Considering vertebroplasty surgery? Learn 7 key facts about this cement injection procedure for fractured vertebrae in our simple guide.
At Liv Hospital, we know how tough fractured vertebrae can be. Vertebroplasty is a minimally invasive procedure. It injects medical cement into the fractured vertebrae. This helps stabilize the spine and eases pain.
The Medical organization says this treatment injects cement into a cracked or broken spinal bone. It helps relieve pain. This way, we can quickly give relief and stability to those with vertebral fractures.
Key Takeaways
- Vertebroplasty is a minimally invasive procedure for treating fractured vertebrae.
- Medical cement is injected into the fractured vertebrae to stabilize the spine.
- The primary goal is to alleviate pain and provide stability.
- Liv Hospital offers internationally recognized expertise in vertebroplasty.
- Advanced cement injection techniques are used for effective treatment.
What Is Vertebroplasty Surgery? A Modern Approach to Spinal Fractures
Vertebroplasty surgery is a new way to treat spinal fractures. It helps ease pain and makes the spine stable. Doctors find it very effective for vertebral compression fractures.
The Definition of Vertebroplasty and Basic Principles
Vertebroplasty is a surgery where bone cement is put into broken vertebrae. It makes the spine stable and relieves pain. The goal is to fix the spine’s structure and stop the pain.
The surgery uses Polymethylmethacrylate (PMMA), a special bone cement. It’s injected into the vertebra under X-ray, making sure it’s placed right. This reduces the chance of problems.
The Evolution of Cement Injection Procedures for the Spine
The idea of using cement in the spine started in the 1980s for hemangiomas. Over time, the method has improved a lot. Now, vertebroplasty is a safe and effective way to treat spinal fractures.
Improvements in cement and how it’s injected have made vertebroplasty popular. It gives quick pain relief and helps patients move better.
Who Needs Cement Injection in Spine Procedures?

Cement injection in spine procedures is a key treatment for many spinal issues. We decide if someone needs it based on the type and how bad the spinal fracture is.
Osteoporotic Vertebral Compression Fractures
Osteoporotic vertebral compression fractures are common in older adults, often those with osteoporosis. These happen when vertebrae collapse because the bones are weak. Cement injection through vertebroplasty can make the vertebrae stable and reduce pain.
Johns Hopkins Medicine data shows vertebroplasty is often used for these fractures. It can greatly improve life quality for those with these fractures.
Traumatic Injuries and Pathological Fractures
Traumatic injuries, like those from car accidents or falls, can lead to spinal fractures needing cement injection. Also, fractures caused by cancer or bone tumors can benefit from this procedure.
We use cement injection to keep the spine stable and prevent more damage. It’s very helpful for patients at risk of more problems because of their condition.
Understanding when cement injection in spine procedures is needed helps us see its value. It’s vital for treating osteoporotic fractures, traumatic injuries, and pathological fractures. Cement injection helps restore spinal stability and eases pain.
The Vertebroplasty Surgery Procedure Explained
Patients going through vertebroplasty surgery first get a detailed check-up. This check is key to see if the surgery is right for them. It also helps plan the best treatment.
Pre-Surgical Assessment and Patient Preparation
Before the surgery, patients get a full review. This includes looking at their medical history, a physical check, and imaging like X-rays or MRI. It helps spot any risks and gets the patient ready for surgery.
Patients are told to stop taking certain medicines that might affect the surgery or healing. They also need to not eat or drink for a while before the surgery. Our team gives clear instructions to make sure patients are ready.
