Shocking Eyelid Surgery Warning Signs & Care
When the immune system attacks the eyes’ healthy tissues, it can cause serious problems. Conditions such as uveitis and dry eye disease can severely affect your vision and quality of life. Understanding these diseases and recognizing their early signs is essential for proper management. If you are worried about a Bad Blepharoplasty, learning the 5 shocking warning signs of eyelid surgery gone wrong can help you take action early and explore treatment options.
Today, modern medicine offers new ways to manage autoimmune eye conditions. These include specialized eye drops, oral medications, and advanced biologic agents. At Liv Hospital, we combine the latest innovations in ophthalmology and immunology to support patients with both common and rare eye diseases, including those dealing with complications similar to Bad Blepharoplasty outcomes.

Key Takeaways
- Autoimmune eye diseases occur when the immune system attacks the eye’s healthy tissues.
- Conditions like uveitis and dry eye disease can lead to serious ocular complications.
- Modern treatment approaches include topical and systemic medications.
- Liv Hospital offers a patient-centered approach combining ophthalmology and immunology expertise.
- Effective management of autoimmune eye diseases requires understanding the condition and available treatments.
Understanding Autoimmune Eye Disease
Autoimmune eye diseases occur when the immune system mistakenly targets the delicate tissues of the eye. This immune response can lead to inflammation, discomfort, and even vision loss. In some cases, symptoms may overlap with issues seen in patients experiencing a Bad Blepharoplasty, making early evaluation essential.

What Happens When Your Immune System Attacks Your Eyes
When the immune system attacks the eyes, it can cause inflammation and damage. This can lead to autoimmune uveitis or dry eye disease linked to other autoimmune disorders.
Common Symptoms and Warning Signs
Common symptoms include eye pain, redness, blurred vision, and dryness. Autoimmune eye diseases vary widely, from mild irritation to severe visual impairment. Some patients may confuse these symptoms with complications from a Bad Blepharoplasty, which makes proper diagnosis even more important.
Symptom | Description | Associated Conditions |
Eye Pain | Sharp or dull pain in or around the eyes | Autoimmune Uveitis, Scleritis |
Redness | Visible redness due to inflammation | Uveitis, Conjunctivitis |
Blurred Vision | Distorted or unclear vision | Uveitis, Optic Neuritis |
Dryness | Feeling of dryness or grittiness in the eyes | Dry Eye Disease, Sjögren’s |
Types of Autoimmune Eye Diseases
It’s important to know about different autoimmune eye diseases. Each one affects the eye in its own way. Understanding them helps doctors diagnose and treat them better.
Dry Eye Disease in Autoimmune Conditions
Dry eye disease is common in people with autoimmune disorders like Sjögren’s syndrome. It happens when the eyes don’t make enough tears or when the tears are bad. This can cause eye pain, vision issues, and eye infections.
Proper management of dry eye disease is vital to alleviate symptoms and prevent complications.
Ocular Manifestations of Rheumatoid Arthritis and Lupus
Rheumatoid arthritis and lupus can affect the eyes. Rheumatoid arthritis can cause dry eye, scleritis, and uveitis. Lupus can lead to retinal vasculitis, optic neuritis, and other eye problems.
Regular eye examinations are critical for patients with these conditions to detect and manage eye-related issues early.
Rare Autoimmune Eye Disorders
Rare conditions like Mooren’s ulcer and sympathetic ophthalmia require expert evaluation. Early treatment is essential to prevent complications that may resemble post-surgical issues, including those associated with Bad Blepharoplasty cases.
Prevalence and Risk Factors
It’s important to know about autoimmune eye diseases to manage them well. These diseases can really affect a person’s life.
Statistics in the United States
Studies in the U.S. have given us useful data. For example, autoimmune uveitis affects 52.4 people per 100,000. It’s also found in 115.3 people per 100,000.
This shows how critical it is to catch these diseases early. We need good healthcare plans to deal with them.
Condition | Incidence (per 100,000) | Prevalence (per 100,000) |
Autoimmune Uveitis | 52.4 | 115.3 |
Dry Eye Disease | Varies | Significant among autoimmune patients |
Who Is Most at Risk ?
Some groups face a higher risk of these diseases. People with a family history are more likely to get them.
