Last Updated on November 26, 2025 by Bilal Hasdemir
Vertebral compression fractures can cause sudden, severe pain and limit your mobility. At Liv Hospital, we take a personalized approach to treat and relieve your pain. We combine medical expertise with empathy to manage these fractures.
We help you find the most advanced, evidence-based vertebral compression fracture treatment for quick and lasting recovery. Our patient-centered care means we tailor your care to fit your needs perfectly.
Managing vertebral compression fractures requires a variety of strategies. From conservative care to advanced interventions, understanding these options is key. It helps you make informed decisions about your care.
Key Takeaways
- Personalized treatment plans are essential for managing vertebral compression fractures.
- A mix of conservative and advanced approaches may be used.
- Pain relief is a critical part of effective management.
- Advanced, evidence-based treatments can lead to quick and lasting recovery.
- Patient-centered care ensures you get the support you need throughout treatment.
Understanding Vertebral Compression Fractures
We will look into what causes vertebral compression fractures and who is at risk. These fractures are a big worry for older adults and people with certain health issues.
Common Causes and Risk Factors
Vertebral compression fractures often happen because of osteoporosis. This is when bones get weak and break easily. They can also be caused by injuries to the spine or diseases like cancer.
Here are some risk factors for these fractures:
- Advanced age
- Osteoporosis
- Previous fractures
- Steroid use
- Low body mass index (BMI)
| Risk Factor | Description |
| Osteoporosis | A condition that weakens bones |
| Advanced Age | Increased risk with age |
| Previous Fractures | History of fractures increases risk |
Signs and Symptoms to Recognize
It’s important to know the signs of vertebral compression fractures. This helps in getting early treatment. Common symptoms include:
- Back pain
- Loss of height
- Stooped posture or kyphosis
- Decreased mobility
The pain from these fractures can be mild or very bad. It can get worse if not treated. If you have these symptoms, see a doctor right away.
Knowing about vertebral compression fractures helps prevent them. It also helps find the right treatment when needed.
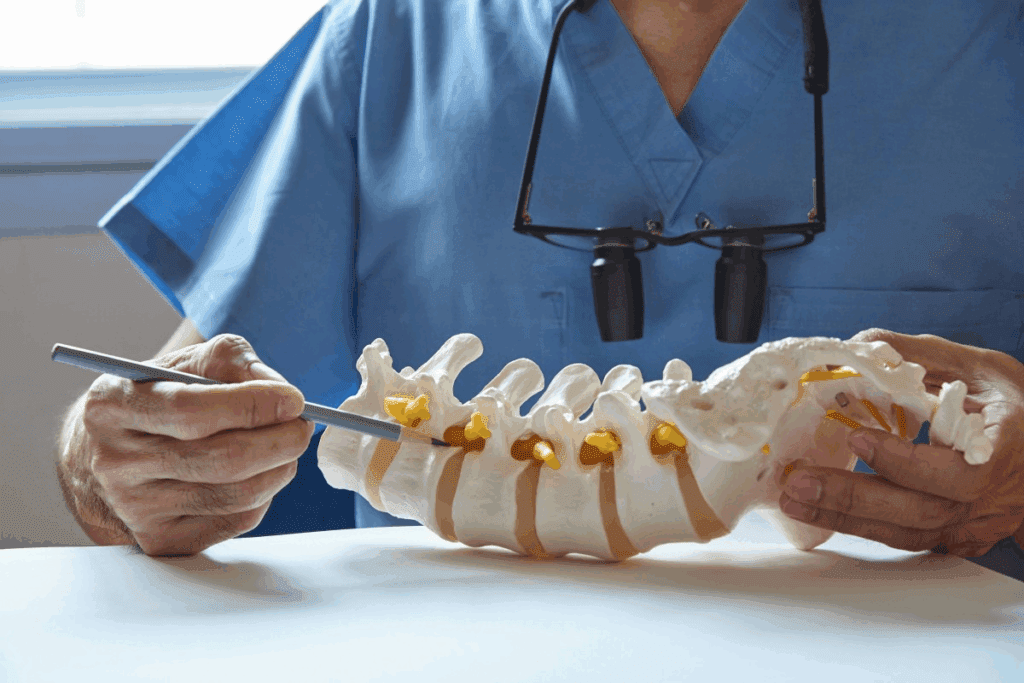
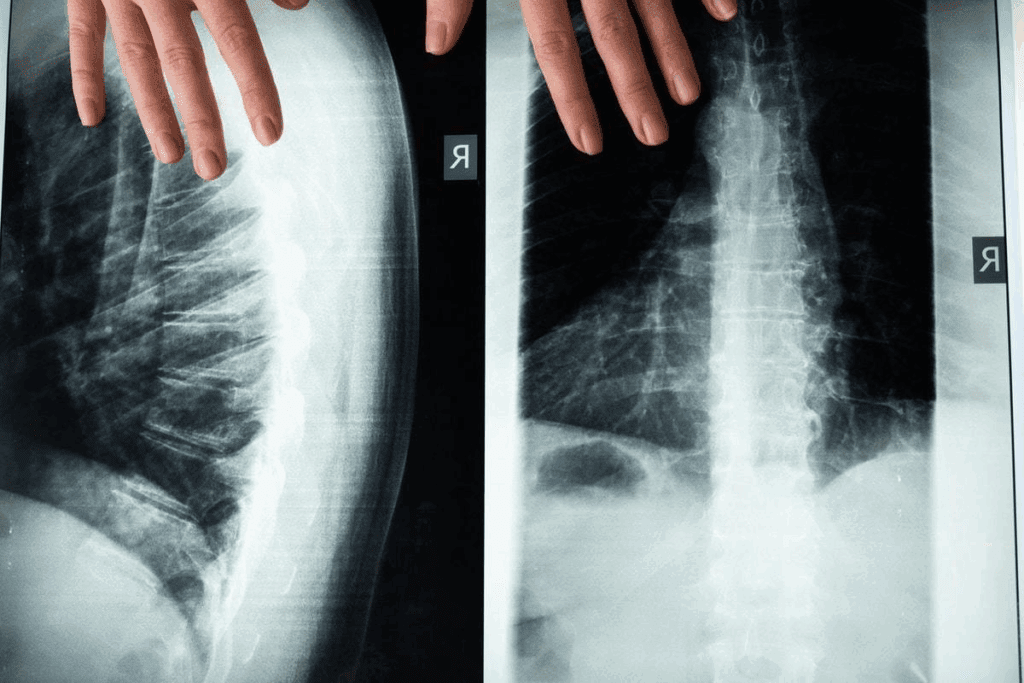
Diagnosing Compression Fractures
