Getting a positive P-ANCA test result can be scary. It makes people wonder about their health. At Liv Hospital, we make sure to explain things clearly. This helps patients understand complex medical info.p anca positiveUric Stones Treatment: Prevention & Relief Tips
Anti-neutrophil cytoplasmic antibodies (ANCA) are autoantibodies that attack neutrophils. Neutrophils are white blood cells that fight infections. The presence of these antibodies is linked to certain autoimmune diseases and inflammation.
A positive P-ANCA test means you have perinuclear anti-neutrophil cytoplasmic antibodies. This can help doctors diagnose and treat you. It’s important for both patients and doctors to understand what this test means.
Anti-Neutrophil Cytoplasmic Antibodies (ANCA) in the blood can signal certain autoimmune diseases. To grasp ANCA’s importance, we need to know what they are and their role in our immune system.
Neutrophils are a key type of white blood cell. They are vital for our immune defense. They fight infections by engulfing and destroying harmful particles.
Their cytoplasm has enzymes and antimicrobial peptides. These are essential for their job.
ANCA are autoantibodies against neutrophil proteins. There are two main types: Perinuclear ANCA (P-ANCA) and Cytoplasmic ANCA (C-ANCA). P-ANCA is linked to myeloperoxidase (MPO) antibodies. C-ANCA is associated with proteinase 3 (PR3) antibodies.
Knowing the differences between these types is key for diagnosing and treating ANCA-associated vasculitides.
ANCA were first found in the 1980s in patients with certain vasculitis types. Now, ANCA testing helps diagnose and monitor autoimmune diseases, like ANCA-associated vasculitides. This shows how far we’ve come in understanding these autoantibodies.
Knowing about ANCA, including neutrophils and ANCA types, helps us see the importance of a positive P-ANCA test. It’s vital for patient care.
It’s important to know the difference between P-ANCA and C-ANCA for the right diagnosis and treatment. These two types of Anti-Neutrophil Cytoplasmic Antibodies are linked to different diseases and symptoms.
P-ANCA shows a perinuclear staining pattern, mainly targeting myeloperoxidase (MPO). It’s often seen in microscopic polyangiitis (MPA) and eosinophilic granulomatosis with polyangiitis (EGPA). P-ANCA is a key marker for some vasculitis and autoimmune diseases.
C-ANCA has a cytoplasmic staining pattern, mainly linked to antibodies against proteinase 3 (PR3). It’s commonly found in granulomatosis with polyangiitis (GPA), a condition with granulomatous inflammation and vasculitis. The C-ANCA test is key for diagnosing GPA and tracking its activity.
“The difference between P-ANCA and C-ANCA is not just for lab curiosity. It’s very important for diagnosis, treatment, and patient care.”
P-ANCA and C-ANCA have different meanings in medicine. They are linked to different diseases and their outcomes. Knowing these differences helps doctors create better treatment plans for their patients. For example, P-ANCA might suggest certain autoimmune diseases, while C-ANCA is more related to GPA.
Key differences between P-ANCA and C-ANCA include:
Understanding P-ANCA and C-ANCA helps healthcare providers make better decisions. This leads to better care and outcomes for patients.
A positive P-ANCA test usually means you have myeloperoxidase (MPO) antibodies. These are a type of anti-neutrophil cytoplasmic antibody. They are linked to certain autoimmune diseases that cause inflammation and damage in the body.
Myeloperoxidase antibodies are important in understanding P-ANCA positivity. About 90 percent of samples with a perinuclear pattern contain MPO antibodies. These antibodies target myeloperoxidase, an enzyme in neutrophils, a key white blood cell for fighting infections.
The presence of MPO antibodies is often seen in autoimmune disorders. These disorders affect blood vessels and cause vasculitis.
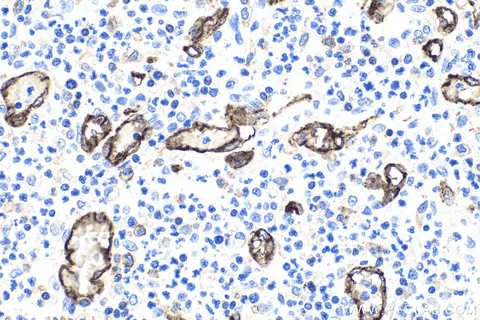
The perinuclear staining pattern is seen in the indirect immunofluorescence assay for ANCA. It is a key sign of P-ANCA positivity. The perinuclear staining happens because the antibodies bind to the antigens around the nucleus of neutrophils.