Key risk factors include:
- Family history of autoimmune diseases
- Presence of other autoimmune conditions
- Genetic predisposition
- Environmental triggers
Genetic and Environmental Triggers
Genes and the environment both play a part in these diseases. Knowing what triggers them helps in early treatment.
Genetic triggers are inherited and make some people more likely to have autoimmune diseases. Environmental triggers can be infections, chemicals, or other things that start an autoimmune response.
Understanding these factors helps doctors create better prevention and treatment plans for autoimmune eye diseases.
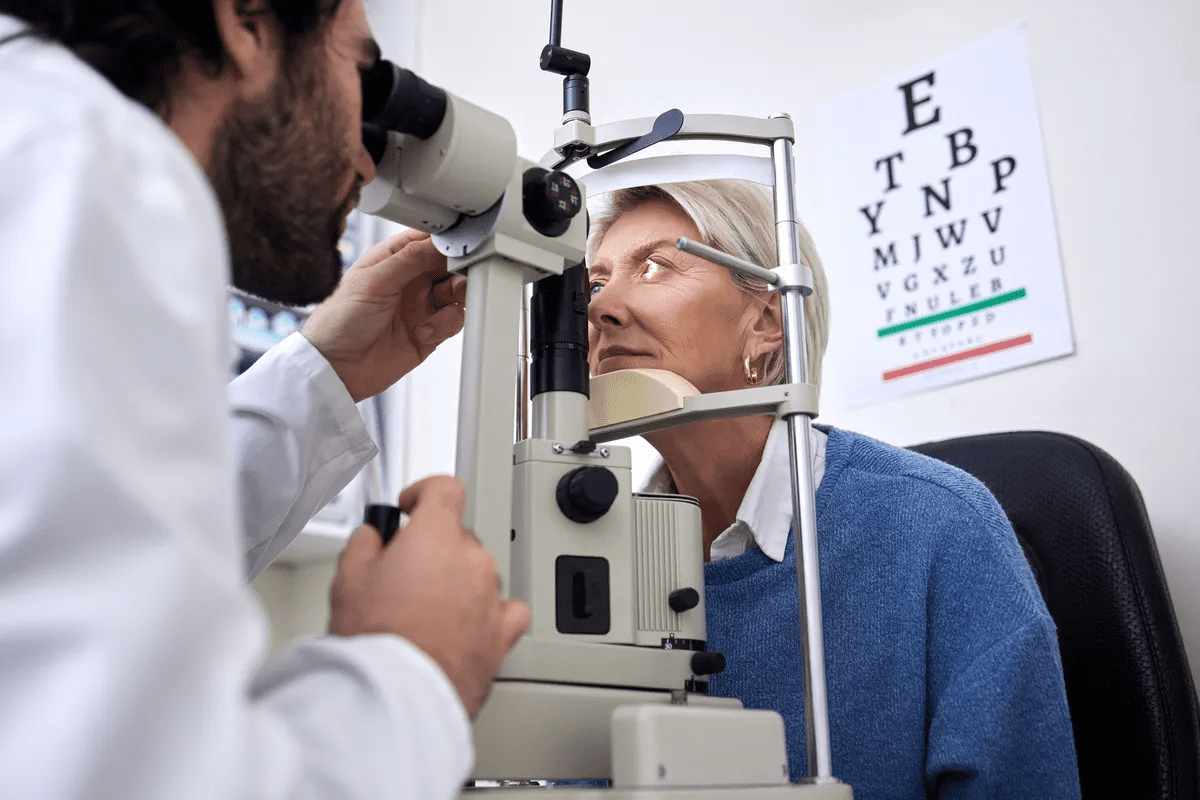
Diagnosing Autoimmune Eye Conditions
Accurate diagnosis includes clinical evaluation, laboratory testing, and imaging such as OCT. Differential diagnosis helps distinguish autoimmune disease from surgical complications, including those seen after a Bad Blepharoplasty.
Clinical Evaluation Process
The first step is a thorough clinical evaluation. It looks at the patient’s medical history and does a detailed eye check. A complete eye exam is essential to see how bad the disease is.
We search for signs like redness, pain, light sensitivity, and vision changes. This detailed check helps us understand how severe the condition is and what might be causing it.
