Last Updated on December 2, 2025 by Bilal Hasdemir
Discover why a urologist recommends cystoscopy and what patients must know before undergoing it.
We know how vital accurate diagnosis and treatment are. Cystoscopy is key for doctors to check the bladder’s lining and the urethra. This is the tube that carries urine out of the body.
A urologist does a cystoscopy mainly to find and treat urinary tract problems. This includes infections and cancers, often before symptoms get worse.
With cystoscopy, we aim to give top-notch healthcare. We offer full support and guidance to our patients. This ensures they get the best care possible.
Key Takeaways
- Cystoscopy is a diagnostic procedure used to examine the bladder and urethra.
- Urologists use cystoscopy to diagnose and manage urinary tract conditions.
- Cystoscopy helps detect infections and cancers early, often before symptoms become serious.
- Accurate diagnosis through cystoscopy enables effective treatment.
- Comprehensive patient support is key in delivering world-class healthcare.
Understanding Cystoscopy: The Essential Diagnostic Procedure
Cystoscopy is a key tool for doctors to check the bladder and urethra. It helps find and treat problems in these areas. We use the latest technology for accurate and effective care.
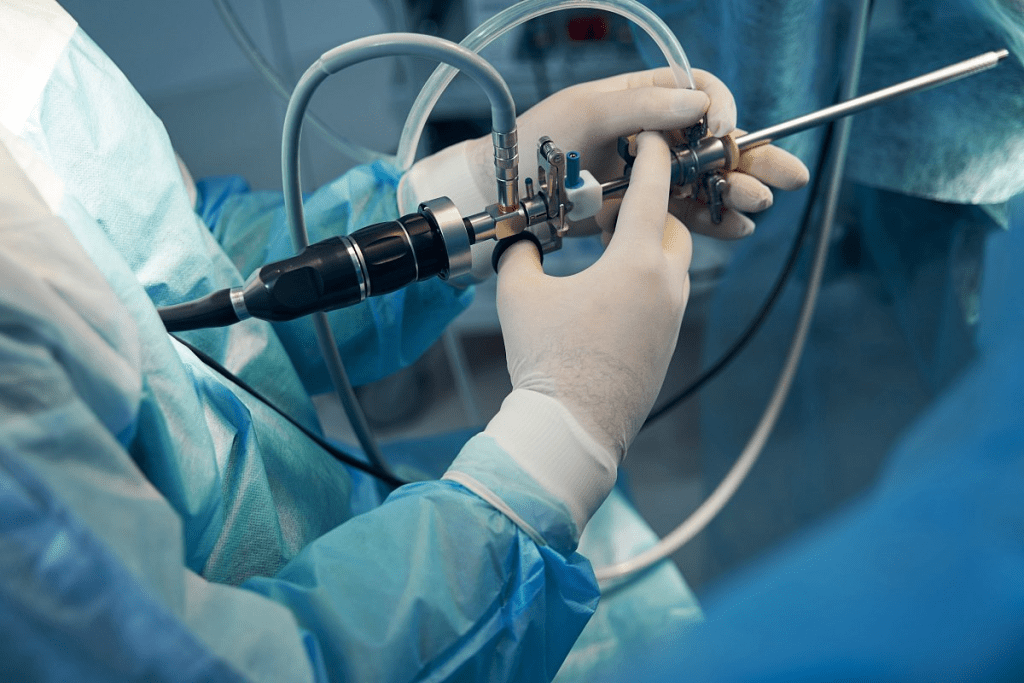
What Happens During a Cystoscopy Examination
A cystoscopy procedure lets a doctor see inside the urethra and bladder. A special camera in the cystoscope shows images on a screen. This helps spot any issues.
Doctors might also use small tools through the cystoscope. These tools can take samples or fix problems. The whole thing is done with local anesthesia to make it less painful. It usually takes about 30 minutes, and most people can go back to their day right after.