This creates a distinctive pattern under the microscope. It’s a critical clue for diagnosing P-ANCA from C-ANCA.
The production of P-ANCA is tied to complex autoimmune mechanisms. In autoimmune diseases, the immune system attacks its own tissues. This leads to inflammation and damage.
The presence of P-ANCA suggests an autoimmune process. This process may involve genetics and environmental triggers. Understanding these mechanisms is key for diagnosing and managing P-ANCA-related conditions.
Understanding ANCA testing is key to grasping its importance. It’s a vital tool for spotting anti-neutrophil cytoplasmic antibodies. These antibodies are linked to several autoimmune diseases.
Indirect immunofluorescence testing (IIF) is a main method for finding ANCAs. It works by fixing neutrophils on a slide and then exposing them to the patient’s serum. If ANCAs are there, they’ll stick to the neutrophils.
A fluorescent dye is then used to show where the ANCAs are. This is done under a special microscope.
IIF helps identify the type of ANCA by looking at its staining pattern. This can be either cytoplasmic (C-ANCA) or perinuclear (P-ANCA). Knowing this is important for diagnosis.
ELISA is another important way to find ANCAs. It looks for specific antigens like myeloperoxidase (MPO) or proteinase 3 (PR3). This method is more precise than IIF and measures how much ANCA is in the blood.
ELISA works by coating a plate with the antigen and adding the patient’s serum. If antibodies are there, they’ll bind. Then, an enzyme-linked antibody and a color-changing substrate are added, showing a positive result.
|
Method |
Description |
Advantages |
|---|---|---|
|
Indirect Immunofluorescence Testing (IIF) |
Detects ANCAs by their staining pattern on neutrophils |
Provides information on the type of ANCA (C-ANCA or P-ANCA) |
|
Enzyme-Linked Immunosorbent Assay (ELISA) |
Quantifies specific ANCA antigens like MPO or PR3 |
High specificity and sensitivity for ANCA detection |
Understanding ANCA test results is complex. It involves knowing the patient’s symptoms and other test results. A positive test might mean an autoimmune disease like vasculitis.
“The interpretation of ANCA results should always be done in the context of the patient’s clinical presentation and other laboratory findings.” –
AACR Clinical Practice Guidelines
Healthcare providers should look at ANCA results alongside the patient’s medical history and other tests. This helps make the best care decisions.
A positive P-ANCA test may show ANCA-associated vasculitides. These are disorders that harm blood vessels. They cause inflammation, which can damage organs and systems in the body.
Vasculitis is when blood vessels get inflamed. This can cause different symptoms, depending on the affected vessels and organs. It can be caused by infections, medicines, or autoimmune diseases.
When vasculitis happens, it can weaken blood vessel walls. This can lead to problems like aneurysms or narrowed vessels. Knowing the cause of vasculitis is key to finding the right treatment.
There are several types of vasculitides linked to ANCA positivity. Each has its own symptoms and effects.
These conditions need quick diagnosis and treatment to avoid lasting harm. Treatment usually includes medicines to fight the autoimmune response and reduce inflammation.
Understanding the link between microscopic polyangiitis and P-ANCA positive results is key. Microscopic polyangiitis (MPA) is a type of vasculitis that mainly affects small blood vessels. It is closely linked to the presence of perinuclear anti-neutrophil cytoplasmic antibodies (P-ANCA).
MPA symptoms can vary a lot among patients. Common signs include kidney problems like hematuria and proteinuria. Systemic symptoms like fever and weight loss are also common.
Respiratory symptoms are common too. Some patients may have cough, hemoptysis, or dyspnea due to lung involvement.
“The clinical manifestations of MPA can be non-specific, making it challenging to diagnose based on clinical grounds alone,” as noted in medical literature. So, lab tests, including ANCA testing, are vital for diagnosis.
Diagnosing MPA requires a mix of clinical assessment, lab tests, and sometimes biopsy. The presence of P-ANCA, mainly MPO-ANCA, is a key marker. Approximately 90% of patients with MPA test positive for ANCA at diagnosis, with most having MPO-ANCA.
