Urinary incontinence affects more than 60% of adult women in the United States. It greatly impacts their quality of life and daily activities leaking urine women.
It is the accidental release of urine. This often happens when coughing, laughing, sneezing, or doing physical activities.
At Liv Hospital, we know urinary incontinence is not normal as we age. There are many treatment options. We offer patient-centered care to help women manage this condition well.
Key Takeaways
- Urinary incontinence is a common condition affecting millions of women worldwide.
- It is not a normal part of aging, and various treatment options are available.
- Liv Hospital offers comprehensive care for managing urinary incontinence.
- Effective management can significantly improve quality of life.
- Seeking medical attention is the first step towards managing the condition.
Understanding Leaking Urine in Women: An Overview
It’s important to understand leaking urine in women to help them better. Urinary incontinence, or the loss of bladder control, affects millions. It doesn’t matter if you’re young or old, from any background, or have any lifestyle.
What is Urinary Incontinence?
Urinary incontinence means losing bladder control and leaking urine. It’s not a disease but a sign of a problem. This problem could be weak pelvic muscles or a neurological disorder. There are different types, like stress incontinence and urge incontinence.
Prevalence and Impact on Quality of Life
About 32.4 percent of women deal with urinary incontinence every month. It really affects their lives, making daily tasks hard. It also makes them feel embarrassed and isolated.
Why Women Are More Susceptible Than Men
Women are more likely to have urinary incontinence because of pregnancy and childbirth. These events can weaken the pelvic floor muscles. Menopause also plays a role, as estrogen levels drop.
Knowing about urinary incontinence helps us support women more. There are many ways to manage it, from simple changes to medical treatments. We can make a difference by being understanding and helpful.
Types of Urinary Incontinence in Women

It’s important to know the different types of urinary incontinence. This is because each type has its own causes and symptoms. Understanding this helps in finding the right treatment.
Stress Incontinence
Stress incontinence is common in younger women. It happens when urine leaks out during activities that put pressure on the belly. This can be due to weak pelvic muscles or problems with the urethral sphincter.
Urge Incontinence (Overactive Bladder)
Urge incontinence, or overactive bladder, is when you suddenly need to pee and can’t hold it. Women with this might pee a lot or wake up to pee at night. It can be caused by many things, like infections or certain medicines.
Mixed Incontinence
Mixed incontinence is when you have symptoms of both stress and urge incontinence. This makes it harder to diagnose and treat. It needs a detailed plan to handle both stress and urge incontinence.
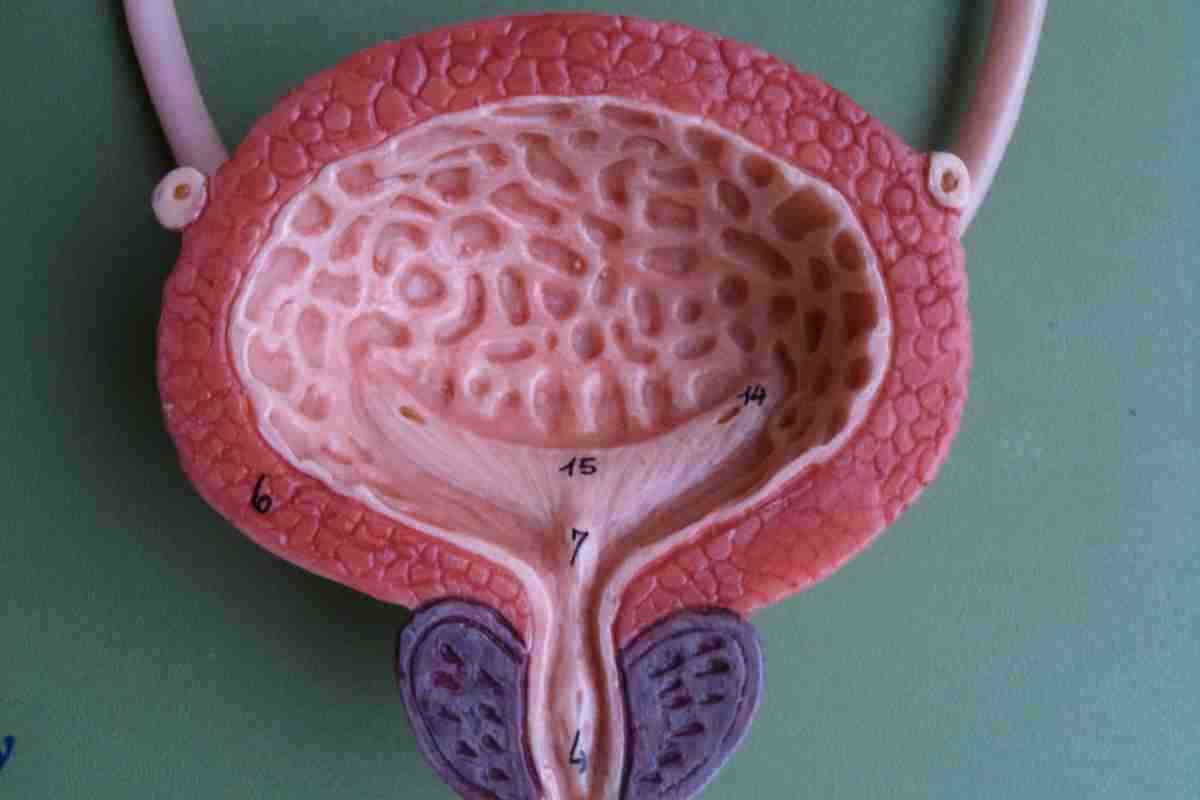
Overflow Incontinence
Overflow incontinence happens when the bladder doesn’t empty fully. This leads to constant or frequent leaking of urine. It’s often linked to diabetes, nerve problems, or blockages in the urinary tract. Treatment aims to fix the cause and help the bladder empty better.
Knowing the exact type of urinary incontinence is key to choosing the right treatment. We’ll look at these options in more detail next.
Common Causes and Risk Factors
