Last Updated on December 2, 2025 by Bilal Hasdemir
Obesity affects over 40% of adults in the United States. This has led to a growing need for effective weight management solutions. Comparing the long-term potential of Weight Loss Drugs vs. Bariatric Surgery for sustained obesity treatment.
Recent advancements in obesity treatment have sparked debate. The question is whether weight loss drugs could replace bariatric surgery.
The rising prevalence of obesity has driven the need for new treatments. Both weight loss drugs and bariatric surgery show promising results.
Key Takeaways
- Obesity rates continue to rise, driving demand for effective treatments.
- Weight loss drugs and bariatric surgery are two prominent obesity treatment options.
- The effectiveness and safety profiles of these treatments are being closely compared.
- Recent advancements in weight loss drugs have sparked debate about their potential to replace bariatric surgery.
- Bariatric surgery has been a long-standing solution for severe obesity.
The Obesity Epidemic in America
The obesity epidemic in America is growing, affecting health and the economy. It’s a complex issue that impacts individuals, communities, and healthcare systems.
Current Prevalence and Trends
The U.S. Centers for Disease Control and Prevention (CDC) reports that 40.3% of Americans are obese. Another 9.4% are severely obese. These numbers show how serious the problem is. Obesity is not just a personal issue but a major public health concern.
Obesity affects different groups differently. Age, income, and where you live all play a part. These factors influence who is more likely to be obese.
Health and Economic Impact
Obesity greatly increases the risk of diseases like diabetes and heart disease. “Obesity is a major risk factor for numerous health conditions, making it a significant burden on the healthcare system.” It also costs the economy billions of dollars each year.
A study found that
“The total economic burden of obesity in the United States was estimated to be around $1.72 trillion in 2016, highlighting the substantial economic impact of this health issue.”
The costs of obesity include medical bills and lost productivity. Fighting obesity is key to better health and saving money.
- Obesity increases the risk of chronic diseases.
- It has significant economic implications.
- The prevalence of obesity varies across demographics.
Traditional Approaches to Weight Management
For a long time, people have tried to manage their weight with diet and exercise. These methods are often the first step against obesity. They focus on changing your lifestyle and sometimes involve medical help.
Diet and Lifestyle Modifications
Changing what you eat and moving more are key parts of traditional weight management. Doctors suggest eating less and more fruits, veggies, and whole grains. Lifestyle modifications also mean making behavioral changes, like keeping a food diary and exercising regularly.
But, making these changes can be hard to keep up. Many people find it tough to stick with these changes, leading to weight gain again.
Medical Interventions
When diet and exercise aren’t enough, medical help might be needed. This can include pharmacological treatments to help with weight loss. These medicines work by reducing hunger or changing how the body absorbs nutrients. They’re usually for people with a BMI of 30 or higher, or those with a BMI of 27 or higher and health problems related to obesity.
Limitations of Conservative Approaches
Even though they’re common, traditional weight management methods don’t work for everyone, mainly those with severe obesity. Obesity is complex, involving genetics, hormones, and environment. So, a single approach doesn’t work for everyone. Many people regain weight after losing it, showing the need for better treatments.
This highlights the need to look into other options, like bariatric surgery and new weight loss medicines. These might offer lasting solutions for those dealing with obesity.
