Last Updated on October 21, 2025 by mcelik
Blood disorders, or hematologic diseases, affect the health of blood cells. They can happen to anyone, at any age. These conditions often need special care.
Hematologic diseases include many conditions. They affect red blood cells, white blood cells, and platelets. They also include bleeding disorders. The type of blood cell affected and the disorder’s nature determine the classification.
| Type of Disorder | Description | Examples |
| Red Blood Cell Disorders | Affect the production or function of red blood cells | Anemia, Polycythemia |
| White Blood Cell Disorders | Impact the immune system, affecting the body’s ability to fight infection | Leukemia, Lymphoma |
| Platelet Disorders | Affect the blood’s ability to clot | Thrombocytopenia, Thrombocytosis |
Hematologic diseases can be caused by genetics, environment, or both. Risk factors include family history, exposure to toxins, and infections.
Knowing these risk factors helps in early detection and prevention.
The symptoms of hematologic diseases vary. Common signs include fatigue, weakness, frequent infections, and easy bleeding or bruising.
“Early recognition of the signs and symptoms of blood disorders can significantly impact the effectiveness of treatment and patient outcomes.”
Seeing these symptoms early and getting medical help is key. It ensures proper diagnosis and treatment.
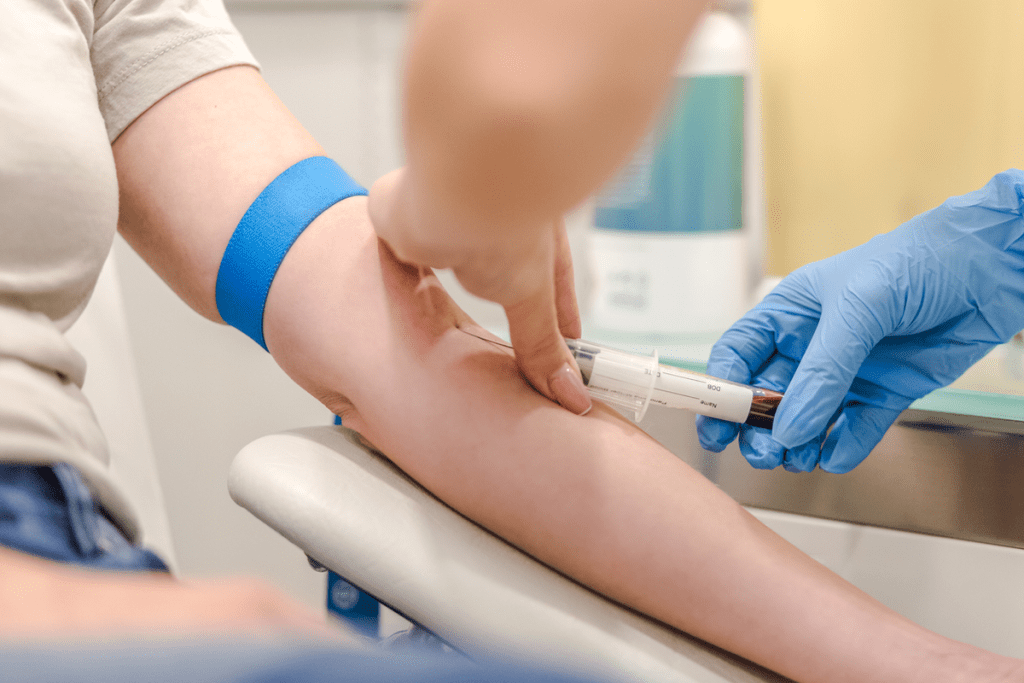
Diagnosing blood disorders requires a mix of clinical checks and advanced tests. We’ll walk you through how doctors diagnose blood disorders step by step.
The first step in diagnosing a blood disorder is a detailed initial assessment. Medical history is key, as it reveals symptoms, past illnesses, and family health that might be linked to the disorder.
During the physical examination, doctors look for signs like pale skin, jaundice, or big lymph nodes. These signs can hint at a blood disorder.
