Last Updated on November 25, 2025 by
We use a uroflow test to find different urological problems. It measures how fast and in what pattern urine flows. This test is non-invasive and gives us important information about the urinary system. It helps us spot possible issues, including abnormalities in the normal urine output in one hour, which is essential for monitoring urinary health.
Uroflowmetry is a key tool for diagnosing issues like Benign Prostatic Hyperplasia (BPH), bladder outlet obstruction, and neurogenic bladder. By looking at the flow rate and pattern, we understand the causes of urinary problems better.
The uroflow test also helps find other urological problems, like urethral stricture and detrusor underactivity. Knowing about these conditions is key to giving the right treatment and care.
Uroflowmetry is a key tool for checking urinary health. It measures urine flow rate and pattern. This test is non-invasive and helps diagnose and manage urinary issues.
Understanding uroflowmetry helps patients grasp their urinary health better. It also clarifies the diagnostic process.
A uroflow test tracks urine flow and volume per second. It shows how well the bladder and sphincter work. Patients urinate into a special device that records flow and volume.
The test gives important measurements like maximum and average flow rates, and total urine volume. The maximum flow rate is key, showing the peak flow during urination.
A low maximum flow rate might mean an obstruction or urinary issue. These measurements help doctors diagnose problems like benign prostatic hyperplasia (BPH) or bladder outlet obstruction.
Preparing for a uroflow test is easy. Patients should arrive with a full bladder. Avoiding caffeine and diuretics before the test is also advised.
Following these tips ensures accurate test results.
Understanding Benign Prostatic Hyperplasia (BPH) is key to diagnosing urinary issues in men. BPH is when the prostate gland gets bigger. This can really affect how well you can urinate.
“The prostate gland is very important for men’s health,” says a top urologist. “As men get older, the chance of getting BPH goes up. So, it’s common in older men.”
BPH can cause many urinary problems. The big prostate can squeeze the urethra. This makes it hard to start or keep urinating.
BPH can really mess with how you pee. Men might find it hard to start, have a weak or broken flow, pee a lot, or not empty their bladder fully.
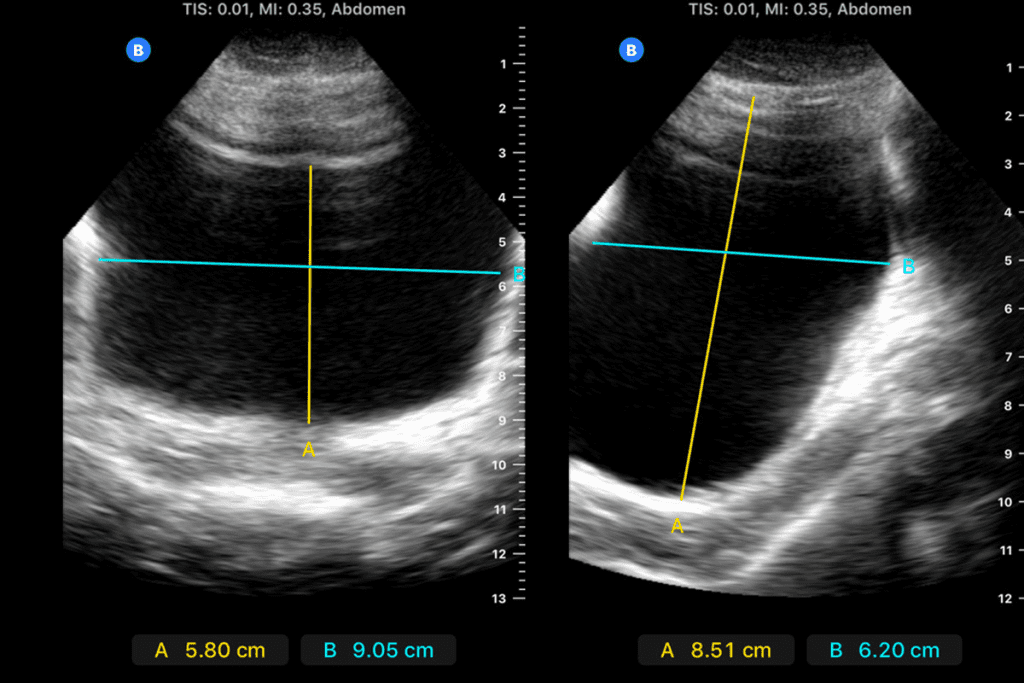
Uroflowmetry tests can spot BPH flow patterns. These patterns show a low flow rate and take longer to pee.
A study showed men with BPH pee at about 10 ml/s. This is way below normal. Spotting these patterns helps doctors diagnose BPH.
A weak pee stream might mean you have BPH. If you keep having trouble peeing, see a doctor. They can check and figure out what’s wrong.