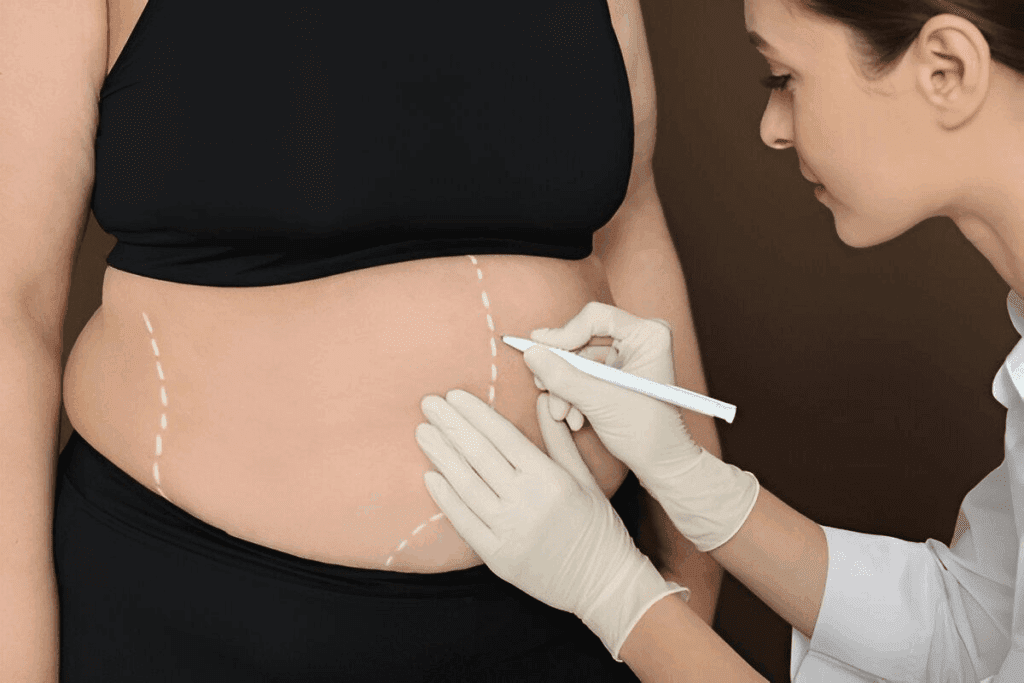
Understanding Bariatric Surgery
Bariatric surgery is a powerful tool for those fighting obesity. It offers a big chance for weight loss and better health. This surgery has changed many lives for the better.
Types of Procedures
There are many types of bariatric surgery, each with its own benefits. Here are some of the most common:
- Sleeve Gastrectomy: This surgery removes a big part of the stomach, leaving a narrow tube-like stomach.
- Gastric Bypass: It makes a small pouch from the stomach and connects it to the small intestine.
- Adjustable Gastric Banding: This is a less invasive option where a band is placed around the stomach.
Each surgery has its own risks and benefits. The right choice depends on the patient’s health and what they prefer.
Mechanism of Action
Bariatric surgery works in several ways to help with weight loss. These include:
- Restriction: Making the stomach smaller to limit how much food you can eat.
- Malabsorption: Changing how food moves through the intestines to reduce nutrient absorption.
- Hormonal Changes: Affecting hunger and fullness hormones to control appetite and metabolism.
Knowing how these mechanisms work helps understand the surgery’s benefits and limits.
Candidate Selection Criteria
Not everyone can have bariatric surgery. The criteria include:
- A Body Mass Index (BMI) of 40 or higher, or a BMI of 35 or higher with obesity-related health conditions.
- Previous weight loss attempts have failed.
- Not having certain medical conditions that could make surgery risky.
- A commitment to making lifestyle changes after surgery.
Choosing the right candidate is a detailed process. A team of healthcare experts carefully evaluates each person.
The Evolution of Weight Loss Medications
Weight loss medications have seen big changes over time. From early failures to recent successes, the journey has been long. The goal has always been to find safe and effective ways to help people lose weight.
Historical Perspective
At first, weight loss drugs had many problems. Some were taken off the market because they were not safe. But these early efforts helped pave the way for today’s research.
In the 1950s and 60s, amphetamines were used to help people lose weight. But they were addictive and their use declined. Later, fenfluramine and dexfenfluramine were introduced but were pulled off the market due to heart problems.
Recent Breakthroughs
Recently, new weight loss drugs have shown great promise. Semaglutide and tirzepatide are two examples. They have been tested in clinical trials and have shown to be effective in helping people lose weight.
These drugs work in new ways. Semaglutide mimics a hormone that helps control hunger. Tirzepatide targets two hormones, which may make it even more effective. These drugs are safer than older ones and offer new hope for those struggling with obesity.
Mechanism of Action
It’s important to understand how these drugs work. Semaglutide and tirzepatide affect hormones that control hunger and fullness. Semaglutide acts like a hormone that helps with glucose and appetite. Tirzepatide works on two hormones, which may make it even better at helping people lose weight.
These drugs show how complex obesity is. They highlight the need for treatments that work in different ways. This is an exciting time for obesity treatment, with new discoveries and treatments on the horizon.
Weight Loss Drugs vs. Bariatric Surgery: Surgery: Effectiveness Comparison
Obesity rates are rising fast. It’s key to compare weight loss drugs and bariatric surgery. Both can help with weight and health issues, but how well they work depends on many things.
