Nearly 40% of adults in the United States are vitamin D deficient. This shows how vital it is to understand vitamin D activation in liver and kidneys and how these organs turn this key nutrient into its active form.
Understanding Vitamin D activation in liver and kidneys is crucial for health, as these organs play a vital role in the conversion process.
This Vitamin D activation in liver and kidneys ensures the nutrient is bioavailable for its various bodily functions.
Vitamin D activation begins in the skin with sunlight exposure, then continues in the liver and kidneys, where it is converted into its active form.
The vitamin D pathway is key for keeping our bones healthy and controlling our body’s functions. Two organs are essential in this process.
Vitamin D is key to our health and fighting diseases. It’s a fat-soluble vitamin that helps keep our bones strong and our overall health good.
Vitamin D activation in liver and kidneys is integral to hormone regulation and immune function.
Vitamin D is a group of fat-soluble secosteroids. It helps keep calcium and phosphate levels right in our bodies. This is vital for our bones. The term “vitamin D” includes several types, but D2 and D3 are the most important.
Vitamin D activation in liver and kidneys influences many aspects of health, warranting close attention.
Vitamin D activation in liver and kidneys is foundational for understanding its broader health implications.
Vitamin D activation in liver and kidneys is essential for maintaining optimal calcium levels in the body.
The process of Vitamin D activation in liver and kidneys involves multiple enzymes and metabolic pathways.
By understanding the Vitamin D activation in liver and kidneys, individuals can better manage their overall health.
Vitamin D comes in two main types: D2 and D3. Vitamin D2 comes from fungi and is in some foods and supplements. Vitamin D3 is made in our skin when we’re in the sun. It’s also in some animal foods and supplements.
Vitamin D3 is more important for humans. It’s the form our skin makes and is better at raising vitamin D levels in our blood.
Knowing about the different forms of vitamin D helps us understand how it works in our bodies. It’s important for keeping vitamin D levels just right.
Vitamin D activation in liver and kidneys is significant for enhancing bone density and overall skeletal health.
Understanding the Vitamin D activation in liver and kidneys can help in addressing deficiencies and related health issues.
The body gets vitamin D from several sources. Knowing these sources is key to keeping vitamin D levels right. This is vital for our health.
Sunlight is a main way to get vitamin D. UVB rays from the sun make vitamin D3 in our skin. This is important for our vitamin D levels.
But, things like skin color, age, and where you live can change how much vitamin D you make.
Vitamin D activation in liver and kidneys plays a significant role in insulin sensitivity and metabolic health.
Foods are another way to get vitamin D. Foods like salmon, mackerel, and some cereals are good sources. They have vitamin D2 and D3.
Even though foods are helpful, they don’t give as much vitamin D as sunlight does.
Supplements are for those who can’t get enough vitamin D from sun and food. They come in D2 and D3 forms. D3 works better at raising vitamin D levels.
Supplements are good for people at risk of not having enough vitamin D. This includes those who don’t get much sun or have certain health issues.