Flexible vs. Rigid Cystoscopes: Tools of the Trade
We have two kinds of cystoscopes: flexible and rigid. Flexible cystoscopes are easier on patients and let us see more details. They’re great for regular checks or for people with certain conditions.
Rigid cystoscopes give a clearer view and are better for complex tasks or taking samples. The choice depends on what the patient needs and what we’re trying to do. Our doctors are experts at using both for the best results.
When a Urologist Recommends Cystoscopy for Urinary Tract Infections
For those dealing with repeated urinary tract infections, a urologist might suggest a cystoscopy. This test looks at the bladder and urethra. It’s key for finding the cause of recurring UTIs, which affect many people.
Evaluating Recurrent UTIs
Recurring UTIs are a big problem, affecting many patients. They are the reason for up to 36% of cystoscopy cases. Our urologists use cystoscopy to check the urinary tract for problems.
They look for things like bladder stones or tumors. This helps find the cause of the infections.
Cystoscopy helps in several ways:
- Identifying the source of recurrent infections
- Detecting any abnormalities or blockages
- Guiding treatment decisions based on the findings
Identifying Structural Abnormalities Contributing to Infection
Structural problems in the urinary tract can lead to UTIs. These might include bladder diverticula or urethral strictures. Our urologists can see these issues during a cystoscopy.
Understanding the cause of recurring UTIs helps us create a better treatment plan. This might include fixing structural problems or managing other conditions. It also helps prevent future infections.
Investigating Blood in Urine: A Primary Reason for Cystoscopy
Cystoscopy is key in finding out why there’s blood in urine, known as hematuria. This can mean different things, from simple issues to serious ones like bladder cancer. Our urologists use cystoscopy to check it out carefully.
Hematuria in Urology Consultations
About 20% of urology visits are because of hematuria. This means blood in urine is a big deal for both doctors and patients. Our doctors work hard to find out why it happens so they can treat it right.
Differentiating Between Benign and Serious Causes
Cystoscopy is vital for looking at hematuria. It lets our doctors see inside the bladder and urethra. This helps tell if it’s something simple or something serious like cancer.
With a borescope or cystoscope, doctors can spot problems like tumors or stones. This is key for making a treatment plan that fits the patient’s needs.
In some cases, uro pills might be given to ease symptoms like pain. But finding the real cause of hematuria is the first step to the best treatment.
Bladder Cancer Detection and Surveillance Through Cystoscopy
Cystoscopy is key in finding and managing bladder cancer, a common urological cancer. It lets us see inside the bladder. This helps us spot tumors and other issues early.
Bladder cancer is a big health issue. Finding it early is vital for good treatment. Cystoscopy helps us find bladder tumors early. This improves how well patients do.
Early Detection Protocols and Improved Survival Rates
We stick to set plans for finding bladder cancer early with cystoscopy. We use a cystoscope to check the bladder lining. This helps us spot any odd spots.
Early detection is key to better survival rates for bladder cancer patients. Finding tumors early lets us start treatment fast. This lowers the chance of cancer getting worse.
Follow-up Schedules After Bladder Cancer Treatment
After treating bladder cancer, we suggest regular cystoscopy checks to watch for signs of it coming back. How often these checks are needed depends on the patient’s risk and how well they did in treatment.
- High-risk patients need more checks, usually every 3-6 months.
- Low-risk patients might need checks less often, every 6-12 months.
Regular cystoscopy checks help us catch any signs of cancer coming back early. This lets us act fast and improve patient results.
Cost-Effectiveness and Advantages of Office-Based Cystoscopy
Office-based cystoscopy is becoming a top choice for checking urinary tract problems. It’s cheaper and safer than traditional methods because it doesn’t need anesthesia.
Outpatient vs. Inpatient Procedures: Saving Over €1,200 Per Case
Office-based cystoscopy saves a lot of money, over €1,200 per case. This is because it doesn’t require a hospital stay. It’s also quicker and more efficient.
