in the ICU. Trauma surgeons work with other healthcare teams to manage these patients’ complex needs. They make important decisions that can greatly affect patient outcomes.
Follow-up Care and Rehabilitation Coordination
After the ICU, trauma surgeons focus on follow-up care and rehabilitation coordination. They work with rehab specialists to create plans for patients to regain strength and mobility. This teamwork is key to ensuring patients get the full care and support they need during recovery.
The role of a trauma surgeon is complex and challenging. They handle everything from critical care to follow-up care. Their work requires surgical skill, critical thinking, and compassion.
Trauma Surgeon Subspecialties and Focus Areas
The field of trauma surgery has many subspecialties. These focus on different types of trauma and patient groups. This allows surgeons to use their skills and interests to improve care.
Pediatric Trauma Surgery
Pediatric trauma surgery is key for treating injured kids. Pediatric trauma surgeons need special training to handle children’s unique needs. They use specific equipment and techniques.
Military and Disaster Response Trauma
Military and disaster response trauma surgery deals with injuries from war or disasters. Trauma surgeons in this field face tough environments. They must make fast decisions under pressure.
Surgical Critical Care
Surgical critical care focuses on very sick or injured patients. Surgical critical care specialists work with a team to give detailed care. This includes life-saving treatments and constant monitoring.
These areas show the wide range and depth of trauma surgery. They give surgeons a chance to specialize and greatly help patients.
Career Outlook and Compensation for Trauma Surgeons
Trauma surgeons are in high demand in many places. Their career prospects depend on population density and the number of trauma cases. The job outlook for these experts is influenced by trends in the job market and where they can work.
Job Market Trends and Demand
The need for trauma surgeons is growing. This is because more people are getting hurt in accidents and violence. Several factors are driving this demand:
- Population growth and urbanization
- Changes in healthcare policies and infrastructure
- Advancements in medical technology and trauma care
These trends suggest a bright job market for trauma surgeons. They offer chances for growth and to specialize in their field.
Geographic Variations in Employment Opportunities
The availability of jobs for trauma surgeons varies by location. Cities and areas with more trauma cases need more of these specialists. Important factors to consider are:
- Regional Trauma Incidence: Places with more trauma (like cities) need more trauma surgeons.
- Healthcare Infrastructure: The number of trauma centers and healthcare facilities affects the demand for trauma surgeons.
It’s important for those thinking about becoming trauma surgeons to understand these factors. They directly affect job availability and pay.
Challenges and Stressors in Trauma Surgery Practice
Trauma surgeons work in a very stressful environment. They have to make quick decisions and can’t afford to make mistakes. Their job is filled with challenges that can affect their health and how well they do their job.
Emotional and Psychological Impact
The job of trauma surgeons is very emotionally demanding. They deal with life-or-death situations and traumatic cases. This can lead to compassion fatigue, where they find it hard to connect with their patients.
One surgeon said, “The hardest part is not the surgery itself, but the emotional burden of dealing with traumatic cases every day.”
“You can’t help but take the cases home with you,” said a renowned trauma surgeon. “It’s not just about saving lives; it’s about the families, the loved ones, and the impact on the community.”
Burnout Prevention and Wellness Strategies
To fight burnout, trauma surgeons are trying different wellness strategies. They practice mindfulness, exercise regularly, and seek help from colleagues and mental health experts.
Wellness Strategy | Description | Benefits |
Mindfulness Practices | Meditation and deep breathing exercises | Reduces stress, improves focus |
Regular Exercise | Physical activity to improve health | Enhances mood, reduces burnout |
Peer Support | Sharing experiences with colleagues | Fosters camaraderie, reduces feelings of isolation |
Ethical Dilemmas in Trauma Care
Trauma surgeons face tough ethical decisions. These include organ donation, end-of-life care, and how to use limited resources. They need a strong sense of ethics and a deep understanding of medical ethics.
By understanding the challenges of trauma surgery, we can better support these critical care providers. It’s important to find ways to prevent burnout and handle ethical dilemmas. This will help keep our trauma care system strong and effective.
The Future of Trauma Surgery
Trauma surgery is on the verge of a new era. This is thanks to new technologies and research. The field is rapidly evolving, with significant advancements in patient treatment.
Emerging Technologies and Treatment Approaches
Robotics and artificial intelligence are making trauma surgery more precise. This leads to better results for patients. Minimally invasive surgery is also growing, cutting down on recovery times and complications.
- Advanced imaging technologies for better diagnosis
- Personalized medicine approaches tailored to individual patient needs
- Innovative biomaterials for wound healing and tissue repair
Evolution of Training Methodologies
Training for trauma surgeons is changing too. Simulation-based training and virtual reality are now key parts of learning. These tools help surgeons get better at their job and make quicker decisions.
Research Frontiers in Trauma Care
Research in trauma care is all about translational research. It’s about moving scientific discoveries from the lab to the hospital. The focus is on better ways to stop bleeding, handle brain injuries, and help patients recover.
Conclusion
Trauma surgeons are key in healthcare, helping patients with severe injuries. They need special skills in surgery, thinking, and leadership.
We’ve looked at what trauma surgeons do, from their education to the challenges they face. We’ve also talked about the types of injuries they treat and the role of trauma centers.
In short, trauma surgeons are vital to healthcare. Their work greatly improves patient outcomes. As trauma surgery grows, we must value these doctors and their lifesaving work.
FAQ
What is a trauma surgeon?
A trauma surgeon is a medical expert who treats severe injuries. They work in trauma centers with a team to provide emergency care.
What kind of training does a trauma surgeon need?
Trauma surgeons get a lot of education and training. They finish medical school, a surgical residency, and sometimes a trauma fellowship. This prepares them for complex injuries.
What are the primary responsibilities of a trauma surgeon?
Their main jobs are to assess and stabilize patients with severe injuries. They perform emergency surgeries and work with other healthcare teams. They also manage critical care and rehabilitation.
How do trauma surgeons differ from other surgeons?
Trauma surgeons specialize in acute injuries and make quick decisions in emergencies. Unlike other surgeons, they focus on emergency cases, not elective procedures.
What are the different levels of trauma centers?
Trauma centers have levels (I-V) based on their resources. Level I centers handle the most complex injuries. Lower levels have less capability.
What is damage control surgery?
Damage control surgery is a method used in trauma care. It focuses on stabilizing the patient first, then does more repairs later.
How do trauma surgeons manage blunt force trauma?
They assess injuries and use imaging studies. Then, they treat with surgery for internal bleeding or organ damage.
What role do trauma surgeons play in critical care?
Trauma surgeons manage critically ill patients with severe injuries. They coordinate care and decide on further interventions.
Are there subspecialties within trauma surgery?
Yes, there are subspecialties like pediatric trauma surgery and military trauma. These need specialized knowledge and skills.
What is the job outlook for trauma surgeons?
The job outlook is positive due to the need for emergency care. It can vary by location and other factors.
How do trauma surgeons cope with the stress of their job?
They face a lot of stress. To cope, they balance work and life, seek support, and do wellness activities.
What emerging technologies are impacting trauma surgery?
New technologies like advanced imaging and robotics are improving trauma care. They make treatments more precise and effective.
References
National Center for Biotechnology Information. Evidence-Based Medical Insight. Retrieved from https://pubmed.ncbi.nlm.nih.gov/21292320/)