For a deeper diagnosis, advanced diagnostic techniques are used. These include bone marrow biopsies, genetic tests, and imaging studies.
Bone marrow biopsy is crucial for diagnosing leukemia or lymphoma. It lets doctors check the bone marrow’s cells up close.
We set clear goals and outcomes when planning treatment. “The main goal is to manage the disease well, improve the patient’s life, and avoid complications,” says our hematology expert. We look at the patient’s health, the blood disorder’s specifics, and the best treatments.
We assess the patient’s condition thoroughly. This includes test results and medical history. This helps us create a personalized treatment plan. The plan might include medicines, lifestyle changes, and support care.
Managing blood diseases often needs a team effort. Our team includes experts in hematology, oncology, and more. We work together to support patients fully during their treatment.
Together, we meet the complex needs of blood disorder patients. We provide holistic care. This includes medical treatment, emotional, and psychological support.
Personalized medicine is key in managing blood disorders. It lets us tailor treatments to each patient’s needs. We use genetic testing and molecular diagnostics to find the best treatments and avoid side effects.
We keep improving our care based on new research and evidence. Our aim is to give patients the best results and improve their life quality.
“The future of hematology lies in our ability to personalize treatment plans and adapt to the unique needs of each patient,” notes a leading expert in the field.
By adopting this approach, we can significantly help patients with blood disorders. We offer them hope and support as they go through their treatment.
Managing blood diseases often requires specific treatments. These treatments have changed how we treat blood diseases. They help patients live better lives.
Anticoagulants and antiplatelet drugs prevent blood clots. Anticoagulants like warfarin and NOACs stop the clotting process. Antiplatelet drugs, such as aspirin, stop platelets from sticking together.
These drugs are used for deep vein thrombosis, pulmonary embolism, and more. The right choice depends on the condition and the patient’s risk.
| Medication Class | Examples | Primary Use |
| Anticoagulants | Warfarin, Rivaroxaban | Preventing DVT, PE |
| Antiplatelet Agents | Aspirin, Clopidogrel | Preventing arterial thrombosis |
Growth factors help make more blood cells. They treat anemia and neutropenia. Erythropoietin-stimulating agents help make red blood cells, reducing the need for transfusions.
Granulocyte-colony stimulating factor (G-CSF) boosts neutrophil production. This lowers infection risk in chemotherapy patients. These treatments greatly improve patient outcomes.
Immunosuppressive therapies treat blood disorders caused by an overactive immune system. These include corticosteroids and other drugs. They are key in managing aplastic anemia and certain hemolytic anemias.
These therapies reduce blood cell destruction and improve bone marrow. But, they must be monitored for side effects and infection risks.
Targeted molecular therapies are a big step forward in treating blood cancers. They target specific disease drivers. Tyrosine kinase inhibitors and monoclonal antibodies are examples.
These therapies improve outcomes and reduce chemotherapy side effects. They are often used with other treatments to boost effectiveness.
Red blood cell disorders affect how red blood cells are made, work, and last. At our center, we use the newest in hematology to help patients. We make care plans that fit each person’s needs.
Anemia means not enough red blood cells or poor quality ones. This makes it hard for tissues to get oxygen. Treatment depends on why it happens, like iron or vitamin lack, chronic disease, or bone marrow issues.
For iron lack, doctors often give iron supplements. This helps make more red blood cells. If anemia comes from chronic disease, treating that disease is key.
Polycythemia and erythrocytosis mean too many red blood cells. This can lead to blood clots and other problems. Our goal is to lower red blood cell count to reduce risks.
Phlebotomy, or regular blood removal, is a common treatment. Sometimes, drugs are used to slow down red blood cell making.
Sickle cell disease changes hemoglobin, making red blood cells sickle-shaped and short-lived. We manage it with a team effort, focusing on pain, infections, and watching for serious problems.
Our treatments include hydroxyurea for fewer pain episodes, blood transfusions for better oxygen, and support for related issues.