A study at the ASMBS 2025 Annual Scientific Meeting showed bariatric surgery leads to five times more weight loss than GLP-1 receptor agonists after two years. This big difference shows bariatric surgery might be a better choice for lasting weight loss for many.
Bariatric surgery usually leads to more weight loss that lasts. The study mentioned above shows surgery is very effective for losing weight. But, newer weight loss drugs like GLP-1 receptor agonists work well too, when used with lifestyle changes.
Improving health issues linked to obesity is also important. Bariatric surgery can greatly help with type 2 diabetes, high blood pressure, and sleep apnea. Weight loss drugs can also help, but the improvement might not be as big as with surgery.
Choosing between weight loss drugs and bariatric surgery depends on the patient’s health, preferences, and goals. Personalized treatment plans are key. They should match the patient’s needs and situation for the best results.
In summary, both weight loss drugs and bariatric surgery have roles in treating obesity. But, the data points to bariatric surgery as a better option for long-term weight loss. Yet, the right choice depends on a full look at the patient’s health and goals.
Safety Profiles and Side Effects
Bariatric surgery and weight loss medications are effective but come with risks. It’s important for healthcare providers and patients to understand these risks. This knowledge helps in making informed decisions about treatment options.
Surgical Complications and Risks
Bariatric surgery, like any surgery, has risks. These include infection, bleeding, and reactions to anesthesia. Specific risks include bowel obstruction, band slippage, and nutritional deficiencies.
A study in a Journal found complication rates between 10% and 17%. Mortality rates are less than 1%. But, risks depend on the surgery type, patient health, and the surgical team’s experience.
Medication Side Effects and Contraindications
Weight loss medications also have side effects and contraindications. Common issues include nausea, diarrhea, and constipation. Serious but rare side effects include increased heart rate and high blood pressure.
For example, phentermine-topiramate can cause paresthesia, dizziness, and bad taste. Medications are contraindicated in pregnancy, certain heart conditions, and substance abuse history.
Medication | Common Side Effects | Contraindications |
Phentermine-Topiramate | Paresthesia, dizziness, dysgeusia | Pregnancy, glaucoma, hyperthyroidism |
Liraglutide | Nausea, diarrhea, constipation | Personal or family history of medullary thyroid carcinoma |
Long-term Safety Considerations
Both bariatric surgery and weight loss medications need long-term monitoring. Surgery requires managing nutritional deficiencies and watching for complications. Medications need monitoring for cardiovascular effects and effectiveness over time.
The choice between surgery and medications depends on the patient’s health, risks, and treatment safety. A thorough evaluation is key.
Cost Considerations and Insurance Coverage
Obesity is becoming more common, making the cost of treatments a big issue. Both patients and healthcare providers worry about the financial side of obesity treatment.
Direct Treatment Costs
The costs of bariatric surgery and weight loss medications differ a lot. Bariatric surgery can cost between $15,000 and $25,000 or more. This depends on the surgery and where it’s done.
Weight loss medications, on the other hand, cost more over time. They can cost between $1,000 and $2,000 a year. This depends on the type of medication and how often it’s taken.
Bariatric surgery costs include:
- Surgical fees
- Hospital stay
- Pre- and post-operative care
Weight loss medication costs, on the other hand, are influenced by:
- Medication type and dosage
- Frequency of prescriptions
- Insurance coverage and copays
Insurance Policies and Coverage Trends
Insurance for obesity treatment has changed. Many insurers now cover bariatric surgery and some weight loss medications. But, coverage can vary a lot.
“The increasing recognition of obesity as a chronic disease has led to greater insurance coverage for evidence-based treatments, including bariatric surgery and certain weight loss medications.”
Insurance coverage is moving towards better support for obesity treatment. This includes:
- Increased coverage for bariatric surgery
- Greater acceptance of weight loss medications as a treatment option
- More emphasis on preventive care and early intervention
Long-term Economic Impact
Looking at the long-term costs of obesity treatment is key. It’s not just about the upfront costs. We also need to think about the savings from better health.
Studies have shown that bariatric surgery can lead to significant long-term cost savings by:
- Reducing healthcare utilization
- Improving comorbid condition management
- Enhancing productivity and quality of life
The long-term economic impact of weight loss medications is also being studied. Factors that affect this include:
- Medication adherence and persistence
- Clinical efficacy and durability
- Potential for cost savings through improved health outcomes
In conclusion, understanding the costs and insurance for obesity treatment is vital. By looking at the direct costs, insurance, and long-term savings, we can make better choices. This helps both patients and healthcare providers find the most effective and affordable treatments.