Laboratory Tests and Imaging
Laboratory tests are key in confirming autoimmune eye diseases. They include blood tests to look for specific markers and signs of inflammation. Imaging studies, like optical coherence tomography (OCT), help us see inside the eye and check for damage.
OCT imaging gives us clear pictures of the retina and other important eye parts. This info is very helpful for making a correct diagnosis and planning treatment.
Differential Diagnosis Considerations
Differential diagnosis is important because it helps rule out other possible causes of symptoms. We look at many other conditions that could cause similar eye problems. This ensures we get the right diagnosis.
By using the results from clinical checks, lab tests, and imaging, we can make a well-informed diagnosis. Then, we can create a treatment plan that fits the patient’s needs.
Autoimmune Eye Disease Treatment Options
Autoimmune eye diseases need a mix of treatments because they are complex. Each treatment is chosen based on the disease and the patient’s needs.
First-Line Treatments
First treatments aim to reduce inflammation and manage symptoms. Topical immunomodulators like cyclosporine and tacrolimus are often used. They are good for conditions like dry eye disease linked to autoimmune diseases.
These drugs change the immune response at the disease site. This helps avoid side effects seen with other treatments. Sometimes, corticosteroid eye drops are used for their strong anti-inflammatory effects. But, they are not used for long because of possible side effects like cataracts and high eye pressure.
Advanced Treatment Approaches
For those not helped by first treatments or with severe disease, more advanced treatments are considered. Systemic immunosuppressants are used to control the immune system more broadly. This is key for diseases like autoimmune uveitis or eye problems from rheumatoid arthritis and lupus.
Biologic agents are another advanced option. They target specific parts of the immune response. This offers a more precise way to fight inflammation and disease. For example, TNF inhibitors are effective against many autoimmune eye diseases.
Treatment Approach | Examples | Use Cases |
Topical Immunomodulators | Cyclosporine, Tacrolimus | Dry eye disease, mild uveitis |
Systemic Immunosuppressants | Methotrexate, Azathioprine | Severe uveitis, ocular manifestations of systemic autoimmune diseases |
Biologic Agents | TNF inhibitors (e.g., Infliximab) | Severe autoimmune eye diseases, refractory cases |
Creating a Personalized Treatment Plan
Creating a treatment plan that fits the patient is key. It considers the patient’s health, disease severity, and past treatment responses. This ensures the best care for autoimmune eye diseases.
Regular check-ups with healthcare providers are vital. They help adjust the treatment plan and watch for medication side effects. Teaching patients how to use their medications correctly is also important for managing the disease well.
Topical Treatments and Eye Drops
Topical treatments and eye drops are key in managing autoimmune eye diseases. They are applied directly to the eye. This helps relieve symptoms like dryness, inflammation, and discomfort.
Immunomodulators: Cyclosporine and Tacrolimus
Immunomodulators like cyclosporine and tacrolimus help control the immune response in the eye. Cyclosporine is great for treating dry eye caused by autoimmune conditions. It boosts tear production and cuts down inflammation. Tacrolimus is used when cyclosporine doesn’t work well because it’s very effective at suppressing the immune system.
Immunomodulator | Primary Use | Benefits |
Cyclosporine | Dry eye associated with autoimmune conditions | Increases tear production, reduces inflammation |
Tacrolimus | Potent immunosuppression | Effective in severe cases, potent anti-inflammatory |
Corticosteroid Eye Drops
Corticosteroid eye drops are good at reducing inflammation. They’re often used for short-term management of acute flare-ups. But, they can cause side effects like cataracts and high eye pressure. So, they’re used carefully.
Artificial Tears and Lubricants
Artificial tears and lubricants are vital for treating dryness and discomfort in autoimmune eye diseases. They keep the eye surface healthy. They can be used as needed during the day.
- Preservative-free options to minimize irritation
- Gel and ointment formulations for prolonged relief
- Options with anti-inflammatory properties
Proper Application Techniques
It’s important to apply eye drops correctly to get the best results and avoid side effects. Patients should wash their hands before use, avoid touching the dropper tip, and keep their eyes closed for a few minutes after application. This lets the medication work properly.