Understanding urinary incontinence is key to managing it. It affects women in many ways, from physical changes to lifestyle and medical issues. We’ll dive into these factors to help you understand it better.
Age-Related Changes
Women’s bodies change with age, affecting bladder control. Age-related changes include weaker pelvic muscles and less flexible bladders. These can lead to incontinence.
Pregnancy and Childbirth Effects
Pregnancy and childbirth can harm the pelvic floor muscles and bladder control. The growing uterus can press on the bladder. Childbirth can damage the muscles and nerves around the bladder. This can cause stress urinary incontinence.
Menopause and Hormonal Changes
Menopause brings big hormonal changes, like lower estrogen levels. This can affect the urinary tract, causing incontinence symptoms. Topical estrogen therapy might help with these symptoms.
Medical Conditions Contributing to Incontinence
Some medical conditions raise the risk of incontinence. These include diabetes, neurological disorders, and mobility issues. Managing these conditions well is key to preventing or reducing incontinence.
Diagnosing Urinary Incontinence
To tackle urinary incontinence, doctors must first find its cause. This involves several steps and tests. These help figure out how severe and what type it is.
When to See a Healthcare Provider
If you’re dealing with ongoing or bad symptoms, see a doctor. You should go if you:
- Leak urine often or more than before
- See changes in how you pee
- Have trouble starting or stopping pee
- Feel the need to pee urgently or a lot
What to Expect During Evaluation
At your first visit, we’ll look at your medical history and do a physical check. This might include:
- Filling out a form about your symptoms and health
- A physical exam, like a pelvic check
- Checking your overall health and any health issues
Diagnostic Tests and Procedures
We might suggest tests to find out why you have urinary incontinence. These could be:
- Urinalysis to check for infections or other issues
- Urodynamic tests to see how your bladder works
- Post-void residual measurement to check for urine left behind
- Cystoscopy to look inside your bladder
These tests help us find the best treatment for you.
Keeping a Bladder Diary
A bladder diary is a helpful tool. It tracks your fluid intake, pee patterns, and any leaks. This helps us understand your bladder habits better.
To keep a bladder diary, note:
- When and how much fluid you drink
- When and how much pee you void
- Any leaks, including what was happening
With your diary and test results, we can make a detailed plan for you.
Lifestyle Modifications to Manage Leaking Urine in Women
Simple changes can greatly improve life for women with urinary incontinence. By making a few adjustments, women can manage their symptoms better. This helps them regain control over their bladder.
Weight Management Strategies
Keeping a healthy weight is key for managing urinary incontinence. Extra weight can put more pressure on the bladder and pelvic muscles. This makes symptoms worse. We suggest a balanced diet and regular exercise to keep a healthy weight.
- Healthy Eating: Eat a variety of fruits, vegetables, whole grains, and lean proteins.
- Regular Exercise: Find activities you like, like walking, swimming, or cycling, to burn calories and strengthen muscles.
Studies show that losing weight can greatly reduce urinary incontinence episodes. This highlights the role of weight management in incontinence care.
