Last Updated on November 4, 2025 by mcelik

Bone dislocations are serious injuries that can significantly affect a person’s life. Nearly 1 in 5 people will experience a bone dislocation at some point. This makes it a common issue that needs quick and proper medical care.
Knowing the different dislocation types is key for effective treatment. We, as medical experts, give detailed care for patients with dislocated bones. We make sure they get the right treatment for their specific bone dislocation.
At our institution, we know how important accurate diagnosis and treatment are for bone dislocations. Our team is committed to giving top-notch healthcare. We also offer full support for international patients.
Understanding bone dislocations is key to diagnosing and treating orthopedic issues. A bone dislocation happens when bones in a joint move out of place. This causes pain, instability, and makes it hard to move.
A bone dislocation, or luxation, is when bones in a joint move out of place. This can happen from trauma, falls, or sports injuries. The joint’s anatomy affects how likely and severe a dislocation is.
Joints with more movement, like the shoulder or hip, are more at risk. The joint’s structure, the strength of surrounding ligaments, and any existing conditions also matter. For example, a dislocated humerus bone or dislocated femur bone can greatly affect limb function.
Dislocations and fractures are different injuries. A fracture is a bone break, while a dislocation is when bones at a joint move out of place. Sometimes, both happen together, creating a more complex injury.
Knowing the difference is important for the right treatment. For instance, treating a bone injury dislocation might be different than treating a fracture. It might focus on fixing the joint’s position and stability.
Signs of bone dislocation include severe pain, swelling, and bruising. The joint may also look deformed or be in an odd position. Sometimes, numbness or tingling can occur due to nerve damage.
Seeing these symptoms early is vital for getting medical help quickly. A doctor can diagnose it with a physical exam and imaging like X-rays or MRI. This helps understand the joint dislocation and bones involved.
Knowing the different types of bone dislocations is key for good treatment. Dislocations can happen anywhere in the body. Their type helps doctors plan the right treatment.
We sort bone dislocations by how bad they are, how complex, and how long they’ve been there. This helps us understand the injury better. Then, we can pick the best treatment.
Dislocations can be either complete or partial. A complete dislocation means the joint is fully broken, and the bones are out of place. A partial dislocation, or subluxation, is when the joint is only partially broken, and the bones are mostly in place.
Complete dislocations need more treatment and take longer to heal than partial ones. Knowing how bad the dislocation is helps us decide the best treatment.
We also classify dislocations by how complex they are. A simple dislocation has no fractures or major soft tissue damage. A complex dislocation has fractures, major soft tissue damage, or nerve and blood vessel injuries.
Complex dislocations need more advanced treatments, like surgery. This is to fix the extra injuries and help the bones heal right.
Dislocations can also be acute or chronic. An acute dislocation is a recent injury. A chronic dislocation has been there for a while, causing ongoing instability and possible more dislocations.
Chronic dislocations need longer, more intense treatments. This includes rehab and sometimes surgery. It’s to get the joint stable and working right again.
Understanding the types of bone dislocations helps doctors treat patients better. This knowledge is key for making the right treatment plans. It ensures patients get the best care for their recovery.

Dislocations in the shoulder area can be very painful. This is because the shoulder joint moves a lot. It’s also prone to injuries like bone dislocations.
The glenohumeral joint is the most likely to get dislocated. Glenohumeral joint dislocations happen when the humerus head pops out of the glenoid cavity. These can be anterior, posterior, or inferior, with anterior being the most common.
Anterior dislocations usually happen from falls onto an outstretched hand or direct blows to the shoulder. Symptoms include severe pain, limited mobility, and a visible deformity.
A dislocated clavicle, or collarbone, often occurs at the acromioclavicular or sternoclavicular joints. These injuries are common in contact sports and can result from falls or direct impacts.
Symptoms of a dislocated clavicle include pain, swelling, and difficulty moving the arm. Treatment often involves immobilization, pain management, and in some cases, surgical intervention.
Acromioclavicular dislocations involve the joint at the top of the shoulder, while sternoclavicular dislocations occur where the clavicle meets the sternum. Both types can result from trauma and may require different treatment approaches based on the severity.
| Type of Dislocation | Common Causes | Symptoms | Treatment |
| Glenohumeral | Falls, direct blows | Pain, limited mobility, deformity | Reduction, immobilization, surgery |
| Acromioclavicular | Falls, direct impacts | Pain, swelling, limited arm movement | Immobilization, pain management, surgery |
| Sternoclavicular | Trauma | Pain, swelling | Immobilization, pain management, surgery |
Scapular dislocations are rare but can occur due to severe trauma. They often involve associated injuries and require prompt medical attention.