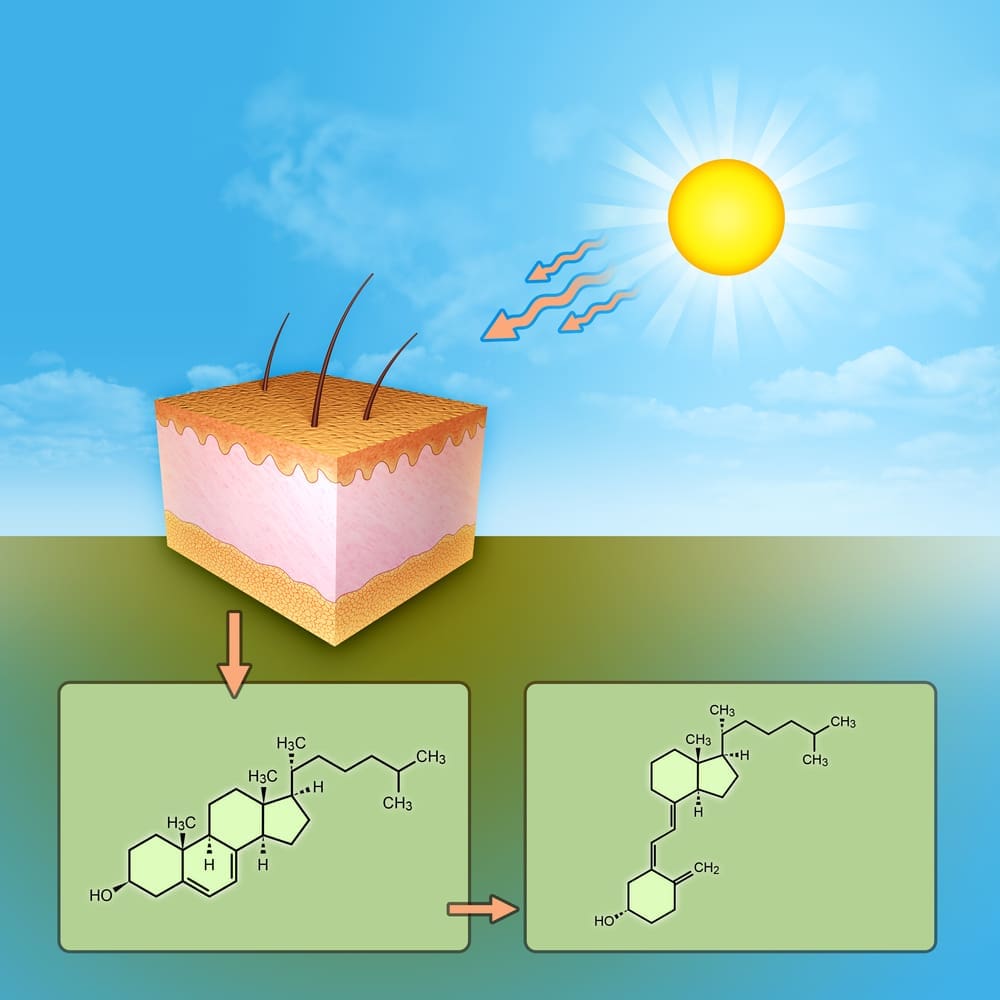
UVB radiation hitting the skin starts a chain of reactions that leads to vitamin D production. This process is key for keeping vitamin D levels in the body right.
The skin is where vitamin D is mainly made. This happens when UVB radiation gets through the skin layers. UVB radiation is vital because it gives the energy needed to change 7-dehydrocholesterol into previtamin D3.
UVB radiation is very important for making vitamin D. It’s the UV part that starts the chemical reaction to make previtamin D3. How much UVB radiation the skin gets depends on things like the time of day, season, and where you are.
When sunlight hits the skin, UVB rays turn 7-dehydrocholesterol into previtamin D3. This change happens because of UVB’s energy.
The change of 7-dehydrocholesterol to previtamin D3 is a big step in making vitamin D. This happens in the skin, thanks to UVB radiation’s energy. Previtamin D3 then turns into vitamin D3 through a heat change.
The new vitamin D3 goes into the blood. It then moves to the liver for more processing. This first step shows how important it is for the skin to get UVB radiation to keep vitamin D levels up.
The liver is key in vitamin D activation. It’s the first organ in this complex process. Vitamin D comes from sunlight, diet, or supplements. The liver changes it a lot.
The liver starts vitamin D’s transformation. It turns it into 25-hydroxyvitamin D, or calcidiol. This is important because calcidiol shows how much vitamin D we have.
Hydroxylation Process: The liver uses an enzyme called cytochrome P450 to change vitamin D. This step is essential for vitamin D to work right.
Turning vitamin D into calcidiol is a big deal. Calcidiol lasts longer in our bodies. It’s a good way to check if we have enough vitamin D.
| Metabolic Step | Location | Resulting Compound |
| Initial Hydroxylation | Liver | 25-hydroxyvitamin D (Calcidiol) |
Cytochrome P450 enzymes are important in vitamin D’s metabolism. The enzyme CYP2R1 helps turn vitamin D into 25-hydroxyvitamin D.
