Last Updated on November 25, 2025 by Ugurkan Demir

Bladder cancer hits tens of thousands of people every year. Many wonder about their prognosis and if they can be cured. The bright side is that bladder cancer is very treatable if caught early. It’s often curable too. What is the tumor in bladder prognosis and is bladder cancer curable? We break down survival rates and the likelihood of a cure by stage.
The American Cancer Society says the 5-year survival rate for bladder cancer depends on when it’s found. For those diagnosed between 2014 and 2020, the survival rate is 97% for in situ alone. It’s 72% for localized, 40% for regional, and 9% for distant stages. This shows how key early detection is.
At Liv Hospital, we use international expertise and evidence-based care for bladder cancer patients. We mix preventive strategies with the latest treatments.
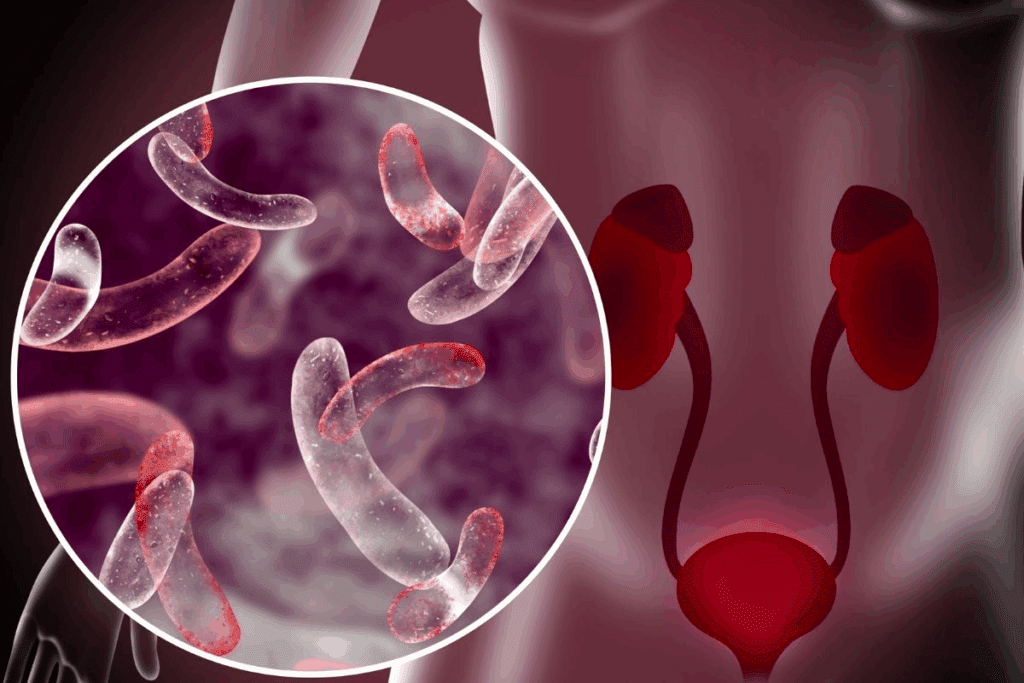
Knowing how bladder cancer is classified and staged is key to understanding treatment options. Bladder cancer is divided based on the type of cells affected and how far it has spread.
There are several types of bladder cancer, each starting in different cells. The most common is urothelial carcinoma, making up about 90% of cases. Less common but aggressive types include squamous cell carcinoma and adenocarcinoma.
The American Cancer Society says knowing the type of bladder cancer is vital. It helps doctors decide the best treatment. For example, urothelial carcinoma can be split into subtypes based on its look and genetics.
The TNM staging system is a way to measure how far cancer has spread. It’s used by the American Joint Committee on Cancer (AJCC) and the Union for International Cancer Control (UICC). It looks at three main parts:
The TNM system gives a detailed look at how far cancer has spread. This is important for planning treatment. For example, T1N0M0 means the tumor is in the bladder wall, no lymph nodes are involved, and there’s no distant spread.
| TNM Component | Description | Prognostic Implication |
| T1 | Tumor limited to the bladder wall | Favorable prognosis with appropriate treatment |
| N0 | No lymph node involvement | Generally associated with better outcomes |
| M0 | No distant metastasis | Localized disease, potentially curable |
Cancer experts say the TNM staging system is key for doctors to plan treatments. Knowing the TNM stage helps patients understand their prognosis and the treatment plan.