With a treatment plan made just for them, we help patients with red blood cell disorders live better lives.

Medical science has made big strides in treating white blood cell disorders. These cells are key to our immune system. Problems with them can cause serious health issues. We’ll look at how to treat leukemia, manage neutropenia, and tackle lymphoproliferative disorders.
Leukemia is a blood and bone marrow cancer that needs quick and effective treatment. The main treatments are chemotherapy, targeted therapy, and stem cell transplantation. Chemotherapy uses drugs to kill cancer cells. Targeted therapy targets specific molecules that help cancer grow.
The right treatment depends on the leukemia type, the patient’s health, and other factors. For example, acute lymphoblastic leukemia (ALL) often gets intensive chemotherapy. Chronic myeloid leukemia (CML) might be treated with targeted therapy using tyrosine kinase inhibitors.
Neutropenia means having too few neutrophils, making infections more likely. To manage it, we use granulocyte-colony stimulating factor (GCSF) to boost neutrophil production. We also follow strict infection control, like washing hands often and staying away from sick people.
Lymphoproliferative disorders involve abnormal lymphocyte growth. They can be benign or cancerous. Treatment varies based on the disorder and its severity. Some may just need watching, while others need chemotherapy, radiation, or immunotherapy right away.
Immunotherapy uses the immune system to fight cancer. It’s showing promise in treating some lymphoproliferative disorders. For example, monoclonal antibodies target specific cancer cells in some lymphomas.
Disorders affecting platelets and blood clotting are big challenges for patients and doctors. To manage these conditions well, we need to understand their causes, symptoms, and treatment options.
Thrombocytopenia means having too few platelets. It can happen for many reasons, like bone marrow problems, certain medicines, or autoimmune diseases. Treatment aims to fix the root cause and may include:
Platelet transfusions help in severe cases or when there’s bleeding. Drugs like romiplostim and eltrombopag help make more platelets.
Thrombocytosis means having too many platelets. It can be primary (from a blood disorder) or secondary (due to another reason). Treatment focuses on the cause and may include:
For primary thrombocytosis, hydroxyurea is used to lower platelet counts and prevent blood clots.
Hemophilia A and B are genetic disorders. They lack clotting factors VIII and IX. Treatment involves replacing these factors to help blood clot.
Factor VIII and factor IX concentrates treat bleeding and prevent future issues. Regular treatment helps keep joints healthy.
Von Willebrand disease (VWD) is the most common bleeding disorder. It’s caused by a lack or problem with von Willebrand factor (VWF). Treatment includes:
Desmopressin is first used for mild VWD. VWF concentrates are for more severe cases or when desmopressin doesn’t work.
For many patients with blood diseases, stem cell transplantation is a hopeful treatment. This complex process replaces a patient’s sick or damaged stem cells with healthy ones. These can come from the patient themselves or a donor.
The choice between autologous and allogeneic transplantation depends on several factors. These include the type of blood disease, the patient’s health, and donor availability. Autologous transplantation uses the patient’s own stem cells, collected, stored, and then reinfused after chemotherapy. This method lowers the risk of GVHD but might increase the chance of disease relapse.
Allogeneic transplantation uses stem cells from a donor. It can offer a graft-versus-tumor effect, lowering relapse risk. But, it also risks GVHD. Choosing the right donor is crucial, with HLA matching being key to avoid complications.
Choosing patients for stem cell transplantation is a detailed process. It includes looking at their medical history, current health, and disease specifics. Preparation for transplantation involves chemotherapy and/or radiation to clear out diseased cells and weaken the immune system.
After stem cell transplantation, patients need careful monitoring for complications. Post-transplant care includes regular check-ups, lab tests, and imaging to check blood counts and overall health.
Advanced cellular therapies are also being used to treat blood diseases. CAR T-cell therapy genetically modifies T cells to attack cancer cells. It has shown great promise in treating some leukemias and lymphomas.