The liver’s role in vitamin D shows how organs and nutrients work together. Knowing this helps us understand vitamin D’s role in health.
The kidneys are key in the vitamin D activation process. They turn 25-hydroxyvitamin D into calcitriol, the active form of vitamin D. This step is vital for keeping calcium levels right and supporting bone health.
The kidneys are essential in vitamin D metabolism. They convert 25-hydroxyvitamin D into 1,25-dihydroxyvitamin D. This happens in the renal proximal convoluted tubules.
The renal cells have the enzymes needed for this conversion. They take in 25-hydroxyvitamin D, bound to vitamin D-binding protein, to start the process.
The conversion of 25-hydroxyvitamin D to 1,25-dihydroxyvitamin D is carefully controlled. This step is key because 1,25-dihydroxyvitamin D is the active form of vitamin D. It binds to vitamin D receptors in different tissues.
1,25-dihydroxyvitamin D (calcitriol) is vital for keeping calcium and phosphate levels balanced. It works in the intestines, bones, and kidneys to manage calcium levels.
The 1α-hydroxylase enzyme is responsible for changing 25-hydroxyvitamin D into 1,25-dihydroxyvitamin D. This enzyme is a cytochrome P450 enzyme found in the mitochondria of renal proximal tubular cells.
The activity of 1α-hydroxylase is controlled by several factors. Parathyroid hormone (PTH), calcium, and phosphate levels all play a role. PTH boosts the production of 1,25-dihydroxyvitamin D by increasing 1α-hydroxylase expression.
Vitamin D’s activation is a complex process. It involves the liver, kidneys, and specific enzymes. This pathway is key for bone health, immune function, and overall well-being.
The metabolism of vitamin D starts in the skin. UVB radiation triggers the synthesis of previtamin D3. This then transforms into vitamin D3.
Vitamin D activation in liver and kidneys is vital for metabolic pathways related to energy balance.
This vitamin D3 is carried to the liver by vitamin D-binding protein (DBP).
In the liver, vitamin D3 is changed by cytochrome P450 enzymes. It becomes 25-hydroxyvitamin D [25(OH)D], or calcidiol. This step is important because 25(OH)D is the main form of vitamin D in the blood.
The 25(OH)D then goes to the kidneys. There, it is changed again by 1α-hydroxylase. This creates 1,25-dihydroxyvitamin D [1,25(OH)2D], or calcitriol, the active form of vitamin D.
Vitamin D activation in liver and kidneys supports various physiological processes essential for life.
Two main enzymes are involved in vitamin D activation. CYP2R1 (and other cytochrome P450 enzymes) in the liver hydroxylates vitamin D to 25(OH)D. 1α-hydroxylase (CYP27B1) in the kidneys changes 25(OH)D to 1,25(OH)2D.
| Enzyme | Location | Function |
| CYP2R1 | Liver | Hydroxylates vitamin D to 25(OH)D |
| 1α-hydroxylase (CYP27B1) | Kidneys | Converts 25(OH)D to 1,25(OH)2D |
Awareness of the role of Vitamin D activation in liver and kidneys can guide effective healthcare practices.
Vitamin D-binding protein (DBP) is key in transporting vitamin D and its metabolites. It binds to vitamin D, 25(OH)D, and 1,25(OH)2D. This helps them move in the bloodstream and reach their target tissues.
The vitamin D activation process shows how vital the liver and kidneys are. Understanding this pathway helps us grasp vitamin D deficiency and its health effects.
Understanding how vitamin D is activated is key to knowing its role in our bodies. This process involves many biochemical steps.
Long-term health benefits are associated with adequate Vitamin D activation in liver and kidneys.
The interconnectedness of Vitamin D activation in liver and kidneys with other systems highlights its importance.
Vitamin D’s activation brings about big changes in its structure. It starts in the skin or comes from food. Then, it goes through hydroxylation in the liver to become 25-hydroxyvitamin D.
This form then moves to the kidneys for another hydroxylation. This makes it into the active form, 1,25-dihydroxyvitamin D.