Spotting BPH early and treating it can make symptoms better. Knowing how BPH affects pee is key to managing it well.
Urinary tract blockages can cause a lot of discomfort. Uroflowmetry is key in finding these problems. A blockage or narrowing at the bladder outlet is known as bladder outlet obstruction. This can happen for many reasons, like an enlarged prostate, urethral strictures, or bladder neck stenosis.
Many things can cause bladder outlet obstruction. Benign Prostatic Hyperplasia (BPH) is a big one in men, where a big prostate can block the urethra. Other causes include urethral strictures, which are narrowings of the urethra, and bladder neck stenosis, a narrowing of the bladder neck.
Knowing why the obstruction is happening is important for treatment. Uroflowmetry helps by measuring urine flow rate. This gives clues about the obstruction’s presence and how bad it is.
Each type of urinary obstruction has its own urine flow pattern. For example, BPH can make the peak flow rate lower and voiding time longer. Urethral strictures might make the flow pattern irregular. By looking at these patterns, doctors can understand the type of obstruction.
Uroflowmetry is a simple test that helps doctors figure out what’s going on. It guides further tests and treatment plans.
After treating bladder outlet obstruction, it’s important to keep an eye on how the patient’s urine works. Uroflowmetry is a great tool for checking if the treatment worked and if the obstruction came back.
By checking urine flow rates often, doctors can make sure the treatment is working. This helps keep the patient’s urinary health in top shape.
Neurogenic bladder is a condition where nerves affect bladder control. It can greatly change a person’s life. This happens when nerves that control the bladder get damaged, causing problems with urination.
Many neurological conditions can cause neurogenic bladder. These include spinal cord injuries, multiple sclerosis, Parkinson’s disease, and stroke. These conditions can harm the nerves that control the bladder, leading to issues like incontinence or trouble fully emptying the bladder.
Each person with these conditions experiences bladder problems differently. So, a detailed check-up is key to figuring out the exact problem and finding the right treatment.
Uroflowmetry is a key tool in diagnosing and managing neurogenic bladder. It shows signs like abnormal flow rates, interrupted flow, and low volumes. These signs can point to problems like underactive or overactive bladder muscles or blockages.
Looking at uroflow results helps us understand bladder issues better. For example, a low maximum flow rate might mean the bladder muscle isn’t working right or there’s a blockage.
Treatment for neurogenic bladder varies based on the cause, symptom severity, and overall health. Uroflowmetry results help us choose the best treatments. These might include lifestyle changes, medications, or procedures like catheterization.
For instance, if the uroflow shows the bladder muscle isn’t working well, we might suggest timed voiding or catheterization. If the muscle is too active, we might prescribe drugs to relax it.
By customizing treatment for each patient, we can improve bladder function. This helps reduce symptoms and improves life quality for those with neurogenic bladder.
It’s important to know the causes and symptoms of urethral stricture and bladder neck stenosis. These conditions narrow the urinary tract, affecting life quality.
Urethral stricture and bladder neck stenosis can come from trauma, infection, or inflammation. Symptoms include weak urine flow, straining, and not fully emptying the bladder. “The narrowing of the urethra or bladder neck can lead to obstructive urinary symptoms, significantly affecting a patient’s daily life,” as noted by urological experts.
We will look at the causes and how they lead to narrowing. Common causes include:
Knowing these causes is key to early diagnosis and treatment.
Uroflowmetry is a tool that measures urine flow rate. It helps find urethral stricture and bladder neck stenosis by spotting flow pattern issues. A low peak flow rate can show narrowing.
We use uroflowmetry to see how severe the narrowing is and to track changes. This is vital for managing these conditions well.
Surgeries aim to fix urethral stricture and bladder neck stenosis by improving urine flow. Uroflowmetry checks if the surgery worked and if the narrowing comes back.
Effective surgical outcomes mean better urine flow and fewer symptoms. Uroflowmetry gives us clear data on these results, helping us decide on further treatment if needed.
Understanding uroflowmetry’s role in diagnosing and managing these conditions helps us give better care to those affected.
Knowing how much urine you make in an hour is key to good health. It’s important for both patients and doctors to understand what a healthy flow looks like. This helps them read test results correctly.
Men and women have different flow rates because of their body differences. Men usually need to go more than 15 ml/s, while women need to go more than 20 ml/s. But age can also play a role, making older people’s flow rates lower.
When looking at test results, we must think about these factors. For example, a 70-year-old man might have a flow rate of 10 ml/s. But that’s okay for his age.
Many things can change how much urine you make. Drinking water, having diabetes, or taking certain medicines can all affect it. For example, diuretics make you pee more, while alpha-blockers help you pee better by relaxing muscles.
Key factors influencing urination output include:
The way you’re tested can change the results. Things like privacy, comfort, and a full bladder can all matter. It’s important to follow instructions before the test to get accurate results.