“Scapular dislocations are often associated with other serious injuries, making thorough evaluation essential.” – Orthopedic Specialist
Knowing about the different types of shoulder bone dislocations is key for proper treatment and recovery. Each type has its own challenges and treatment options.
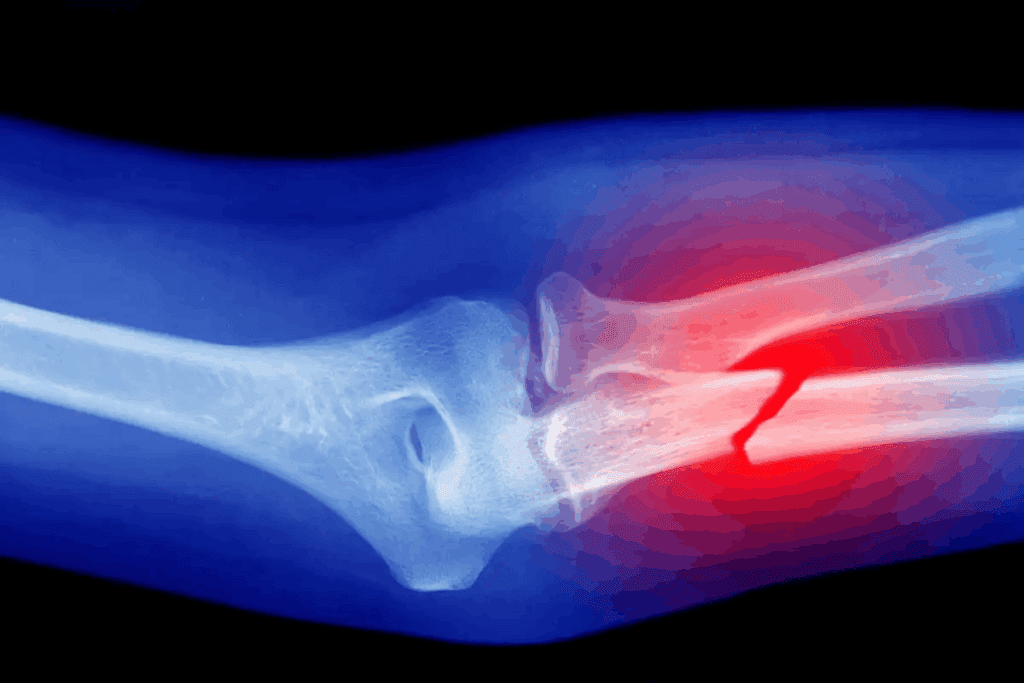
Understanding elbow bone dislocations is key for diagnosis and treatment. They can range from mild to severe. The elbow joint, a complex hinge joint, is prone to different types of dislocations.
The radius and ulna bones form the elbow joint. A dislocation happens when these bones are pushed out of place. This can result from a fall or a direct hit to the elbow.
Symptoms include severe pain, swelling, and difficulty moving the elbow. Treatment involves immediate medical care to fix the dislocation and keep the joint stable. Sometimes, surgery is needed to repair damaged tissues.
A radial head dislocation happens when the radius bone’s head is out of place. It’s common in kids and can occur from a sudden arm pull, like when lifting by the hand.
Nursemaid’s elbow, a type of radial head subluxation, is common in young children. It’s when the radius bone partially dislocates, causing pain and making the child reluctant to move the arm.
Nursemaid’s elbow affects kids under 4. It’s when the radius bone is partially dislocated, causing pain and making the child hold the arm in place.
Treatment for nursemaid’s elbow is simple. A healthcare professional gently puts the bone back in place. It can happen again, so parents are taught how to prevent it.
Complex elbow dislocations involve bone dislocation, fractures, or significant ligament damage. These are severe injuries needing detailed treatment, often surgery to fix the joint and repair damaged areas.
Rehabilitation after a complex elbow dislocation is vital for strength and mobility. Physical therapy is a key part of the recovery process.