- Reduced hospital stay costs
- Lower anesthesia costs due to the use of local anesthesia
- Efficient use of resources, minimizing unnecessary expenditures
This method makes healthcare cheaper for patients and hospitals. It also makes patients happier because it’s less scary and more comfortable.
Reduced Anesthesia Risks for Older Patients
Office-based cystoscopy is safer for older patients because it uses local anesthesia. General anesthesia, used in hospitals, can be risky. Local anesthesia is safer and lets patients recover faster.
The benefits for older patients are clear:
- Lower risk of respiratory complications
- Faster recovery times, enabling patients to resume normal activities sooner
- Reduced need for post-procedure monitoring, further streamlining care
Office-based cystoscopy is a safer and more efficient way to diagnose problems. It’s perfect for older patients or those with health issues. As we keep improving in urology, office-based cystoscopy will become even more popular.
Conclusion: The Critical Role of Cystoscopy in Modern Urological Care
Cystoscopy is key in today’s urological care. It helps us make accurate diagnoses and treat patients well. This tool is very important for patient care and success.
We use cystoscopy to find and treat many urinary problems. This includes infections, bleeding, and bladder cancer. A urologist looks inside the bladder and urethra with a cystoscope.
This lets us see any problems and plan the best treatment. Cystoscopy helps us give our patients the best care possible.
We are dedicated to giving our patients the best care. We use cystoscopy to help diagnose and treat. Our goal is to support and guide our patients every step of the way.
FAQ
What is a cystoscopy, and why is it performed?
A cystoscopy lets a urologist see inside the bladder and urethra with a cystoscope. It helps find and treat issues like UTIs, bleeding, and bladder cancer.
What are the differences between flexible and rigid cystoscopes?
Flexible cystoscopes are more comfy and show more detail. Rigid ones give clearer images and are used for complex tasks.
What can I expect during a cystoscopy examination?
During a cystoscopy, a urologist will put a cystoscope into your urethra. They will then look at your bladder. The whole thing is done with local anesthesia to make you feel less uncomfortable.
Is cystoscopy a painful procedure?
Cystoscopy isn’t usually painful. You might feel some pressure or discomfort. But local anesthesia helps make it more comfortable.
How is cystoscopy used in the diagnosis and management of bladder cancer?
Cystoscopy is key in finding and watching bladder cancer. It lets doctors see inside the bladder for tumors. This helps in early treatment and better outcomes.
What are the benefits of office-based cystoscopy?
Office-based cystoscopy is cheaper and safer. It avoids the risks of general anesthesia and hospital stays.
How does cystoscopy help in evaluating recurrent UTIs?
Cystoscopy helps find problems like stones or tumors that cause UTIs. This way, doctors can treat them better.
What is the role of cystoscopy in investigating hematuria?
Cystoscopy helps find where blood in the urine comes from. It lets doctors see inside the bladder and urethra. This helps tell if it’s serious or not.
What is a cystogram, and how does it differ from cystoscopy?
A cystogram uses X-rays to see the bladder. Cystoscopy is a direct look inside the bladder and urethra with a cystoscope.
What is a uro pill, and is it related to cystoscopy?
Uro pills treat urinary issues. But they’re not part of cystoscopy, which is for looking inside the bladder and urethra.
What is the difference between cystoscopy and cystourethroscopy?
Cystoscopy and cystourethroscopy are often the same. But cystourethroscopy means looking at both the bladder and urethra with a cystoscope.
References:
- Matulewicz, R. S., et al. (2017). Cystoscopy. JAMA, 317(11), 1187. https://jamanetwork.com/journals/jama/fullarticle/2612619
- Guldhammer, C. S., et al. (2023). Cystoscopy Accuracy in Detecting Bladder Tumors. PMC (PubMed Central). https://pmc.ncbi.nlm.nih.gov/articles/PMC10777997/
- Shore, N. D., et al. (2023). Clinical and economic impact of blue light cystoscopy in non-muscle invasive bladder cancer. European Urology. https://www.sciencedirect.com/science/article/abs/pii/S1078143922004756