- Wash hands thoroughly before application
- Tilt head back and pull down lower lid
- Instill prescribed number of drops
- Keep eyes closed for 1-2 minutes
Systemic Medications for Autoimmune Eye Diseases
Autoimmune eye diseases are often treated with systemic medications. These drugs help control inflammation and weaken the immune system. They are key for severe cases that harm vision or are linked to other autoimmune disorders.
Conventional Immunosuppressants
Immunosuppressants are a mainstay in treating autoimmune eye diseases. Drugs like methotrexate and azathioprine reduce the immune system’s overactive response. They lessen the disease’s severity and prevent lasting damage.
“Immunosuppressive therapy has changed how we treat autoimmune eye diseases,” says a leading expert. “It gives patients a way to manage their condition effectively.”
Corticosteroids
Corticosteroids are strong anti-inflammatory drugs used for autoimmune eye diseases. They are effective but can have side effects with long-term use. Prednisone is a common corticosteroid given orally or by injection.
Managing Medication Side Effects
It’s vital to manage the side effects of systemic medications. Regular check-ups with healthcare providers are needed to adjust treatment as necessary. Minimizing side effects while keeping treatment effective is a challenge.
Strategies for managing side effects include adjusting doses, switching medications, and supportive care. For example, patients on long-term corticosteroids may need to watch for osteoporosis and other side effects.
- Regular monitoring of blood counts and liver function
- Adjusting medication dosages based on patient response
- Implementing preventive measures for known side effects
By managing systemic medications and their side effects, healthcare providers can improve outcomes for patients with autoimmune eye diseases. This leads to a better quality of life.
Biologic Therapies and Advanced Treatments
Biologic therapies have changed how we treat autoimmune eye diseases. They offer hope to those with severe or hard-to-treat conditions. These treatments target the immune system, helping manage eye problems caused by autoimmune disorders more effectively.
TNF Inhibitors
TNF inhibitors are a type of biologic therapy. They work well against autoimmune diseases, including those affecting the eyes. By stopping tumor necrosis factor-alpha (TNF-alpha), they reduce inflammation and slow disease growth. Etanercept, infliximab, and adalimumab are some of these medicines.
Key Benefits of TNF Inhibitors:
- Reduced ocular inflammation
- Improved visual outcomes
- Potential to decrease reliance on corticosteroids
B-Cell Therapies
B-cell therapies are another promising area. They target B cells, key players in many autoimmune diseases. Rituximab, a monoclonal antibody, has helped manage eye symptoms of autoimmune diseases by reducing B cells.
Emerging Treatment Options
The field of biologic therapies for autoimmune eye diseases is growing. Scientists are looking into new targets and developing new treatments. Some of these include:
Treatment | Target | Potential Benefits |
Interleukin inhibitors | IL-6, IL-17, IL-23 | Reduced inflammation, improved safety profile |
Janus kinase (JAK) inhibitors | JAK pathways | Oral administration, rapid onset of action |
Stem cell therapies | Regeneration of ocular tissues | Potential for tissue repair and regeneration |
As research moves forward, we’ll see more targeted and effective treatments. This brings hope to patients and doctors alike.
Working with Healthcare Providers
Managing autoimmune eye diseases requires a coordinated medical team. Patients should ask detailed questions, track symptoms, and attend regular follow-ups. This is especially important when distinguishing autoimmune inflammation from complications resembling Bad Blepharoplasty outcomes.
Building Your Medical Team
Starting with a good medical team is key. This team usually includes:
- An ophthalmologist who knows about uveitis or autoimmune eye issues
- A rheumatologist to handle systemic autoimmune diseases
- A primary care doctor to oversee overall health
- Other specialists like immunologists or genetic counselors when needed
Coordinating Care Between Specialists
It’s important to coordinate care among specialists. Patients should:
- Keep a detailed record of their medical history and treatments
- Make sure to see each specialist regularly
- Talk openly about their symptoms and treatment plans
This helps avoid conflicting treatments and keeps everyone informed about the patient’s health.
Questions to Ask Your Doctor
Patients should ask questions about their condition and treatment. Some key questions include:
Category | Sample Questions |
Diagnosis | What is the specific diagnosis of my autoimmune eye disease? |
Treatment | What are the available treatment options for my condition? |
Prognosis | What can I expect in terms of disease progression and outcomes? |
Monitoring Disease Progression
Keeping an eye on how the disease is progressing is vital. This means:
- Regular eye exams to check on the disease
- Imaging tests like OCT or fluorescein angiography
- Blood tests to watch inflammation and medication levels
By working closely with healthcare providers, patients can get better results and live a better life.