Dietary Changes to Reduce Symptoms
Changing what you eat can help manage urinary incontinence. Some foods and drinks can irritate the bladder, while others can help.
- Avoid Irritants: Cut down or avoid caffeine, alcohol, spicy, and acidic foods that can irritate the bladder.
- Incorporate Beneficial Foods: Eat more foods high in fiber, like whole grains and vegetables, to prevent constipation and reduce incontinence.
“Dietary changes can significantly impact the management of urinary incontinence. By making informed choices, women can reduce their symptoms and improve their quality of life.”
Fluid Management Techniques
Controlling how much you drink is important for managing urinary incontinence. It might seem odd, but drinking too little can make urine more concentrated. This can irritate the bladder.
- Monitor Fluid Intake: Keep track of your fluid intake to find patterns and irritants.
- Spread Out Fluid Consumption: Drink fluids throughout the day instead of all at once.
Smoking Cessation Benefits
Quitting smoking is good for your health and can help with urinary incontinence. Smoking can cause chronic coughing, which strains the pelvic floor muscles.
By quitting, women can lower their risk of urinary incontinence. There are many resources and support groups for quitting smoking.
We encourage women to try these lifestyle changes to manage leaking urine. Making these adjustments can help women regain control and improve their overall well-being.
Pelvic Floor Exercises and Physical Therapy
Managing urinary incontinence requires a mix of methods. This includes pelvic floor exercises, bladder training, and changes in lifestyle. We suggest starting with pelvic floor exercises like Kegel training. These exercises help strengthen the muscles that control the bladder.
Strengthening Pelvic Floor Muscles
Kegel exercises are key for pelvic floor muscle training. They help women control their bladder better and lessen incontinence symptoms. We teach patients how to do Kegel exercises correctly to get the most benefit.
Bladder Training Techniques
Bladder training helps manage urinary incontinence. It involves scheduled bathroom visits and waiting longer to go. This increases bladder capacity and cuts down on leaks. We help track progress and adjust plans as needed for the best results.
Comprehensive Management Strategies
Managing urinary incontinence also means using absorbent products and protective underwear. Choosing the right clothes and finding ways to handle work and social situations are important too. We discuss medical treatments like medications and surgery to offer a full solution.
By using these methods together, women can manage urinary incontinence well. We create a plan that fits each patient’s needs to improve bladder health.
FAQ
What is urinary incontinence, and how common is it in women?
Urinary incontinence means you can’t control when you pee. It’s very common, affecting over 60% of women in the U.S.
What are the different types of urinary incontinence that affect women?
There are a few types. Stress incontinence happens when you pee during activity. Urge incontinence is when you pee suddenly. Mixed incontinence is a mix of both. Overflow incontinence is when your bladder is always full.
What are the common causes and risk factors associated with urinary incontinence in women?
Getting older, pregnancy, childbirth, and menopause can cause it. Some medical conditions also play a role.
How is urinary incontinence diagnosed?
Doctors use tests and a bladder diary to diagnose it. This diary helps track your pee habits.
What lifestyle modifications can help manage urinary incontinence?
Losing weight, eating right, managing fluids, and quitting smoking can help. These changes can ease symptoms.
How can pelvic floor exercises help with urinary incontinence?
Exercises like Kegels strengthen the muscles around your bladder. This can help control your pee.
What is bladder training, and how can it help?
Bladder training means going to the bathroom at set times. It helps you hold your pee longer. Delayed voiding and double voiding are also part of it.
What are the benefits of working with a pelvic floor physical therapist?
A physical therapist can create a workout plan for you. This plan strengthens your pelvic floor muscles and improves bladder control.
What medical treatments are available for managing urinary incontinence?
Doctors can prescribe medications or use Botox injections. Topical estrogen and pessaries are also options.
What surgical options are available for urinary incontinence?
Surgery includes sling procedures and bladder neck suspension. Prolapse surgery and sacral nerve stimulation are also options for those who don’t respond to other treatments.
How can women manage urinary incontinence in daily life?
Using absorbent products and choosing the right clothes can help. Strategies for work and social situations also help manage it.
Are there any travel tips for women with urinary incontinence?
Plan ahead, pack essentials, and know where restrooms are. These tips help manage incontinence while traveling.
Can women with urinary incontinence lead active lives?
Yes, with the right management and treatments, women can live active and fulfilling lives.
References
National Center for Biotechnology Information. Evidence-Based Medical Guidance. Retrieved from https://pubmed.ncbi.nlm.nih.gov/35030139/