The change from vitamin D to its active form needs enzymatic reactions. The liver’s first step is helped by cytochrome P450 enzymes. The kidneys’ second step is done by 1α-hydroxylase.
Vitamin D activation in liver and kidneys is a focus of current research in nutritional science.
Vitamin D works through different cellular pathways. It binds to its receptor, which changes how genes are expressed. This affects how cells behave.
The vitamin D receptor (VDR) is key in vitamin D’s effects. VDR is a nuclear receptor that controls genes related to calcium, immune response, and cell growth.
The bond between vitamin D and its receptor is vital. When 1,25-dihydroxyvitamin D binds to VDR, it changes shape. This lets it bind to DNA, controlling gene expression.
| Component | Function | Location |
| Cytochrome P450 enzymes | Mediate hydroxylation of vitamin D | Liver |
| 1α-Hydroxylase | Catalyzes conversion to active vitamin D | Kidneys |
| Vitamin D Receptor (VDR) | Regulates gene expression in response to vitamin D | Nucleus of cells |
Vitamin D has a big impact on stem cells. It affects how they grow and work. This is important for fixing damaged tissues.
Stem cells have special receptors for vitamin D. This means vitamin D can directly affect them. Studies show that vitamin D changes how stem cells grow and become different types of cells.
The way vitamin D and its receptors work together is complex. It involves many signals that change how genes work. This is key to understanding vitamin D’s role in stem cell growth.
Vitamin D affects how stem cells multiply and become different cells. This can change the number and types of cells made from stem cells. Research shows vitamin D helps stem cells turn into more mature cells. This is important for fixing tissues and growing new ones.
“Vitamin D is a key regulator of stem cell biology, influencing their proliferation and differentiation, with significant implications for regenerative medicine.”
Monitoring the Vitamin D activation in liver and kidneys may provide insights into various health conditions.
The connection between Vitamin D activation in liver and kidneys and chronic diseases continues to be explored.
Vitamin D activation in liver and kidneys should be a priority in health assessments and treatments.
Vitamin D activation in liver and kidneys contributes to overall cellular health and function.
The relationship between Vitamin D activation in liver and kidneys and metabolic disorders is an emerging area of research.
The effects of vitamin D on stem cells are very important for fixing damaged tissues. Knowing how vitamin D works with stem cells can help create new treatments. Using vitamin D could make stem cell therapies work better.
We need more research to fully understand vitamin D’s role in fixing damaged tissues. But, what we know so far is promising. Vitamin D might be a big help in making stem cell treatments more effective.
Vitamin D needs several important helpers to work right. Magnesium and zinc are key players. They help vitamin D get used by the body.
Vitamin D activation in liver and kidneys is a key factor in maintaining metabolic homeostasis.
Magnesium is vital for vitamin D to work well. It helps enzymes turn vitamin D into its active form. Without enough magnesium, vitamin D activation can fail.
Magnesium’s Role in Vitamin D Metabolism:
Vitamin D activation in liver and kidneys is paramount for achieving optimal health outcomes.
Zinc and vitamin K also play big roles with vitamin D. Zinc helps with vitamin D’s metabolism. Vitamin K is key for calcium in bones.
| Cofactor | Role in Vitamin D Metabolism |
| Magnesium | Enzyme cofactor for vitamin D conversion |
| Zinc | Cofactor for enzymes and proteins in vitamin D metabolism |
| Vitamin K | Regulates calcium deposition in bones |
Other nutrients like vitamin C and omega-3 fatty acids also help. Eating a balanced diet with these nutrients is key for vitamin D to work best.
Getting enough of these nutrients through food or supplements boosts vitamin D’s effect. This is good for your health.
There is a growing body of evidence supporting the need for Vitamin D activation in liver and kidneys for optimal health.
Vitamin D is not just made in the kidneys. It’s also activated in other tissues, like immune cells. This local activation is key to its function.
Immune cells, like macrophages and T lymphocytes, have an enzyme called 1α-hydroxylase. This enzyme turns 25-hydroxyvitamin D into 1,25-dihydroxyvitamin D. This process is vital for the immune system’s function.