To diagnose vertebral compression fractures, we use a mix of clinical checks and advanced imaging. These steps help us spot the fracture and figure out how bad it is.
Imaging Tests and Procedures
Several imaging tests are key in spotting vertebral compression fractures. These include:
- X-rays: Give us the first look at the spine to find fractures.
- CT Scans: Show detailed images from different angles, helping us see how serious the fracture is.
- MRI: Helps us check for soft tissue damage and find other pain causes.
These tests are essential for figuring out how bad the fracture is and what treatment to use.
Differentiating Types of Vertebral Fractures
It’s important to know the different types of vertebral fractures to plan the right treatment. The main types are:
| Type of Fracture | Description | Common Causes |
| Osteoporotic Compression Fracture | Fracture caused by weak bones. | Osteoporosis, minor trauma |
| Traumatic Compression Fracture | Fracture from a big impact. | Accidents, falls, sports injuries |
| Pathological Compression Fracture | Fracture from bone disease or tumor. | Cancer, bone infections, metabolic bone diseases |
Knowing the exact type of fracture is key to picking the best treatment.
Initial Steps After Diagnosis
Getting diagnosed with a vertebral compression fracture means taking quick action. We’ll show you what to do right after you find out and when to rush to the hospital.
Immediate Actions to Take
Right after you’re told you have a fracture, there are steps to take. Rest and avoid hard activities that might make the fracture worse. Here’s what we suggest:
- Avoid heavy lifting
- Don’t bend or twist too much
- Use the right lifting methods if you must lift
Also, check your meds with your doctor. Make sure they won’t hurt your bones or slow down healing.
When to Seek Emergency Care
Knowing when to get help is key when you have a vertebral compression fracture. Severe pain that doesn’t get better, or new numbness or weakness in your arms or legs, means you need to go to the emergency room.
| Symptom | Action |
| Severe pain not relieved by rest or medication | Seek emergency care |
| New numbness or weakness in limbs | Seek emergency care |
| Increased difficulty walking or maintaining balance | Consult your healthcare provider |
Knowing these steps and when to get help can really help your recovery. We’re here to support you every step of the way with your vertebral compression fracture.