“The accurate staging of bladder cancer using the TNM system is critical for determining the most appropriate treatment approach and improving patient outcomes.”
— Medical Expert, Urologist

Knowing the survival stats for bladder cancer is key for both patients and doctors. These numbers show how likely someone is to live for five years after being diagnosed.
The 5-year survival rate for bladder cancer is about 77-78 percent. This means 77-78 percent of people with bladder cancer might live for five years after diagnosis, compared to others.
The 5-year survival rate is a common way to predict cancer outcomes. For bladder cancer, this rate changes a lot based on the cancer’s stage. In England, the 5-year survival rate for bladder cancer is around 50% for all stages, says Cancer Research UK.
Let’s look at survival rates by stage:
| Stage at Diagnosis | 5-Year Relative Survival Rate |
| Localized | 70-71% |
| Regional Spread | 39% |
| Metastatic Disease | 8% |
Survival rates come from cancer registries that track patient outcomes. The 5-year relative survival rate compares cancer patients to the general population, adjusting for age and other factors.
It’s important to remember that survival rates are just estimates. They can change based on many things, like overall health, treatment response, and cancer specifics.
Bladder cancer survival rates can be compared to other urological cancers. For example, prostate cancer has a higher 5-year survival rate. Kidney cancer’s rate is somewhat similar to bladder cancer’s.
By knowing these stats and how they compare, patients and doctors can make better treatment and care choices.
Knowing the prognosis for bladder cancer is key for both patients and doctors. It changes a lot based on the stage found at diagnosis. The American Cancer Society gives insights into survival rates based on the SEER stage. This info helps in understanding the prognosis and making treatment choices.
Carcinoma in situ (CIS) is an early stage of bladder cancer. The cancer cells are only in the bladder lining. The American Cancer Society says CIS has a 5-year survival rate of 96-97%.
This high survival rate is because CIS is treated well with intravesical therapy or surgery.
“The high survival rate for CIS shows how well current treatments work,” says Dr. [Last Name], a leading urologist. “Patients diagnosed at this stage have a good chance of recovery.”
Localized bladder cancer means the cancer hasn’t spread beyond the bladder. The 5-year survival rate for this stage is 70-71%. Treatment options include surgery, chemotherapy, and radiation therapy, often used together.
The American Cancer Society notes that survival rates for localized bladder cancer are much higher than for more advanced stages. This shows how important early detection and treatment are.
When bladder cancer spreads to nearby tissues or lymph nodes, it’s called regional. The 5-year survival rate for regional bladder cancer is 39%. Treatment at this stage often includes radical cystectomy and chemotherapy.
The survival rate drops significantly for regional bladder cancer. This highlights the need for quick and effective treatment when the cancer has spread.
Metastatic bladder cancer has spread to distant parts of the body. It has a 5-year survival rate of 8%. Treatment focuses on improving quality of life, though some may benefit from aggressive therapies.
“While the prognosis for metastatic bladder cancer is generally poor, new treatments like immunotherapy and targeted treatments offer hope,” says Dr. [Last Name], a specialist in urologic oncology.
It’s important to know the difference between non-muscle-invasive and muscle-invasive bladder cancer. This helps doctors figure out the best treatment and what to expect. The main difference is how deep the tumor is in the bladder wall.
About 90% of bladder cancer cases are non-muscle-invasive. These cases usually have a better outlook. On the other hand, muscle-invasive bladder cancer is more serious and can spread easily.
Non-muscle-invasive bladder cancer has a good prognosis. The 5-year survival rate is around 96% for the most common type. Most people with NMIBC can live a long time with the right treatment and follow-up care.
Muscle-invasive bladder cancer is much harder to treat. The 5-year survival rate is lower as the cancer goes deeper. Doctors often use radical surgery or other treatments to fight it.