As research advances, new and innovative therapies are emerging. These treatments are part of a shift towards personalized medicine. They are tailored to meet each patient’s unique needs.
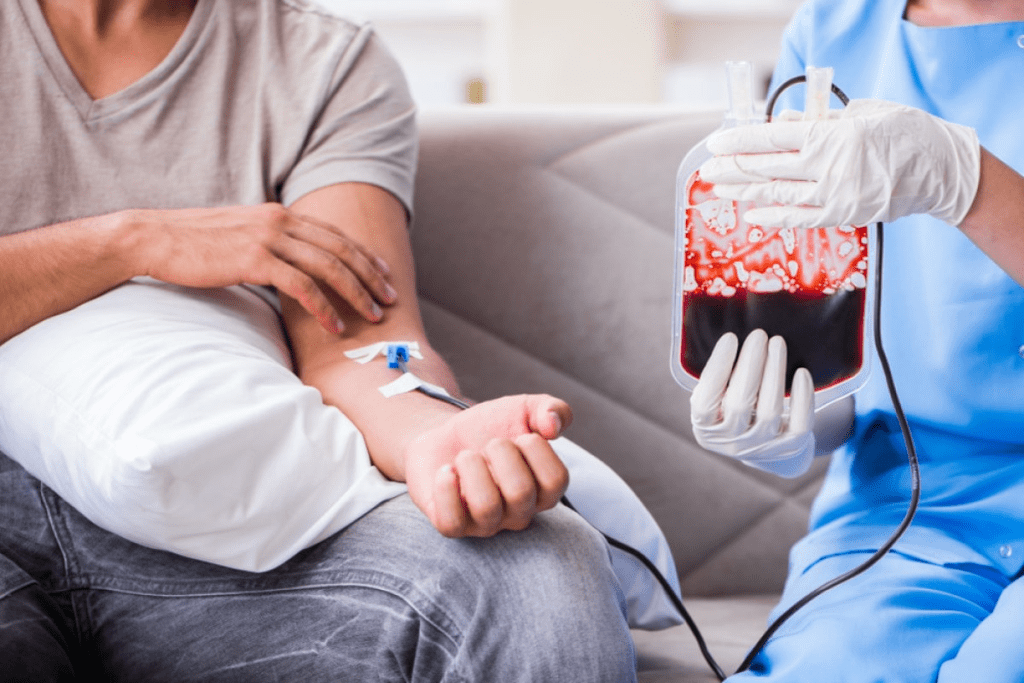
Blood transfusion therapy is key in managing hematologic diseases. It involves giving blood or blood parts to replace or add to the patient’s blood cells or clotting factors. We will look at the different parts of blood transfusion therapy. This includes the types of blood products used, when to give them, how to give them, and handling reactions and complications.
Blood transfusion therapy uses different blood products for various needs. These include:
Deciding to give a blood transfusion is based on clinical judgment and lab results. Common reasons include:
Guidelines stress the importance of proper patient identification, compatibility testing, and monitoring during and after transfusion.
| Blood Component | Indication | Administration Guideline |
| Red Blood Cells | Anemia, Blood Loss | Transfuse to improve oxygen delivery |
| Platelets | Thrombocytopenia, Platelet Dysfunction | Transfuse to prevent or treat bleeding |
| Fresh Frozen Plasma | Clotting Factor Deficiency | Transfuse to correct coagulopathy |
While blood transfusion therapy is safe, there are risks and complications. These include:
Quick recognition and management of these reactions are key to patient safety.
Research is ongoing for alternatives to traditional blood transfusion. These include:
These alternatives aim to reduce blood transfusion risks and improve patient outcomes.
Pain management is key for patients with hematologic diseases. We use various strategies, like medicine and non-medical methods. Effective pain management boosts comfort and quality of life.
Fatigue is common in patients with hematologic conditions. It affects daily life and quality of life. We tackle fatigue with lifestyle changes and medical help to boost energy.
Nutritional support is crucial for patients with hematologic diseases. Good nutrition helps manage symptoms and supports health. We guide patients on dietary needs to keep them strong and support treatment.