Conservative Vertebral Compression Fracture Treatment Options
When someone gets a vertebral compression fracture, the first step is usually to treat it without surgery. This helps ease the pain and lets the body heal. It’s important to start with these steps to help patients feel better and live better lives.
Rest and Activity Modification
One key part of treatment is to rest and change how you move. You should avoid lifting heavy things or bending a lot. This helps the spine heal without getting worse.
It’s not about staying in bed all day. It’s about making small changes to your daily life. Use the right lifting techniques and take breaks to rest. This helps your spine without putting too much strain on it.
Pain Management Techniques
Managing pain is a big part of treating vertebral compression fractures. We use different methods to help with pain, including:
- Medications: We might use over-the-counter or prescription drugs to help with pain.
- Heat or Cold Therapy: Applying heat or cold packs can help lessen pain and discomfort.
- Rest: Getting enough rest is key to letting the fracture heal.
We tailor pain management to each patient. We work closely with them to find the best way to manage their pain.
“Pain is a complex and multifaceted experience that requires a thorough treatment plan. By effectively managing pain, we can greatly improve a patient’s quality of life and help them heal.”
Physical Therapy Approaches
Physical therapy is also very important. It helps patients get stronger, more flexible, and improves their spinal health. A physical therapist can create a special exercise plan to:
- Strengthen the muscles around the spine
- Improve posture and lower the risk of more fractures
- Boost mobility and flexibility
Adding physical therapy to their treatment plan can lead to better results. It can also lower the chance of long-term problems.
| Treatment Approach | Benefits | Key Components |
| Rest and Activity Modification | Reduces stress on the spine, promotes healing | Avoiding heavy lifting, proper lifting techniques |
| Pain Management Techniques | Manages pain, improves quality of life | Medications, heat or cold therapy, rest |
| Physical Therapy Approaches | Regains strength, improves flexibility, enhances spinal health | Personalized exercise programs, strengthening muscles, improving posture |
Conservative treatments for vertebral compression fractures offer a complete way to handle the condition. They focus on easing symptoms and improving spinal health in the long run.
Medication Options for Pain Relief
Managing pain is key to improving life for those with vertebral compression fractures. It’s a big part of their care.
Over-the-Counter NSAIDs and Analgesics
OTC meds like NSAIDs (e.g., ibuprofen, naproxen) and analgesics (e.g., acetaminophen) are often first. They help cut down inflammation and ease pain.
- NSAIDs: Good for reducing inflammation and pain.
- Analgesics: Help with pain, with acetaminophen being a top pick.
Prescription Pain Medications
For really bad pain, prescription meds are needed. This includes stronger opioids or other non-opioid meds.
- Opioids: For severe pain, but used short-term due to side effects and dependency risk.
- Non-opioid prescription medications: May include muscle relaxants or certain antidepressants for pain.
Vertebral Compression Fracture Medication Considerations
Choosing pain relief meds involves many factors. These include the patient’s health history, drug interactions, and side effects risks.
- Medical history: Past health issues can guide medication choices.
- Drug interactions: Possible effects of mixing with other meds.
- Side effects: Knowing the possible downsides of the meds.
Finding the right pain relief is vital for vertebral compression fractures. Healthcare providers can tailor care by understanding these options and their considerations.
Bracing and External Support Methods
Bracing and external support are key in managing vertebral compression fractures. They help stabilize the spine and reduce pain. This approach is a conservative treatment that aids in the healing process.
Types of Braces for Vertebral Fractures
There are many braces for vertebral compression fractures, each with its own purpose. Here are a few common ones:
- Jewett brace: This hyperextension brace is great for fractures at the thoracolumbar junction.
- Thoracic lumbar sacral orthosis (TLSO) brace: It supports the thoracic, lumbar, and sacral spine, giving full stability.
- Cruciform anterior spinal hyperextension (CASH) brace: This hyperextension brace is easy to wear and offers good spine support.
Proper Bracing Techniques and Duration
Using braces correctly is vital for managing vertebral compression fractures. The brace must fit well to support the spine without discomfort. The time to wear a brace varies based on the fracture’s severity and the person’s health.
Bracing is usually recommended for 6 to 12 weeks. Regular check-ups with a healthcare provider are key to track healing and adjust the brace as needed.
Effectiveness in Acute Vertebral Compression Fracture
Bracing is very effective for acute vertebral compression fractures. It provides immediate stability, reducing pain and preventing further spine injury. Research shows bracing can greatly improve outcomes, helping patients get back to their normal activities sooner.