Key aspects of local activation in immune cells include:
Other tissues, like the skin, prostate, and colon, also activate vitamin D. This extra-renal activation is important for many bodily functions. It may also help prevent or treat diseases.
Research is ongoing to understand the clinical importance of extra-renal vitamin D activation. It may play a role in preventing and treating diseases. This includes autoimmune diseases, cancers, and cardiovascular diseases.
| Disease/Condition | Role of Extra-Renal Vitamin D Activation |
| Autoimmune Diseases | Modulation of immune response, potentially reducing disease severity |
| Cancer | Influence on cell proliferation and differentiation, potentially inhibiting tumor growth |
| Cardiovascular Diseases | Potential role in vascular health and blood pressure regulation |
In conclusion, extra-renal vitamin D activation is complex and vital for health. More research is needed to fully grasp its mechanisms and benefits.
Vitamin D activation in liver and kidneys can be enhanced through specific dietary choices and supplements.
Vitamin D is key for bone health, immune function, and overall health. Its activation and metabolism depend on the function of certain organs. This shows a complex relationship between vitamin D and organ function.
Liver disease can harm vitamin D activation. The liver starts vitamin D’s metabolic process by converting it to 25-hydroxyvitamin D. Liver dysfunction can lower this metabolite, affecting vitamin D levels.
Understanding Vitamin D activation in liver and kidneys can help guide nutritional recommendations for better health.
The liver uses an enzyme called cytochrome P450 for this conversion. Liver diseases like cirrhosis or hepatitis can damage this process. This leads to a vitamin D deficiency.
Awareness of Vitamin D activation in liver and kidneys is essential for optimizing health interventions.
Kidney disease also plays a big role in vitamin D deficiency. The kidneys convert 25-hydroxyvitamin D to its active form, 1,25-dihydroxyvitamin D. Kidney dysfunction can stop this conversion, leading to low active vitamin D levels.
People with chronic kidney disease often have low vitamin D. This can cause bone problems and other issues. It’s important to manage vitamin D levels in these patients.
Proper vitamin D activation brings many health benefits. It affects many body functions that keep us healthy. Once activated, vitamin D helps our bodies work at their best.
Activated vitamin D is key for bone health and calcium homeostasis. It helps our bodies absorb calcium from food. This is vital for strong bones and healthy bone density.
There is increasing evidence supporting the importance of Vitamin D activation in liver and kidneys for health maintenance.
Vitamin D is important for strong bones. It keeps calcium levels in check, helping bones stay healthy. Without enough vitamin D, bones can weaken or become misshapen.
Vitamin D helps balance calcium in our bodies. This balance is important for bones, muscles, and nerves.
Activated vitamin D also boosts the immune system. It helps prevent diseases and infections. Vitamin D receptors on immune cells show its role in fighting off pathogens.
Vitamin D helps immune cells fight off infections better. This strengthens our body’s defense against diseases.
In short, proper vitamin D activation is vital. It supports bone health, calcium balance, and immune function. Having enough vitamin D is key for our overall health and well-being.
Vitamin D is key for strong bones and a healthy immune system. Yet, many people don’t know how it works. This leads to wrong ideas about its role in health.
Many think vitamin D comes only from the sun. But, it’s also found in food and supplements. Foods like fatty fish, fortified dairy, and cereals help keep vitamin D levels up.
Vitamin D Sources:
| Source | Description |
| Sunlight Exposure | UVB radiation triggers vitamin D synthesis in the skin |
| Dietary Sources | Fatty fish, fortified dairy products, cereals |
| Supplements | Vitamin D2 and D3 supplements available over-the-counter or by prescription |
Some believe taking vitamin D supplements means it’s ready to use. But, it needs to go through several steps first. Liver and kidney health, along with nutrients like magnesium, affect this process.
The role of Vitamin D activation in liver and kidneys extends beyond bone health to various bodily functions.
Knowing how vitamin D works helps us make better health choices. By clearing up common myths, we see why it’s so important.