Dislocations in the wrist and hand can make everyday tasks hard. The wrist and hand’s complex structure makes them prone to different dislocations. We’ll look at the causes, symptoms, and treatments for these dislocations.
Carpal bone dislocations happen in the wrist. They can result from falls or other injuries. Symptoms include pain, swelling, and limited wrist mobility. Doctors use X-rays or CT scans for diagnosis.
“The wrist is a complex joint, and injuries to this area can have significant consequences if not properly treated,” says an orthopedic specialist. Treatment may involve immobilization, closed reduction, or surgery, depending on the severity of the dislocation.
Metacarpal bones are the long bones in the hand that connect the wrist to the fingers. A dislocation can occur when these bones are forced out of their normal position, often due to a direct blow or fall. Symptoms include deformity, pain, and difficulty moving the affected finger.
Finger bone dislocations, also known as phalangeal dislocations, occur when the bones in the fingers are displaced. These injuries can result from sports accidents, falls, or other traumas. Treatment typically involves closed reduction, followed by immobilization to allow healing.
“Prompt treatment of finger dislocations is critical to prevent complications and restore normal function,” notes a hand surgeon.
The thumb is prone to dislocations due to its wide range of motion and exposure to trauma. A dislocated thumb can be very painful and may require immediate medical attention. Treatment may involve reduction and immobilization, with a focus on restoring thumb function.
Managing wrist and hand bone dislocations can be tough. But, with the right diagnosis and treatment, most people can fully recover and regain wrist and hand function.
The hip and pelvic area can suffer from different dislocations. Each has its own causes and effects. It’s important to know about these injuries to understand their impact on life.
A dislocated femoral head happens when the hip’s ball-and-socket joint is disrupted. This causes the femoral head to move out of place. Such injuries often come from high-energy events, like car crashes.
There are various types of femoral head dislocations. The most common are posterior, anterior, and central. Knowing the type helps doctors choose the right treatment.
| Type of Dislocation | Description | Common Causes |
| Posterior Dislocation | The femoral head is displaced posteriorly, often associated with dashboard injuries in car accidents. | High-energy trauma, such as motor vehicle accidents. |
| Anterior Dislocation | The femoral head is displaced anteriorly, typically resulting from forced abduction and external rotation. | Trauma, falls, and sports injuries. |
| Central Dislocation | The femoral head is driven into the pelvis, often due to a significant force applied to the greater trochanter. | Severe trauma, such as falls from height or direct blows to the hip. |
Pelvic ring dislocations happen when the pelvic ring is disrupted by trauma. These injuries can be complex and may need surgery to fix the pelvis.
Pelvic ring dislocations often come with other injuries. A detailed assessment and treatment plan are essential. The Young and Burgess classification helps doctors understand and treat these injuries.
Sacroiliac joint dislocations occur when the joint between the sacrum and ilium is disrupted. These injuries can be due to trauma or wear and tear. They can cause a lot of pain.
Diagnosing sacroiliac joint dislocations involves clinical checks and imaging. Treatment can be non-surgical or surgical, depending on the injury’s severity.
Congenital hip dislocation, or developmental dysplasia of the hip (DDH), is when the hip joint doesn’t form right. Early treatment is key to avoid long-term problems.
Managing congenital hip dislocations needs a team effort. Doctors, orthopedic specialists, and other healthcare professionals work together. Treatment can include the Pavlik harness or surgery, depending on the case.
Knee bone dislocations are a big problem in orthopedics. They need quick and good treatment to fix the knee and stop pain. We’ll look at the types, causes, symptoms, and how to treat them.
The kneecap can move out of place, often from a hit or twist. Patellar dislocations happen more in people with certain knee shapes. Treatment includes fixing the kneecap and exercises to make the muscles stronger.
Tibiofemoral joint dislocations happen when the tibia moves out of place. These are very painful and can come from big injuries. Quick doctor visits are key to check for nerve or blood vessel damage.
The joint between the tibia and fibula can also get out of place. This can cause knee pain and instability. Doctors use exams and scans to find out what’s wrong.
Meniscal dislocations happen when the meniscus tears and moves. This can make the knee feel stuck or catch. Surgery, like arthroscopy, is often needed to fix or remove the torn meniscus.
Treatment for knee bone dislocations depends on the problem. It can be simple care like rest and therapy or surgery for serious cases. The main goal is to fix the knee, ease pain, and avoid more problems.