“Bracing is a simple yet effective method for managing vertebral compression fractures, improving patients’ quality of life.”
Talking to a healthcare professional about bracing’s benefits and limitations is important. They can help decide the best treatment plan for you.
Minimally Invasive Procedures
We use special procedures to fix broken vertebrae and ease pain in patients with vertebral compression fractures. These methods are key in treatment plans. They help those who don’t get better with just rest or have serious fractures.
Vertebroplasty: Process and Benefits
Vertebroplasty is a small procedure where bone cement is injected into a broken vertebra. The process involves using images to guide the cement’s placement. It brings quick pain relief and better movement for many.
Kyphoplasty: Technique and Outcomes
Kyphoplasty is another small technique. It uses a balloon to make space in the broken vertebra before adding cement. This technique can help regain some lost height and reduce kyphosis. It often leads to less pain and better spinal stability.
Vertebral Augmentation Advances
New advancements in vertebral augmentation focus on better cement materials and new techniques. These advances aim for longer-lasting pain relief and fewer complications.
By using these small procedures, we can help patients with vertebral compression fractures. It improves their life quality.
Treating Specific Types of Compression Fractures
Different types of compression fractures need different treatments. The location and details of the fracture play a big role in how it’s treated.
Lumbar Compression Fracture Treatment
Lumbar compression fractures happen in the lower back. They often need a mix of treatments. Pain management is key, using medicine and physical therapy to help move and strengthen the back.
Thoracic Compression Fracture Management
Thoracic compression fractures are in the mid-back. They’re tricky because of the spine’s shape there. Treatment might include bracing and pain relief. Sometimes, procedures like vertebroplasty or kyphoplasty are needed for severe cases.
Addressing Compression Fracture with Retropulsion
Fractures with retropulsion are serious because they can harm nerves. They need quick and strong treatment. This might mean surgery to take pressure off the spinal cord or nerves.
Knowing the exact type of fracture is key to a good treatment plan. Tailoring treatment to each fracture can greatly improve a patient’s life.
Managing Osteoporosis-Related Vertebral Fractures
Treating vertebral fractures linked to osteoporosis requires a mix of approaches. This includes using medications to strengthen bones and making lifestyle changes. Osteoporosis increases the risk of these fractures, so it’s key to stop bone loss.
Bone-Strengthening Medications
Medicines that make bones stronger are vital in treating these fractures. They help increase bone density, lowering the chance of more fractures. Common medicines include bisphosphonates, denosumab, and teriparatide.
Bisphosphonates, like alendronate and risedronate, are often the first choice. They slow down bone loss, making bones denser. Denosumab works by stopping bone breakdown through a different method.
Lifestyle Modifications for Bone Health
Changing your lifestyle is also key to keeping bones healthy and preventing more fractures. This includes eating right, exercising, and avoiding falls.
Eating foods high in calcium and vitamin D is important. Patients should eat more dairy, leafy greens, and fortified foods. Also, doing exercises that make bones stronger is helpful.
- Ensure adequate calcium and vitamin D intake
- Engage in regular weight-bearing exercise
- Implement fall prevention strategies at home
Specialized Approaches for Osteoporotic Fractures
Some patients might need special treatments for their fractures. These include vertebroplasty and kyphoplasty, which are less invasive. They help stabilize the vertebra and ease pain.
Vertebroplasty fills the fractured vertebra with bone cement. Kyphoplasty uses a balloon to make space before adding cement. Both can greatly reduce pain and improve movement.
By using medicines, making lifestyle changes, and sometimes special treatments, doctors can manage these fractures well. This helps patients live better lives.
Recovery and Rehabilitation Process
The journey to recover from vertebral compression fractures is detailed. It includes healing, rehabilitation, and watching for complications. We’ll walk you through each step to help you understand the process.
Timeline for Healing
The healing time for vertebral compression fractures varies. It usually starts with managing pain and stabilizing the fracture, which can take weeks. Pain relief medications and rest are key during this time.
As the fracture heals, usually in 6-12 weeks, you can start moving more. But always do so with your healthcare team’s advice.
Rehabilitation Exercises and Therapy
Rehabilitation is vital to regain strength and function. Physical therapy starts when the pain lessens and the fracture stabilizes. Exercises include stretching, strengthening the back and core, and improving posture.