Doctors should also make sure patients are comfortable and private during the test. This makes the test more accurate and helps patients feel less stressed.
The detrusor muscle is key to urination. Its problems can cause many urinary issues. These issues affect the bladder’s muscular layer, which is needed for urine release.
Detrusor underactivity means the muscle is too weak. This leads to not fully emptying the bladder. Detrusor overactivity, on the other hand, makes the muscle contract too much. This causes urgency and a need to pee often.
Uroflowmetry measures urine flow to check the muscle’s work. A weak pee stream or low flow rate shows detrusor underactivity. Key uroflow signatures of weak bladder muscles include:
It’s important to tell the muscle problems from blockages. Uroflowmetry and other tests help figure this out. Clinical evaluation and urodynamic studies are key to making this distinction.
Uroflowmetry is more than just for finding blockages. It’s key in spotting many other urological issues. This test gives us a close look at how the urinary system works. It helps us find a variety of health problems.
Uroflowmetry can spot bladder tumors or prostate cancer by noticing changes in urine flow. For example, a tumor or a big prostate can block urine flow. This leads to changes that uroflowmetry can pick up.
“Abnormal uroflow patterns can be an early sign of serious issues like bladder tumors or prostate cancer,” says experts. This makes uroflowmetry a vital tool for early detection.
We use uroflowmetry to check for these conditions early on. By looking at flow rate and volume, doctors can decide if more tests are needed.
Diabetes can mess with the bladder, causing problems with storing and releasing urine. Uroflowmetry helps see how diabetes affects the bladder by measuring flow rates and patterns.
People with diabetes-related bladder issues often have specific flow patterns. These might include a slower flow or stops and starts. Finding these patterns helps us manage the condition better.
Uroflowmetry is also great for finding and treating urinary incontinence and an overactive bladder. These issues cause sudden leaks or a strong urge to pee.
Looking at uroflowmetry results helps us figure out what’s causing these symptoms. For example, an overactive bladder might show fast flow with lots of stops. Urinary incontinence might show leaks during the test.
Recurring cystitis and UTIs can change urine flow due to bladder and urethral irritation. Uroflowmetry can spot these changes, helping us diagnose and treat these infections.
People with recurring cystitis might have different flow patterns because of the infection. By watching these changes, we can make treatment plans that really work.
In short, uroflowmetry is a key tool for finding many urological problems, not just blockages. It’s non-invasive and gives quick results. This makes it a big help in urology care.
Uroflow testing is key in diagnosing urological issues. It helps doctors check urinary health and spot problems early. This includes finding issues like urinary blockages and bladder problems.
These tests guide how we treat different urological conditions.
Uroflow testing improves patient care and health. It’s a vital tool in urology. It helps us give better care and support to those with urological issues, making their lives better.
A uroflow test, also known as uroflowmetry, is a non-invasive tool. It measures how fast urine flows out. This helps doctors understand how well the bladder empties, giving insights into urinary health.
A healthy adult usually makes 40-80 mL of urine per hour. This adds up to 800-2000 mL a day. But this can change based on how much you drink, your health, and other factors.
Uroflowmetry helps spot BPH by looking at urine flow rates and patterns. Men with BPH might have a weak or broken urine stream. This can be seen with uroflowmetry, helping doctors diagnose and understand how severe it is.
Neurogenic bladder, caused by nerve problems, shows up in uroflowmetry tests. It might have irregular flow rates, broken streams, or not empty fully. These signs help doctors diagnose and plan treatment.
Uroflowmetry spots urethral stricture and bladder neck stenosis by looking at urine flow rates and patterns. These conditions narrow the urinary tract, changing the flow curve in a way that can be seen.
Many things can change how much urine you make, like how much you drink, your age, sex, health, and some medicines. Knowing these can help doctors understand uroflow test results better.
Problems with the detrusor muscle, like it being too weak or too strong, can really affect urine flow. A weak muscle might make urine flow slowly or for a long time. A strong muscle might make you need to urinate often or urgently.
Uroflowmetry isn’t a main tool for finding bladder tumors or prostate cancer. But it can hint at problems. If the flow is off, it might mean there’s something wrong that needs looking into.
To get ready for a uroflow test, come with a bladder that’s not too full or too empty. Don’t drink caffeine or other things that make you pee a lot before the test. Follow any special instructions from your doctor to get the best results.
Uroflow testing is key in finding and treating many urinary problems. It gives doctors important information about how well you’re urinating. This helps them decide on the best treatment and check if it’s working.
American Urological Association. (n.d.). Urodynamics. Retrieved from https://www.urologyhealth.org/urologic-conditions/urodynamics
Subscribe to our e-newsletter to stay informed about the latest innovations in the world of health and exclusive offers!