It’s key to sort patients into risk groups within both types of bladder cancer. For NMIBC, doctors look at the tumor’s grade, size, and how often it comes back. For MIBC, how far the cancer has spread and if it’s in the lymph nodes are important.
| Disease Category | 5-Year Survival Rate | Treatment Approach |
| Non-Muscle-Invasive | 96% | TURBT, Intravesical Therapy |
| Muscle-Invasive | Varied, often lower | Radical Cystectomy, Chemotherapy, Bladder-Preserving Approaches |
Knowing the differences helps doctors create better treatment plans. This can lead to better outcomes and a better quality of life for patients.
Bladder cancer’s curability depends on several factors. These include the cancer’s stage and grade. We will look into what “cure” means in bladder cancer treatment. We will also examine cure rates based on stage and grade.
In bladder cancer, a “cure” means the cancer is gone, and the patient is disease-free. But, the term “cure” is complex. It depends on the cancer’s stage, grade, and the patient’s health.
Key factors influencing curability:
Cure rates for bladder cancer change based on stage and grade. Generally, non-muscle-invasive bladder cancer has a higher cure rate than muscle-invasive bladder cancer.
Recent data shows bladder cancer, when caught early, has a high cure rate. Advances in surgery, intravesical therapies, and immunotherapy have improved treatment results.
It’s important to know the difference between long-term remission and a complete cure. Long-term remission means the cancer is controlled, but it might come back. A complete cure means the cancer won’t come back.
For many bladder cancer patients, long-term remission is a big win. With ongoing care and follow-up, the chance of the cancer coming back can be low.
The way we treat bladder cancer greatly affects how well patients do and if they can be cured. We’ll look at the different treatments available. This includes their good points and downsides to see how they help fight bladder cancer.
Transurethral resection of bladder tumor (TURBT) is key for early bladder cancer. It removes the tumor from the bladder wall. This helps doctors know the cancer’s stage and grade. TURBT is often paired with intravesical therapy to stop the cancer from coming back.
For those with non-muscle-invasive bladder cancer (NMIBC), TURBT can be very effective. It gives them a good chance of being cured. But, they need to watch closely because the cancer can come back.
Radical cystectomy, or removing the bladder, is a big surgery for muscle-invasive bladder cancer or high-risk NMIBC. Thanks to better surgery methods, results have gotten better. Whether to have radical cystectomy depends on the cancer’s stage, grade, and the patient’s health.
How well someone does after radical cystectomy varies. Survival rates depend on the cancer’s stage at surgery. Those with cancer that’s only in the bladder do better than those with cancer that’s spread or in lymph nodes.
Bladder-preserving methods, like trimodal therapy (TMT), are options for some patients. TMT uses TURBT, chemotherapy, and radiation to get rid of the tumor without removing the bladder. This is great for patients who want to keep their quality of life.
Research shows bladder-preserving treatments can work as well as removing the bladder in the right patients. They also help keep urinary and sexual function.
Immunotherapy has changed how we treat advanced bladder cancer. Drugs like checkpoint inhibitors work well in patients with spread-out cancer. Immunotherapy is a hopeful option for those who’ve tried other treatments.
Targeted therapies focus on specific changes in the tumor. They aim to improve results by matching treatment to the patient’s tumor.
| Treatment Approach | Stage of Bladder Cancer | Curability Impact |
| TURBT | Early-stage (NMIBC) | High cure rate with close surveillance |
| Radical Cystectomy | Muscle-invasive or high-risk NMIBC | Improved survival with organ-confined disease |
| Bladder-Preserving Approaches | Selected muscle-invasive cases | Comparable survival to radical cystectomy with preserved bladder function |
| Immunotherapy | Advanced or metastatic disease | Promising outcomes in previously treated patients |
The chance of bladder cancer coming back is a big worry for patients. Even if the first treatment works, bladder cancer can come back. So, keeping an eye on the patient is very important.
Some things can make bladder cancer more likely to come back. These include:
Knowing these risk factors helps doctors plan better follow-up care. This can lead to better results for patients.
Regular checks are vital to catch cancer early. Cancer Research UK says these checks usually include:
“Regular cystoscopies, imaging tests, and urine cytology to monitor for any signs of cancer recurrence.”