- Stretching exercises to improve flexibility
- Strengthening exercises for back and core muscles
- Postural training for better spinal alignment
Monitoring Progress and Addressing Complications
Regular check-ups with healthcare providers are key. They help track healing and catch any issues early. This might include imaging tests to see how the fracture is healing.
By watching closely, we can quickly handle any problems. This ensures the best recovery outcome.
Throughout recovery, patient education and following the treatment plan are critical. Understanding the importance of medication, physical therapy, and lifestyle changes is essential for a successful recovery.
Quality of Life Improvements After Treatment
Vertebral compression fracture treatment does more than just ease pain. It changes a patient’s life in many ways. It helps them feel better, be more independent, and do things they love again.
Pain Relief Outcomes
One main goal of treating vertebral compression fractures is to reduce pain. When treatment works well, it can make a big difference. Patients often say they feel much less pain and can do things they couldn’t before.
Mobility and Function Restoration
Another key part of treatment is getting patients to move better. It helps them get stronger and more flexible. This way, they can do everyday tasks easily and avoid more problems from being stuck in one place for too long.
Psychological Well-being
Vertebral compression fractures can also affect a person’s mind. Long-term pain and not being able to move can make someone feel lonely and sad. Good treatment not only fixes the physical issues but also helps the mind. It makes patients feel better about themselves and helps them connect with others again.
We know that everyone’s experience is different. But with the right treatment and support, many people see big improvements in their lives.
Conclusion
Managing vertebral compression fractures needs a full plan. We’ve looked at many ways to treat them, from simple steps to more complex methods. Each method is chosen based on the patient’s needs for the best results.
Dealing with these fractures means more than just fixing the immediate problem. We also look at what caused it and how it might affect the future. Care includes managing pain, physical therapy, and sometimes surgery like vertebroplasty or kyphoplasty.
By taking a complete care approach, we can make a big difference. This way, patients can live better lives and avoid more fractures. Our talk shows how working together is key to the best care for these fractures.
The main aim is to help patients function better, feel less pain, and be healthier overall. With a detailed care plan and focusing on the patient, we can help them get back to their normal life.
FAQ
What are the common treatment options for managing vertebral compression fractures?
We offer several treatments. These include rest, pain management, and physical therapy. We also do vertebroplasty and kyphoplasty, which are minimally invasive.
How are vertebral compression fractures diagnosed?
Diagnosing these fractures involves imaging tests. We use X-rays, CT scans, and MRI to see the extent of the fracture. This helps us decide the best treatment.
What are the signs and symptoms of a vertebral compression fracture?
Signs include back pain and limited mobility. You might also notice a change in posture or height. If you have severe or ongoing back pain, see a doctor.
How can osteoporosis-related vertebral fractures be managed?
Managing these fractures involves several steps. We use medications to strengthen bones and make lifestyle changes. We also tailor treatments to each patient’s needs.
What is the recovery process like after a vertebral compression fracture?
Recovery starts with rest. Then, we do rehabilitation exercises to improve mobility and strength. We also watch for any complications.
Can bracing help in the treatment of vertebral compression fractures?
Yes, bracing can help. It stabilizes the spine and aids in healing. We choose the right brace based on the fracture’s severity and location.
What are the benefits of minimally invasive procedures like vertebroplasty and kyphoplasty?
These procedures offer pain relief and stabilize the vertebra. They improve quality of life. We discuss the benefits and risks to see if they’re right for you.
How can I manage pain associated with a vertebral compression fracture?
We offer several pain management options. These include NSAIDs, analgesics, and prescription medications. The choice depends on your pain level and health.
What lifestyle changes can help improve bone health and reduce the risk of future fractures?
We suggest a balanced diet, regular exercise, and avoiding smoking and alcohol. These help improve bone health.
How long does it take to heal from a vertebral compression fracture?
Healing time varies. It depends on the fracture’s severity, treatment effectiveness, and individual factors. We provide a personalized timeline.
What are the possible complications of vertebral compression fractures?
Complications include chronic pain and limited mobility. In severe cases, there might be spinal deformity or neurological issues. We closely monitor patients to address any complications.
Can vertebral compression fractures be prevented?
While some risks can’t be avoided, we recommend preventive measures. These include maintaining strong bones through diet and exercise, and managing osteoporosis. This reduces the risk of fractures.
Reference
- Cauley, J. A. (2015). Osteoporosis: diagnosis and management. Journal of Clinical Endocrinology & Metabolism, 100(11), 3964-3972.
https://doi.org/10.1210/jc.2015-2516