How Cement Is Injected Into Spine During the Procedure
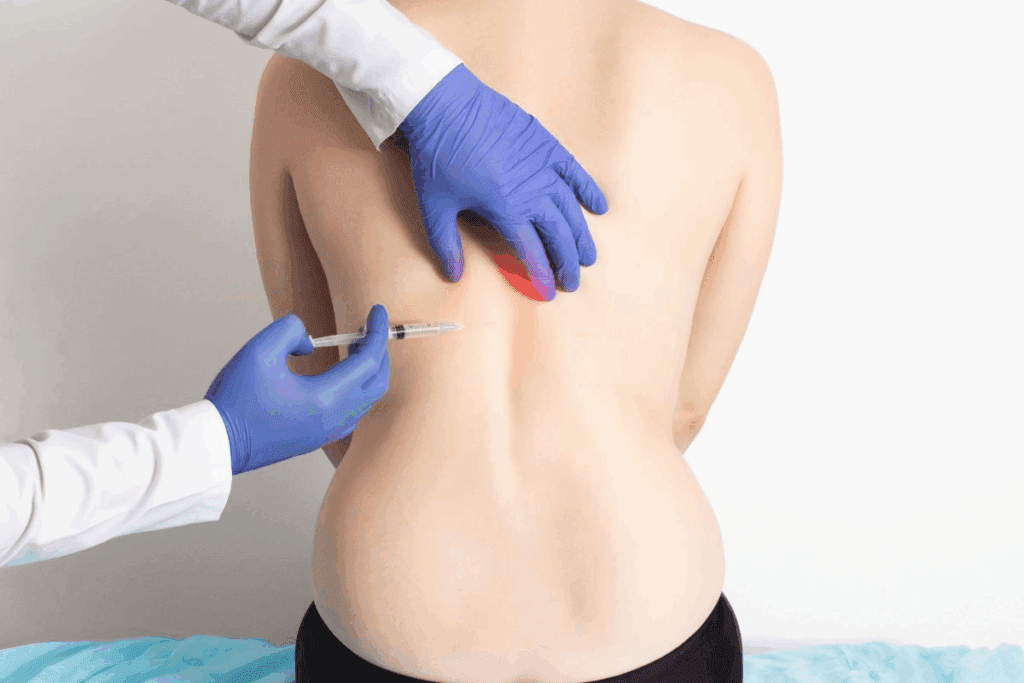
The patient lies on their stomach on an X-ray table during the procedure. They are given local anesthesia and sedation to make the process comfortable. A small cut is made in the back, and a needle is carefully placed in the vertebra under X-ray.
Then, bone cement is slowly put into the vertebra. This cement fills the bone spaces, making it stable and easing pain. The surgery is done one vertebra at a time, but can be done on more if needed.
Types of Medical Cement Used in Back Surgery
The main cement used is polymethylmethacrylate (PMMA). It’s a trusted material used in orthopedic surgery for years. PMMA is mixed to the right consistency and hardens fast after being injected.
Other cements, like calcium phosphate, are being looked at for vertebroplasty. They might have special properties, like being broken down by the body over time.
Our team picks the best cement for each patient based on their needs and condition.
The Science of Cement in Back Procedures
Cement in back procedures has changed how we treat spinal fractures. It offers a less invasive way to help patients with vertebral compression fractures. We’ll look into the science behind this, focusing on the material used and its effects on the spine.
Polymethylmethacrylate (PMMA): The Standard for Cement Back Surgery
Polymethylmethacrylate (PMMA) is the top choice for vertebroplasty procedures. Johns Hopkins Medicine says PMMA is great because it makes fractured vertebrae stable right away. PMMA is also safe for the body and hardens fast, making it perfect for this job. PMMA has:
- High biomechanical strength
- Rapid hardening
- Compatibility with human tissue
These traits help PMMA make fractured vertebrae stable. This reduces pain and helps patients move better.
Biomechanical Effects of Cement on Fractured Vertebrae
PMMA cement injected into fractured vertebrae has big effects. It fills in the gaps in the vertebra, making the spine strong again. Studies show this can:
- Lessen pain by stabilizing the fracture
- Improve spinal alignment
- Make patients more mobile
The effects of PMMA cement are key in treating vertebral compression fractures. They greatly affect how well patients recover and live their lives.
Benefits and Success Rates of Cement Injection in Spine
Cement injection in spine procedures has changed how we treat vertebral fractures. It offers many benefits to patients. Studies show it’s effective in giving quick pain relief and improving how well patients can move.
Rapid Pain Relief: 90% Patient Recovery Statistics
Cement injection in spine procedures quickly relieves pain. About 90% of patients see a big drop in pain after vertebroplasty. This is a big plus because it lets patients get back to their daily lives faster.