Living with a hematologic disease is tough, physically and emotionally. We offer psychological and emotional support, like counseling and support groups. Access to these resources is key for mental well-being and resilience.
By adding supportive care and symptom management to treatment plans, we improve outcomes for patients with hematologic diseases. Our care is comprehensive and patient-centered. It addresses the complex needs of those with blood disorders.
Hematologic conditions are getting new treatments that change patient outcomes. Medical research has led to new ways to treat blood disorders. These new treatments offer hope to patients.
Immunotherapy uses the immune system to fight diseases. CAR T-cell therapy, a type of immunotherapy, is very effective against some leukemias and lymphomas.
“Immunotherapy represents a paradigm shift in the treatment of hematologic diseases, offering patients a more targeted and potentially less toxic alternative to traditional therapies.”
New targeted agents are being researched in hematology. They aim to target disease-causing mechanisms without harming healthy cells. Several promising therapies are in clinical trials, offering hope for better treatment results.
Precision medicine is changing how we treat blood diseases. It tailors treatment to each patient’s genetic profile and disease. This approach helps doctors choose the best treatment and reduce side effects.
As we learn more about hematologic diseases, new treatments and therapies will be key in improving patient care.
Getting a blood disorder diagnosis is just the beginning. It’s important to learn how to manage it for better health. Managing blood disorders means getting medical care, making lifestyle changes, and getting ongoing support.
Exercise is key for those with blood disorders. It boosts circulation, energy, and health. But, the right exercise depends on the person’s condition and how they feel.
Recommended Activities:
Before starting any new exercise, patients should talk to their doctor. This is especially true for those with conditions like thrombocytopenia or bleeding risks.
Patients with blood disorders, especially those who are immunocompromised, are at a higher risk of infections. It’s important to prevent infections.
Prevention Measures:
Living with a blood disorder can affect daily life and quality of life. Patients may need to adjust their routines to manage their condition well.
Practical Tips:
By making smart lifestyle choices and getting the right support, people with blood disorders can live active and meaningful lives.
Hematologic diseases affect the blood and blood-making parts. They are split into types based on the blood cell affected. This includes red, white, and platelet disorders.
Signs include feeling tired, weak, and pale. You might also have shortness of breath, get sick often, bruise easily, and bleed. Symptoms vary by disorder.
Doctors use physical checks, medical history, and lab tests. These include blood work and bone marrow biopsies. Advanced tests are also used.
Goals depend on the disease. They often include managing symptoms and improving life quality. Sometimes, the aim is to cure or achieve remission.
It’s about tailoring treatment to fit each patient. This is based on their condition, genetics, and other factors.
Treatments include anticoagulants, growth factors, and immunosuppressives. There are also targeted molecular therapies.
Anemia is treated with iron supplements. Sickle cell disease may use hydroxyurea. Blood transfusions are sometimes needed.
Leukemia treatment often includes chemotherapy and targeted therapy. Sometimes, stem cell transplantation is used.
Treatments include platelet transfusions for low counts. For high counts, medications are used. Hemophilia is treated with replacement therapy.
It replaces diseased bone marrow with healthy stem cells. It’s used for diseases like leukemia and lymphoma.
It’s a therapy that genetically modifies T-cells to fight cancer. It’s an advanced cellular therapy.
It helps with anemia and bleeding. But, there are risks like reactions and infectious disease transmission.
Patients can manage symptoms with pain relief, nutrition, and counseling. Exercise and infection prevention also help.
New treatments include gene therapy and immunotherapy. There are also novel agents and precision medicine.
Patients can get advice on exercise, diet, and infection prevention. Stress management is also key.
Supportive care meets physical, emotional, and social needs. It improves well-being and coping ability.
Patients should avoid certain foods and stay hydrated. Adequate nutrition is also important for health.
Subscribe to our e-newsletter to stay informed about the latest innovations in the world of health and exclusive offers!