Treatment for MPA usually involves immunosuppressive therapy. Corticosteroids are often the first choice, sometimes with other drugs like cyclophosphamide or rituximab.
“Early and aggressive treatment is key to better outcomes in MPA patients,” clinical guidelines say. Keeping an eye on disease activity and adjusting treatment as needed is important for long-term care.
Understanding EGPA and its link to ANCA status is key for diagnosis and treatment. EGPA is a rare autoimmune disorder. It is marked by eosinophils, a type of white blood cell, and granulomatous inflammation.
EGPA goes through three phases. The first is the allergic phase, with asthma and eosinophilia. The second is the eosinophilic phase, where organs are damaged by eosinophils. The third is the vasculitic phase, with systemic vasculitis.
Common symptoms include asthma, sinusitis, skin rashes, and gastrointestinal issues. As it progresses, it can cause serious problems like cardiac issues and neuropathy.
Diagnosing EGPA is hard because it’s similar to other vasculitides and can present differently. ANCA can help diagnose, but its presence varies among patients. About 40% of EGPA patients are ANCA-positive, often with a P-ANCA pattern.
To diagnose EGPA, doctors look at clinical features, lab findings (like eosinophilia), and histological evidence of vasculitis or eosinophilic infiltration.
Managing EGPA involves several steps. Corticosteroids are used first to reduce inflammation and control symptoms. For severe cases or those not responding to corticosteroids, more immunosuppressive therapy may be needed.
Treatment goals include inducing remission, reducing relapse risk, and managing complications. ANCA status can affect treatment, with positive patients needing more aggressive therapy.
We stress the need for a personalized treatment plan. This plan should consider the patient’s clinical features, ANCA status, and disease severity.
P-ANCA antibodies are often found in people with certain inflammatory bowel diseases, like ulcerative colitis. Inflammatory bowel disease (IBD) is a group of conditions that cause long-term inflammation in the gut. Ulcerative colitis and Crohn’s disease are the most common types.
Up to 80 percent of ulcerative colitis patients test positive for P-ANCA. These antibodies are linked to certain symptoms and behaviors of the disease. P-ANCA is a key marker for diagnosing ulcerative colitis. Doctors use P-ANCA tests to tell ulcerative colitis apart from Crohn’s disease.
P-ANCA is less common in Crohn’s disease. But when it is present, it might suggest a certain type of Crohn’s disease similar to ulcerative colitis. The exact role of P-ANCA in Crohn’s disease needs more study.
Diagnosing IBD is complex and involves several tests. P-ANCA testing is a helpful tool in this process. It’s important to tell ulcerative colitis and Crohn’s disease apart to choose the right treatment.
|
Disease Characteristics |
Ulcerative Colitis |
Crohn’s Disease |
|---|---|---|
|
P-ANCA Positivity |
High prevalence (up to 80%) |
Less common |
|
Disease Location |
Typically limited to the colon |
Can affect any part of the GI tract |
In conclusion, P-ANCA positive results are very important in inflammatory bowel disease, mainly in ulcerative colitis. Knowing about P-ANCA helps doctors diagnose and manage the disease better. This leads to better care for patients.
P-ANCA positivity is not just linked to vasculitides. It’s also connected to other health issues. Let’s dive into these conditions and what they mean.
Autoimmune hepatitis is when the immune system attacks the liver. P-ANCA positivity is common in patients with this condition. This suggests a connection between the disease’s autoimmune causes and the presence of these antibodies.
Primary sclerosing cholangitis (PSC) is a chronic liver disease. It causes inflammation and scarring of the bile ducts. P-ANCA is often found in PSC patients. It’s seen as a diagnostic marker, but it’s not exclusive to this disease.
Rheumatoid arthritis (RA) mainly affects the joints. While P-ANCA is less common in RA, some patients may test positive. This is more likely in those with severe disease or other symptoms outside the joints.
Some medications can cause ANCA production, leading to P-ANCA positivity. This is seen in drugs for treating infections and autoimmune diseases. The importance of drug-induced ANCA positivity needs careful evaluation.
|
Condition |
P-ANCA Positivity Rate |
Clinical Significance |
|---|---|---|
|
Autoimmune Hepatitis |
30-80% |
Diagnostic marker, indicates autoimmune activity |
|
Primary Sclerosing Cholangitis |
60-80% |
Diagnostic aid, associated with disease activity |
|
Rheumatoid Arthritis |
5-20% |
May indicate more severe disease or extra-articular involvement |
|
Drug-Induced |
Varies |
Depends on the drug and clinical context |
P-ANCA positivity is a challenge in clinical practice. It requires careful evaluation and management. A thorough approach is needed, including initial evaluation, follow-up testing, treatment, and monitoring disease activity.