It’s important to understand ankle and foot dislocations for the right treatment. These areas have many bones, joints, and ligaments. This makes them prone to different types of dislocations.
Ankle joint dislocations are serious and can happen from falls or sports injuries. They often come with fractures and ligament injuries. Prompt reduction and stabilization are key to avoid more damage and help healing.
Subtalar joint dislocations affect the talocalcaneal and talonavicular joints without a fracture. These are rare but hard to diagnose and treat. Early recognition is vital to prevent long-term issues like arthritis and chronic instability.
Midfoot dislocations can happen alone or with fractures. They usually come from big traumas. Treatment often includes reduction and immobilization. Surgery might be needed for more serious cases.
Toe bone dislocations are less severe but can be painful and affect function. They can happen from direct trauma or sports injuries. Treatment usually involves manual reduction and then immobilization to heal.
In summary, ankle and foot bone dislocations are various injuries needing careful evaluation and treatment. Knowing the specifics of each dislocation is essential for the best care.
It’s important for both patients and doctors to understand spinal bone dislocations. These happen when vertebrae don’t line up right. This can be due to injury, medical conditions, or being born with it.
Cervical vertebrae dislocations are serious because they can harm the nerves. They can happen in the upper or lower neck. Quick medical help is key to avoid lasting damage.
Dislocations in the middle and lower back can come from big injuries. This includes car accidents or falls. These injuries might need detailed treatment.
Facet joint dislocations happen when the joints between vertebrae get out of place. This can happen anywhere in the spine. Sometimes, surgery is needed to fix it.
Atlantoaxial dislocations affect the top two neck vertebrae. This is a serious issue that can cause neck instability. It needs careful handling.
Surgery might be done to fix the spine. The aim is to make it stable again, reduce pain, and stop nerve damage.
Dislocations of the jaw and facial bones can greatly affect a person’s life. They impact both how well you can function and your looks. These injuries can happen from many things, like accidents, sports injuries, or some health issues.
We know that jaw and facial bone dislocations need quick and accurate medical checks. This is to avoid lasting problems and get your normal function back.
The temporomandibular joint (TMJ) links the jawbone to the skull. It’s key for jaw movement. TMJ dislocations happen when the jawbone moves out of place. This can cause pain, trouble closing your mouth, and jaw clicking or locking.
TMJ dislocations can be from yawning, laughing, or other wide-mouth actions. Treatment often includes manually putting the jaw back in place. Then, rest and physical therapy might be needed to strengthen the muscles.
Nasal bone dislocations can happen from hitting the nose, like from a fall. These can make your nose look crooked or misshapen. They might also make breathing hard. Accurate diagnosis through imaging is key to see how bad the injury is.
Treatment for nasal bone dislocations might be manual reduction or, for more serious cases, surgery. Surgery aims to fix the nasal bones and improve breathing.
The orbit is made of several bones that protect the eye. Orbital bone dislocations can come from big trauma. They might cause double vision, a sunken eye, or even vision loss.
Orbital bone dislocations need careful checks by experts. This often means working with eye doctors and maxillofacial surgeons. Treatment might be surgery to fix the orbit and keep your vision.
In summary, jaw and facial bone dislocations are serious and need detailed medical care. Knowing the causes, symptoms, and treatments helps us give the right care. This way, we can help restore function and appearance.
It’s important to know why bone dislocations happen. This knowledge helps in preventing and treating them. Bone dislocations can really affect someone’s life, so it’s key to find and handle the causes.
Most bone dislocations come from accidents. These can be from falls, sports injuries, or car crashes. The force from these events can push joints out of place.
Not all dislocations come from accidents. Some happen without trauma, often because of health issues or how the body is built.
Some health conditions and genetics can make you more likely to get bone dislocations. This includes connective tissue disorders and conditions that affect muscle and joint stability.
Some activities can increase the chance of bone dislocations. These often involve big impacts, heavy lifting, or constant strain on joints.
Knowing the causes and risks can help prevent bone dislocations. It’s also important to get medical help when needed. Treating dislocated bones means fixing the injury and dealing with the underlying causes to avoid future problems.
Diagnosing dislocated bones involves several steps. These include a physical exam, imaging studies, and ruling out other conditions. We aim to give patients the right treatment quickly and accurately.