Lifestyle Management and Self-Care
Managing autoimmune eye diseases goes beyond medical treatments. Lifestyle changes and self-care are key. By focusing on diet, environment, and stress, patients can improve their condition.
Dietary Considerations
Eating a balanced diet is vital for eye health. Foods like salmon and flaxseeds are great because they fight inflammation. “A diet rich in anti-inflammatory foods can greatly help manage autoimmune eye diseases,” says an expert.
Drinking plenty of water is also important for eye health. Cutting down on processed foods and sugars can help reduce inflammation too.
Environmental Modifications
Changing your environment can help with autoimmune eye disease symptoms. Stay away from dry, windy places and use humidifiers to fight dry eyes. Wearing sunglasses that wrap around your face protects your eyes from UV rays and wind.
Long hours in front of screens can strain your eyes. Remember the 20-20-20 rule to avoid this. Look away from your screen every 20 minutes and focus on something 20 feet away for 20 seconds.
Stress Management Techniques
Stress can make autoimmune conditions worse, including eye diseases. Stress-reducing activities like meditation, yoga, or deep breathing can help. “Adding stress management to your daily routine can improve your health and eye health,” says a healthcare professional.
Regular exercise and enough sleep are also key for managing stress and staying healthy.
Support Groups and Resources
Connecting with others who face similar challenges can be very helpful. Support groups, online or in-person, offer a place to share and learn. They provide insights and new strategies for managing your condition.
Using resources like educational materials and patient advocacy groups can empower you. “Being part of a community that understands autoimmune eye diseases can greatly impact your journey,” says a patient advocate.
Conclusion
Managing autoimmune eye diseases requires a combination of medical treatment, lifestyle strategies, and ongoing support. By understanding symptoms, risk factors, and treatment options, patients can take control of their eye health. A comprehensive approach also helps differentiate autoimmune symptoms from surgical issues such as those linked to a Bad Blepharoplasty, ensuring proper and timely care.
Treatment for autoimmune eye diseases includes many options. These range from eye drops and topical treatments to systemic drugs and biologic therapies. Our guide has covered these in detail. It shows how important it is to tailor treatment to each person.
Lifestyle changes are key in managing the disease. Eating right, making environmental changes, and managing stress can help eye health. These steps can improve overall well-being.
By taking a full approach to managing autoimmune eye disease, symptoms can lessen, and the disease can progress slower. We aim to offer top-notch healthcare and support to international patients. We hope this guide has given you useful insights and information for your journey with autoimmune eye disease.
Frequently Asked Questions
What are autoimmune eye diseases?
Autoimmune eye diseases happen when the immune system attacks the eyes’ healthy tissues. This leads to eye problems.
What are the common symptoms of autoimmune eye diseases?
Symptoms include eye pain, redness, blurred vision, and dryness.
What is autoimmune uveitis?
Autoimmune uveitis can cause blindness if not treated. It’s when the immune system attacks the eye’s middle layer.
How does lupus affect the eyes?
Lupus can cause dry eye, uveitis, and retinal vasculitis. These affect different parts of the eye.
What is the prevalence of autoimmune eye diseases in the United States?
In the U.S., autoimmune uveitis affects 52.4 per 100,000 people. It has a prevalence of 115.3 per 100,000.
How are autoimmune eye diseases diagnosed?
Diagnosis includes a thorough check-up, blood tests, and imaging like OCT.
What are the treatment options for autoimmune eye diseases?
Treatments include eye drops, medicines, biologic agents, and lifestyle changes.
What are the benefits of biologic therapies in treating autoimmune eye diseases?
Biologic therapies target the immune system. They offer hope for severe cases.
How can I manage my autoimmune eye disease effectively?
Work with your doctor, make lifestyle changes, and use treatments.
What lifestyle changes can help manage autoimmune eye diseases?
Eat omega-3 rich foods, avoid dry eye triggers, and manage stress with meditation and yoga.
Can autoimmune eye diseases be cured?
Some can be managed well, but a cure isn’t always possible. Treatment aims to control symptoms and prevent damage.