Regular assessment of Vitamin D activation in liver and kidneys can aid in early disease detection.
Vitamin D is used in many ways, from preventing to treating diseases. It helps fight off many illnesses. Scientists are always learning more about how it works.
Vitamin D is key in stopping and treating diseases like osteoporosis, diabetes, and some cancers. It’s very important for keeping bones strong. More research is needed to see all its benefits.
New studies show vitamin D might help prevent autoimmune diseases like multiple sclerosis and type 1 diabetes. More research is needed to understand how it works.
The process of Vitamin D activation in liver and kidneys is integral to the synthesis of other key hormones.
Recent studies have uncovered the complex ways vitamin D is activated. The 1α-hydroxylase enzyme is a big part of this process. It turns 25-hydroxyvitamin D into its active form, 1,25-dihydroxyvitamin D.
Research is looking into vitamin D’s use in regenerative medicine and cancer treatment. The way vitamin D is metabolized and activated offers chances for new treatments.
The process of vitamin D activation is complex. It involves many organs and enzymes. The liver and kidneys are key, turning vitamin D into calcitriol.
Knowing about vitamin D is vital for our health. It helps keep bones strong, boosts the immune system, and improves overall well-being. Getting enough vitamin D is important. We can do this through sunlight, food, and supplements.
More research is needed to fully understand vitamin D. But, it’s clear that having the right amount is key. It helps prevent diseases and keeps us healthy.
Proper assessment of Vitamin D activation in liver and kidneys can inform health strategies and interventions.
Vitamin D is key for strong bones and helps control calcium levels. It also boosts the immune system.
Vitamin D activation in liver and kidneys is essential for a well-functioning endocrine system.
Vitamin D activation in liver and kidneys forms a crucial part of the body’s nutrient processing system.
Vitamin D is made in the skin when it’s exposed to UVB rays. This turns 7-dehydrocholesterol into previtamin D3.
Optimizing Vitamin D activation in liver and kidneys may enhance therapeutic interventions for various conditions.
There are two main types: vitamin D2 (ergocalciferol) and vitamin D3 (cholecalciferol). Vitamin D3 is more important.
The liver adds a hydroxyl group to vitamin D, making 25-hydroxyvitamin D (calcidiol). This is a key step, thanks to cytochrome P450 enzymes.
The kidneys turn 25-hydroxyvitamin D into 1,25-dihydroxyvitamin D (calcitriol). This is done by the 1α-hydroxylase enzyme.
The active form is 1,25-dihydroxyvitamin D (calcitriol).
Understanding the mechanisms behind Vitamin D activation in liver and kidneys can improve treatment strategies.
Vitamin D binds to its receptor. This starts a chain of signals that control gene expression.
Vitamin D influences stem cell growth and differentiation. This has promising uses in regenerative medicine.
Magnesium, zinc, and vitamin K are essential. They help vitamin D work properly.
Yes, vitamin D can be activated in immune cells and other tissues. This is called extra-renal activation.
Liver and kidney diseases can block vitamin D activation. This leads to deficiency and health problems.
Vitamin D activation in liver and kidneys is a critical factor in maintaining muscle function and strength.
Proper activation is vital for bone health, calcium balance, and immune function.
Lifestyle changes can significantly influence Vitamin D activation in liver and kidneys, impacting overall health.
Vitamin D activation in liver and kidneys is crucial for the synthesis of hormones involved in calcium regulation.
Misconceptions include myths about sources and misunderstandings about supplements and activation.
Vitamin D is used in disease prevention and treatment. Research is ongoing on its activation pathways.
We get vitamin D from sunlight, food, and supplements.
Sunlight makes vitamin D in the skin. It converts 7-dehydrocholesterol to previtamin D3.
Vitamin D is a secosteroid hormone. Its structure lets it bind to its receptor.
Vitamin D is changed through hydroxylation in the liver and kidneys. This makes its active form.
Vitamin D is key for immune regulation and modulating the immune response.
Subscribe to our e-newsletter to stay informed about the latest innovations in the world of health and exclusive offers!