Here’s what a typical check-up schedule might look like:
| Time After Treatment | Surveillance Method |
| 0-3 months | Cystoscopy and urine cytology |
| 6-12 months | Cystoscopy, urine cytology, and imaging tests |
When cancer comes back, how it’s treated depends on the stage and where it is. Doctors might use:
Regular checks can really help treat bladder cancer that comes back. It’s all about catching it early.
There are many factors that affect how bladder cancer will progress, beyond just the stage. The stage tells us how far the cancer has spread. But other factors help doctors guess how the cancer will grow and react to treatment.
Age and other health issues, or comorbidities, are key in bladder cancer prognosis. Older patients or those with other health problems might face more risks from treatment. Comprehensive geriatric assessment is now seen as important for older adults with bladder cancer. It helps doctors choose the best treatment based on the patient’s health.
The tumor grade is also important. It shows how much the tumor cells look like normal cells. High-grade tumors grow and spread faster. Molecular markers like TP53 or RB1 changes also affect how the tumor behaves and how it responds to treatment.
How well a patient responds to the first treatment is very telling. For non-muscle-invasive bladder cancer, how well the tumor reacts to BCG therapy is key. For muscle-invasive cancer, how the tumor responds to chemotherapy before surgery is very important.
Seeing doctors who specialize in bladder cancer matters too. High-volume centers often have better results for complex surgeries like radical cystectomy. This shows how important it is to get care from experts.
In summary, while the stage of bladder cancer is very important, other factors like age, comorbidities, tumor biology, treatment response, and access to specialized care also matter a lot. By looking at these factors, doctors can give more accurate predictions and tailor treatments to each patient’s needs.
It’s important to know how bladder cancer affects men and women differently. Studies show big differences in survival rates, how it’s diagnosed, and what affects its outcome.
Women often face a tougher battle with bladder cancer than men. The 5-year survival rate for women is lower. This gap is due to differences in how the cancer behaves and how well it responds to treatment.
Key statistics on gender-based survival differences:
Women often face longer waits before being diagnosed with bladder cancer. This delay is due to several reasons:
These delays mean women are diagnosed at a later stage. This makes treatment harder and survival chances lower.
Biological differences between men and women also impact bladder cancer prognosis. Hormones and genetics can change how the cancer grows and responds to treatment. Scientists are working to understand these differences and find treatments that work better for each gender.
Getting a diagnosis early and tailoring treatment is key. Knowing the gender differences in bladder cancer helps doctors give better care to patients.
Bladder cancer is more than just treatment. It’s about keeping a good quality of life. We must think about how the disease and its treatment affect daily life.
Bladder cancer treatment can change a person’s body. Patients might have trouble with their urine, like incontinence. Rehabilitation and supportive care help them adjust to these changes.
Some patients might need a urostomy after surgery. This means big changes in their daily life. Proper education and support from doctors can make a big difference.
The mind is also affected by bladder cancer. Patients often feel anxious, depressed, and scared of the cancer coming back. Access to mental health support is key to bettering their life quality.
Support groups, online or in-person, offer a community. They help patients understand they’re not alone. Connecting with others who share similar experiences is very helpful.
Bladder cancer treatment can also impact sex life and bladder control. Changes in sexual desire or function are common. Open discussions with healthcare providers can lead to solutions.
Urinary control issues, like incontinence, can greatly affect life quality. Pelvic floor rehabilitation and other treatments can help manage these problems.
Healthcare providers can offer more than just cancer treatment. They can support the whole patient. It’s about improving life quality, not just treating the cancer.
New hope is coming for bladder cancer patients. Advances in fields like immunotherapy and genetic testing are changing how we treat the disease. This is opening up new ways to fight cancer.
Immunotherapy has changed the game for bladder cancer treatment. Checkpoint inhibitors are showing great promise in treating advanced cases. These treatments help the immune system fight cancer cells better.
Research is also exploring other immunotherapy options. For example, BCG (Bacillus Calmette-Guérin) therapy is being looked at for non-muscle-invasive bladder cancer. New combinations and formulations are being tested to make these treatments even better.
The future of bladder cancer treatment is personalized. Genomic profiling helps find specific mutations in cancer cells. This allows for targeted treatments that are more likely to work.