The first step is a detailed physical exam. We look for signs like deformity, swelling, and bruising. We also consider the patient’s medical history for clues.
We check how well the joint moves and do specific tests. For example, we might use the apprehension test for shoulder dislocations. This test checks how the patient reacts to certain movements.
Imaging studies are key to confirming a dislocated bone diagnosis. X-rays are often the first choice. They quickly show bone alignment and fractures.
For more complex cases, we might use Computed Tomography (CT) scans or Magnetic Resonance Imaging (MRI). CT scans help with complex dislocations and bone structure checks. MRI is great for soft tissue injuries like ligament and tendon damage.
Differential diagnosis is important. It helps us rule out other conditions that might look like a dislocated bone. We look at things like fractures, sprains, and soft tissue injuries.
It involves both clinical checks and imaging studies. For example, we might need to tell apart a dislocated shoulder from a fracture-dislocation. A systematic approach ensures accurate diagnosis and treatment.
Dislocated bones need different treatments. These range from simple manual methods to more complex surgeries. We’ll look at how to manage these injuries effectively.
Closed reduction is a non-surgical method. A healthcare provider moves the bone back into place without cutting. It’s often used for simple cases and can be done under sedation or local anesthesia to reduce pain.
Benefits of Closed Reduction:
When closed reduction doesn’t work, surgery might be needed. Surgery can stabilize the joint, repair damaged tissues, and align the bone properly.
Types of Surgical Interventions:
After fixing a dislocated bone, keeping it stable is key. This is done with casts, splints, or slings, based on the injury’s location and severity.
| Immobilization Method | Typical Use | Duration |
| Casts | Fractures or dislocations needing strong support | 4-6 weeks |
| Splints | Milder injuries or post-surgical support | 2-4 weeks |
| Slings | Shoulder or upper arm injuries | 1-3 weeks |
Managing pain is vital in treating dislocated bones. We use both medicines and non-medical methods to control pain.
Pharmacological Methods:
Understanding the treatments for dislocated bones helps us offer complete care. This care meets both immediate needs and long-term recovery goals.
Getting better after a dislocated bone is all about regaining strength and moving freely again. The plan for getting better is made just for you. It depends on the joint affected and how bad the dislocation was.
Physical therapy is key in getting back on track after a dislocated bone. We create a special workout plan for you. It helps improve how well you can move, makes muscles stronger, and keeps the joint stable.
For example, if you dislocated your shoulder, you might do exercises like pendulum swings and wall slides. These help you move better over time.
Our physical therapists work with you closely. They check how you’re doing and change the plan if needed. This teamwork helps you get back to doing what you love faster.
How long it takes to get back to normal depends on the dislocation’s severity and your health. Here’s a general idea of what to expect:
| Recovery Stage | Timeline | Activities |
| Immediate Post-Injury | 0-2 weeks | Rest, immobilization, pain management |
| Early Rehabilitation | 2-6 weeks | Range of motion exercises, strengthening |
| Advanced Rehabilitation | 6-12 weeks | Progressive strengthening, functional activities |
| Return to Full Activity | 3-6 months | Full participation in sports or heavy activities |
Doing exercises to strengthen and stabilize is very important. These exercises help in several ways:
For instance, after a knee dislocation, you might do exercises like straight leg raises and quadriceps sets. These help strengthen the muscles around the knee.
“Rehabilitation after a dislocation is not just about regaining strength; it’s about restoring function and preventing future injuries.”
An Orthopedic Specialist
Managing a dislocated bone long-term means ongoing care to avoid future problems. This care includes:
By sticking to a detailed rehabilitation plan, you can recover well and avoid future issues.
Bone dislocations can cause many problems that affect a person’s life a lot. We will look at the issues that can happen, like their causes, signs, and how to deal with them.
Neurovascular injuries are serious problems from bone dislocations. They can harm nerves and blood vessels near the joint. This can cause numbness, tingling, and poor blood flow.
Common neurovascular injuries associated with bone dislocations include:
Joint instability is another issue after a bone dislocation. Damage to ligaments and tissues can make the joint unstable. This raises the chance of more dislocations.
Factors contributing to joint instability include:
Post-traumatic arthritis is a long-term problem from bone dislocations. It happens because of the injury and damage to the joint. This can cause chronic pain, stiffness, and less mobility.