When a patient tests positive for P-ANCA, a detailed medical history and physical exam are key. We look for signs of vasculitis or other conditions. We also review lab results, including P-ANCA levels and other autoantibodies.
Follow-up tests are vital to confirm the diagnosis and assess disease extent. We may run more lab tests, like complete blood counts and inflammatory markers. Imaging studies help check for organ involvement.
Treatment for P-ANCA-positive patients depends on the diagnosis and disease severity. Immunosuppressive therapy is often needed to manage vasculitis and prevent damage. We consider the patient’s health and treatment risks carefully.
Monitoring disease activity is key to adjusting treatment and preventing flare-ups. Regular clinical checks, lab tests, and imaging studies are part of this process.
Here’s a summary of managing P-ANCA-positive patients:
|
Management Component |
Description |
Key Considerations |
|---|---|---|
|
Initial Evaluation |
Thorough medical history and physical examination |
Identify signs of vasculitis or other conditions |
|
Follow-up Testing |
Laboratory tests and imaging studies |
Assess disease extent and organ involvement |
|
Treatment Considerations |
Immunosuppressive therapy based on diagnosis and disease severity |
Weigh benefits and risks, consider patient health and side effects |
|
Monitoring Disease Activity |
Regular clinical assessments and laboratory tests |
Adjust treatment plans, prevent disease flare-ups |
P-ANCA testing is key in diagnosing and managing autoimmune diseases. It greatly impacts patient care in today’s medicine. The ANCA Profile Test helps diagnose and manage autoimmune vasculitis and other related conditions.
It’s important for healthcare providers to understand what a p ANCA positive result means. This knowledge helps them make better treatment choices. ANCA testing has changed how we diagnose and treat autoimmune disorders. It leads to better therapies and outcomes for patients.
In today’s medicine, P-ANCA testing is vital for accurate diagnoses and treatment plans. As we learn more about autoimmune diseases, ANCA testing will keep being essential. It helps ensure high-quality care for patients.
P-ANCA and C-ANCA are two types of ANCA. They show different patterns when stained on neutrophils. P-ANCA is linked to myeloperoxidase (MPO) antibodies. C-ANCA is linked to proteinase 3 (PR3) antibodies.
A positive P-ANCA test means you have antibodies against the neutrophil’s cytoplasm. This is often seen in autoimmune diseases like vasculitis, inflammatory bowel disease, or autoimmune hepatitis.
MPO antibodies are common in P-ANCA positivity. They target myeloperoxidase in neutrophils. This is often linked to microscopic polyangiitis.
ANCA testing uses indirect immunofluorescence testing (IIF) or enzyme-linked immunosorbent assay (ELISA). IIF stains neutrophils with patient serum. ELISA measures specific ANCA antibodies.
Being P-ANCA positive can mean you have conditions like microscopic polyangiitis, inflammatory bowel disease, or autoimmune hepatitis. The impact depends on the condition and its severity.
Yes, P-ANCA positivity can also be seen in inflammatory bowel disease, autoimmune hepatitis, primary sclerosing cholangitis, and rheumatoid arthritis.
Managing P-ANCA-associated vasculitis involves immunosuppressive therapy. This helps control inflammation and prevent damage. Treatment varies based on the condition and its severity.
P-ANCA testing helps diagnose and differentiate inflammatory bowel disease. It’s useful in telling ulcerative colitis apart from Crohn’s disease.
Yes, some medications can cause P-ANCA positivity. This is often seen in drug-induced lupus or vasculitis-like syndromes.
Patients with positive P-ANCA tests need regular check-ups. This is to monitor disease activity, adjust treatment, and manage complications.
National Center for Biotechnology Information. Positive P-ANCA Test: Understanding Anti-Neutrophil Cytoplasmic Antibodies. Retrieved
from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC10253038/
Subscribe to our e-newsletter to stay informed about the latest innovations in the world of health and exclusive offers!