Research backs up these benefits. A study in the Journal of Vascular and Interventional Radiology found 87% of patients felt better after vertebroplasty. Another study in the Spine Journal showed a 92% success rate in pain relief. These numbers show how reliable cement injection in spine procedures is.
Key statistics on pain relief:
- 90% of patients experience significant pain reduction
- 87% of patients report improved pain scores
- 92% success rate in pain relief reported in some studies
Improved Mobility and Return to Daily Activities
Cement injection in spine procedures does more than just relieve pain. It also makes it easier for patients to move around. This is because it stabilizes the fractured vertebra, allowing patients to do daily activities without pain. This is key for a full recovery and a better quality of life.
Patients who get vertebroplasty can usually get back to their normal activities in just a few weeks. This is a big plus compared to more invasive surgeries, which take longer to recover from.
Cost-Effectiveness Compared to Traditional Broken Vertebrae Surgery
Cement injection in spine procedures is also cheaper than traditional surgery for broken vertebrae. It’s a less invasive procedure that needs less hospital time and resources than open surgery.
A study comparing costs found vertebroplasty is much cheaper. It needs less hospital time, has simpler post-operative care, and patients can get back to work faster. All these factors add up to big cost savings.
Benefits of cost-effectiveness:
- Reduced hospital stay
- Less complex post-operative care
- Quicker return to work
Potential Risks and Complications of Cement in Back Surgery
Vertebroplasty is usually safe, but there are risks. These can be lessened with the right patient care and technique. It’s key to know these risks to avoid problems.
Common Side Effects After Cement Procedure in Back
After vertebroplasty, some people might feel pain at the injection site, mild fever, or be tired. These symptoms usually go away in a few days. Some might also feel more pain relief as the cement helps the vertebra.
Following post-procedure instructions is very important. Avoid heavy lifting, bending, or hard work for a while.
Serious Complications: Cement Leakage and Pulmonary Embolism
Cement leakage is a big risk with vertebroplasty. It happens when cement gets out of the vertebra. This can sometimes press on other parts or, worse, cause cement to go to the lungs.
Cement pulmonary embolism is rare but very dangerous. Look out for sudden breath trouble, chest pain, or coughing. Get medical help right away if you have these symptoms.
Contraindications for Vertebroplasty
Not everyone can have vertebroplasty. You can’t have it if you have an active infection, are allergic to the cement, or have certain fractures. Also, if your vertebra is severely damaged or has a big hole, it’s not a good choice.
We check each patient carefully to see if vertebroplasty is right for them. We look at the fracture type, how severe it is, and your overall health.
Knowing about these risks helps patients make better choices. It’s a team effort between doctors and patients to get the best results.
Recovery Timeline After Cement Spine Surgery
Knowing what to expect after cement spine surgery is key. It helps patients manage their recovery smoothly. We’ll cover what happens right after, the long-term recovery, and the role of follow-up care.
Immediate Post-Procedure Expectations
Vertebroplasty often brings quick pain relief, with some feeling better the next day. Johns Hopkins Medicine says recovery takes weeks. Right after, patients might feel:
- Soreness at the injection site: This side effect usually goes away in a few days.
- Relief from fracture pain: Many see a big drop in pain soon after.
- Fatigue: The procedure can be exhausting, so rest is important.
It’s vital to follow your doctor’s post-procedure instructions. This helps avoid complications and ensures a smooth recovery.
Long-term Recovery and Activity Guidelines
In the long-term recovery, patients should:
- Gradually increase activity levels: Start with light movements and slowly add more intensity and time.
- Avoid heavy lifting and bending: These can stress the spine and should be avoided for weeks.
- Follow a rehabilitation program: Physical therapy can boost mobility and strength.
Most can get back to normal in a few weeks. But, always follow your doctor’s specific advice.
Follow-up Care and Monitoring Vertebral Stability
Regular follow-ups are key to check on the vertebrae’s stability and catch any issues early. We suggest:
- Regular check-ups: Keep appointments with your healthcare provider to track your progress.
- Imaging tests: X-rays or other tests might be needed to check the vertebrae’s stability.