Avascular necrosis happens when the bone’s blood supply is cut off. This leads to bone death. It can cause a lot of pain and make it hard to move.
Risk factors for avascular necrosis include:
| Complication | Description | Risk Factors |
| Neurovascular Injuries | Damage to nerves and blood vessels | Severe trauma, complex dislocations |
| Joint Instability | Increased risk of recurrent dislocations | Inadequate rehabilitation, anatomical abnormalities |
| Post-Traumatic Arthritis | Chronic pain and stiffness | Initial injury severity, joint damage |
| Avascular Necrosis | Bone death due to disrupted blood supply | Severe trauma, delayed treatment |
Different groups face unique challenges when it comes to bone dislocations. We must take these into account to give the best care.
Children’s bones and joints are different from adults. Children’s bones are more prone to certain types of injuries, like growth plate fractures. These can affect how their bones grow.
When treating children, we use gentle methods and watch closely to help them heal right. Prior approval may be needed for some treatments in kids, showing we need to plan carefully.
| Age Group | Common Dislocation Types | Treatment Considerations |
| 0-5 years | Nursemaid’s elbow, clavicle fractures | Gentle reduction, immobilization |
| 6-12 years | Elbow dislocations, forearm fractures | Closed reduction, physical therapy |
| 13+ years | Shoulder dislocations, complex elbow dislocations | Surgical intervention, rehabilitation |
Older adults are more likely to get bone dislocations because their bones are weaker. Osteoporosis is a big risk factor for fractures and dislocations in this group. We must be careful to avoid making things worse.
When treating older adults, we look closely at their bone health and any other health issues. Pain management is key to keep them comfortable and help them recover.
Athletes are at high risk for bone dislocations because of the demands of sports. Shoulder and knee dislocations are common in athletes. We need to treat them quickly and effectively to get them back playing fast.
When treating athletes, we consider the sport and their role in it. Return to play criteria are strict to keep them safe and prevent injuries.
People with connective tissue disorders, like Ehlers-Danlos syndrome, are more likely to have joint dislocations. These patients need special care to manage their condition and avoid problems.
We must watch for joint problems in these patients and plan for long-term care. Multidisciplinary care is often needed to meet their complex needs.
Knowing about the different types of dislocated bones is key for proper treatment. We’ve looked at various bone dislocations, their causes, symptoms, and how to treat them. Each type, from shoulder to spinal dislocations, needs a special treatment plan.
The recovery process is just as important. It includes healing, rehabilitation, and long-term care to avoid future problems. We talked about the importance of proper rest, managing pain, and physical therapy for a good recovery.
Healthcare experts can greatly improve patient care by understanding each dislocation type well. Whether it’s an immediate or ongoing issue, knowing the details is essential for top-notch care.
A bone dislocation happens when a bone moves out of its joint. This disrupts the bone’s normal position.
There are many types of bone dislocations. They include complete vs. partial, simple vs. complex, and acute vs. chronic. Each type varies in severity and injury nature.
Dislocations are when a bone moves out of its joint. Fractures are when a bone breaks or cracks.
Signs and symptoms include severe pain, swelling, and bruising. You might also have limited mobility and see deformity in the affected area.
Doctors use physical exams, X-rays, and MRI scans to diagnose. They might also check for nerve and blood vessel damage.
Treatment options include closed reduction, surgery, and immobilization. Pain management is also important, depending on the injury.
Rehab involves physical therapy and exercises. The goal is to strengthen and stabilize the area to prevent future injuries.
Complications include nerve and blood vessel damage. You might also face joint instability, arthritis, and bone death.
Yes, kids, older adults, athletes, and those with certain conditions are at higher risk. This is due to various factors.
While some dislocations can’t be avoided, prevention is possible. Wear protective gear, stay strong, and avoid risky activities.
Recovery time varies. It depends on the injury’s severity, treatment success, and individual factors. It usually takes weeks to months of rehab.
Recurring dislocations can cause chronic instability and degeneration. They also increase the risk of arthritis. Proper treatment and prevention are key.
Benoist, M. (2002). The natural history of lumbar degenerative spinal stenosis: A comprehensive review. Joint Bone Spine, 69(5), 450-457. https://www.sciencedirect.com/science/article/abs/pii/S1297319X02004293
Subscribe to our e-newsletter to stay informed about the latest innovations in the world of health and exclusive offers!