Liquid biopsies are also emerging. They can find cancer DNA in blood or urine without surgery. This could change how we monitor and detect bladder cancer.
Clinical trials are key to finding new treatments for bladder cancer. Trials are looking at therapies like antibody-drug conjugates and PARP inhibitors. These trials offer hope for those who have tried standard treatments.
| Therapy Type | Description | Potential Benefit |
| Checkpoint Inhibitors | Drugs that release the brakes on the immune system | Enhanced immune response against cancer cells |
| Genomic Profiling | Identifying specific genetic mutations in cancer cells | Targeted therapies with higher efficacy |
| Liquid Biopsies | Detecting cancer DNA in blood or urine | Non-invasive monitoring and early detection of recurrence |
Looking ahead, the outlook for bladder cancer patients is getting better. With more research and clinical trials, we can expect even better treatments to come.
Bladder cancer’s outlook changes a lot based on when it’s found. Early detection is key, as it makes treatment more effective, mainly for non-muscle-invasive types. The 5-year survival rate for bladder cancer is about 77-78 percent.
This rate can change a lot based on the cancer’s stage when it’s found. Knowing about prognosis and treatment results is very important for both patients and doctors. We need to keep working on finding better ways to treat bladder cancer.
Early detection and the right treatment can make bladder cancer very treatable. As we get better at using immunotherapy and treatments tailored to each person, the future looks brighter for bladder cancer patients. We must keep working to improve treatment results and the quality of life for those with bladder cancer.
Bladder cancer can be fatal if not caught early. But, the outlook is generally good, mainly for non-muscle-invasive types. The 5-year survival rate varies with the stage at diagnosis.
The prognosis for bladder cancer greatly depends on its stage. Carcinoma in situ has a 96-97% survival rate. Localized bladder cancer has a 70-71% survival rate. Regional spread has a 39% survival rate. And, metastatic disease has an 8% survival rate.
Bladder cancer is staged using the TNM system. It looks at the tumor size and spread (T), nearby lymph nodes (N), and metastasis (M). This system helps figure out the prognosis and treatment options.
Non-muscle-invasive bladder cancer stays in the bladder lining and has a better prognosis. Muscle-invasive bladder cancer has gone through the bladder muscle layer. It’s more aggressive and needs more intense treatment.
Bladder cancer can be cured, mainly if caught early. “Cure” means the treatment has removed all cancer, and the patient is disease-free. Cure rates depend on the cancer’s stage and grade.
Treatments for bladder cancer include TURBT, radical cystectomy, and bladder-preserving methods. Immunotherapy is also used. The choice of treatment affects the disease’s curability, based on stage and grade.
Risk factors for bladder cancer coming back include the initial tumor’s stage and grade. Also, having multiple tumors and how well the initial treatment worked are important. Regular check-ups are key to catch recurrence early.
Beyond stage, factors like age, health conditions, tumor grade, and molecular markers influence outcomes. How well the initial treatment works and access to specialized care also play a role in treatment decisions.
Yes, men and women have different bladder cancer prognoses. Women often face delays in diagnosis, which can affect survival. Biological factors also impact prognosis.
Quality of life for bladder cancer patients includes physical changes, psychological impact, and support needs. Sexual function and urinary control are also important. Care that addresses these aspects improves outcomes.
New research and advances in immunotherapy, genetic testing, and personalized treatments are improving bladder cancer care. Ongoing clinical trials offer hope for more effective treatments and better patient outcomes.
Bladder cancer is highly curable if caught early, mainly for non-muscle-invasive types. Early detection greatly improves survival rates and treatment success.
The cure rate for bladder cancer varies with stage and grade. Early-stage bladder cancer has a higher cure rate than more advanced stages.
Metastatic bladder cancer has a lower survival rate. But, treatments like immunotherapy and targeted therapies can improve outcomes. The cure rate for metastatic disease is generally lower than for earlier stages.
Government Health Resource. (2025). What Is the Prognosis for Bladder Cancer and. Retrieved from https://www.cancer.org/cancer/types/bladder-cancer/detection-diagnosis-staging/survival-rates.html
Subscribe to our e-newsletter to stay informed about the latest innovations in the world of health and exclusive offers!