- Reporting any new symptoms: Tell your healthcare provider right away if you notice any new or worsening symptoms.
By following these guidelines and staying in touch with your healthcare team, you can have a successful recovery after cement spine surgery.
The Growing Market for Vertebroplasty: Statistics and Trends
As the world’s population ages, more people need vertebroplasty. This is making the market grow fast. We’re seeing a big change in healthcare, with more need for treatments for broken vertebrae.
Annual Procedure Rates: Over 100,000 in the US Alone
In the United States, over 100,000 vertebroplasty procedures happen every year. This number is likely to go up as more people get older and more fractures happen.
Key Statistics:
| Region | Annual Procedures | Growth Rate |
| United States | 100,000+ | 5% |
| Europe | 80,000+ | 4% |
| Asia-Pacific | 50,000+ | 6% |
Global Market Projections: Reaching $1.6 Billion by 2035
Experts predict the global vertebroplasty market will hit $1.6 billion by 2035. This growth comes from more procedures, better technology, and more people knowing about vertebroplasty’s benefits.
New cement types and delivery systems are key to this growth.
Innovations Improving Safety and Efficacy of Cement Procedures
New tech in vertebroplasty is making procedures safer and more effective. These include:
- New cement materials with better properties
- Improved systems for injecting cement
- Advanced imaging for clearer views during procedures
With tech getting better and more procedures happening, the market is set to grow a lot. We’re here to keep you updated on this fast-changing field.
Conclusion: Making Informed Decisions About Vertebroplasty
Vertebroplasty is a key treatment for spinal fractures. It brings quick pain relief and better mobility to many. When done by skilled doctors, it’s safe and works well, as the Medical organization says.
To choose vertebroplasty wisely, patients need to know its good points and possible downsides. This knowledge helps them pick the best treatment for their health and goals.
Deciding on vertebroplasty should be a team effort with a healthcare expert. They consider your unique situation and the latest research. This way, you make the best choice for your care.
FAQ
What is vertebroplasty surgery?
Vertebroplasty surgery is a minimally invasive procedure. It involves injecting medical cement into fractured vertebrae. This helps stabilize the spine and relieve pain.
What conditions require cement injection in spine procedures?
Cement injection is needed for osteoporotic vertebral compression fractures. It’s also used for traumatic injuries and pathological fractures. These conditions cause vertebral instability and pain.
How is cement injected into the spine during vertebroplasty?
Cement is injected through a needle during vertebroplasty. The needle is guided into the fractured vertebra using imaging technology. This includes fluoroscopy or CT scans.
What type of medical cement is used in vertebroplasty?
Polymethylmethacrylate (PMMA) is the most common medical cement used. It’s biocompatible and provides stability and support to the fractured vertebrae.
What are the benefits of vertebroplasty?
Vertebroplasty offers rapid pain relief and improved mobility. It allows for a quick return to daily activities. Success rates are reported in up to 90% of patients.
What are the possible risks and complications of vertebroplasty?
Risks include cement leakage, pulmonary embolism, infection, and nerve damage. These complications are rare when experienced practitioners perform the procedure.
How long does it take to recover from vertebroplasty?
Recovery is typically quick. Most patients experience significant pain relief within a few days. They can return to normal activities within a few weeks.
What is the growing market trend for vertebroplasty?
The global market for vertebroplasty is rapidly growing. It’s driven by an aging population, increasing osteoporosis, and advancements in technology. Projections reach $1.6 billion by 2035.
Is vertebroplasty a cost-effective treatment option?
Yes, vertebroplasty is cost-effective compared to traditional surgical methods. It reduces hospital stay, recovery time, and healthcare costs.
What are the contraindications for vertebroplasty?
Contraindications include active infection, bleeding disorders, and severe vertebral destruction or collapse. Patients should be carefully evaluated before undergoing the procedure.
References
Peng, J., et al. (2024). Systematic review and meta-analysis of current evidence in uterine artery embolization compared to myomectomy on symptomatic uterine fibroids. Scientific Reports, 14, Article 12345. https://www.nature.com/articles/s41598-024-69754-0