Patient Experience and Quality of Life
Weight loss is a personal journey. The choice between bariatric surgery and weight loss medications greatly affects a patient’s quality of life. It’s important for healthcare providers to understand this to offer the best care.
Recovery and Lifestyle Adjustments
Recovering from bariatric surgery means big changes in lifestyle. Patients must adapt to a new way of eating and living to keep weight off and stay healthy.
Weight loss medications, on the other hand, require less drastic lifestyle changes. But, they need regular monitoring and might need to be taken for life. The ease of starting medication must be balanced with the commitment to ongoing treatment.
Psychological Impact
The psychological impact of weight loss treatments is deep. Bariatric surgery often improves mental health by reducing weight and improving health conditions.
Weight loss medications also help mental health, but how much varies. Support from healthcare providers is key in managing any psychological impacts.
Patient Satisfaction Rates
Treatment | Patient Satisfaction Rate | Quality of Life Improvement |
Bariatric Surgery | 85% | Significant |
Weight Loss Medications | 70% | Moderate to Significant |
Patient satisfaction rates differ between bariatric surgery and weight loss medications. Surgery often gets higher satisfaction due to more weight loss. Yet, both treatments can greatly improve quality of life.
The choice between bariatric surgery and weight loss medications depends on individual needs and health. Understanding the impacts on patient experience and quality of life helps healthcare providers support patients better.
Regulatory Landscape and Approval Process
It’s important to know about the rules for weight loss drugs and bariatric surgery. These rules help shape how these treatments are developed, approved, and used.
FDA Approval Pathways for Weight Loss Drugs
The FDA has strict steps to check if weight loss drugs are safe and work well. Clinical trials are key, done in phases to test the drug’s effects and side effects.
The FDA looks at many things when reviewing these drugs. They check how the drug works, its dosage, and how it might react with other medicines. They also look at the drug’s effects on people.
FDA Approval Phase | Description | Key Considerations |
Phase 1 | Initial human trials to assess safety | Dosage, pharmacokinetics |
Phase 2 | Trials to evaluate efficacy and side effects | Efficacy, safety, optimal dosage |
Phase 3 | Large-scale trials to confirm efficacy and monitor side effects | Long-term safety, efficacy in diverse populations |
Surgical Procedure Standards and Regulations
Bariatric surgery must follow strict rules to keep patients safe. Surgical procedure guidelines are set by experts and regulators to ensure consistent care.
These rules cover things like pre-operative evaluation, how the surgery is done, and aftercare. Following these rules is key to reducing risks and improving results.
Future Regulatory Considerations
As obesity treatment changes, so will the rules. New trends, like combination therapies and new medicines, will need new rules.
The future might see more detailed checks on weight loss treatments. This could include using real-world evidence and long-term data.
Healthcare Provider Perspectives
As obesity rates keep going up, healthcare providers are changing their ways. They now use both surgery and medicine to help people lose weight. This change is because they need ways to help people lose weight for good.
Changing Prescribing Patterns
Doctors are now thinking about weight loss medicines more often. New medicines are safer and offer more options for treatment.
- GLP-1 receptor agonists, like semaglutide, are showing great promise in studies.
- Doctors are looking into combining medicines to make them work better and have fewer side effects.
Treatment Recommendation Factors
Doctors look at many things when deciding on treatments. They think about the patient’s health, how much weight they want to lose, and the risks of different treatments.
Factor | Considerations | Impact on Decision |
Patient Health Status | Presence of comorbidities, previous weight loss attempts | High |
Weight Loss Goals | Amount of weight to be lost, timeline for weight loss | Medium |
Potential Risks | Surgical complications, medication side effects | High |
Interdisciplinary Approaches
Dealing with obesity is complex. That’s why doctors are working together with dietitians, psychologists, and others. They see the value in teamwork.
By working together, doctors can give patients better, tailored plans. This not only helps patients but also makes care better overall.
Patient Selection: Who Benefits Most from Each Approach?
Choosing the right treatment for obesity is key. It depends on many things like health, mind, and how treatments fit each person. This is where personalized medicine comes in.
Clinical Factors Influencing Treatment Choice
Health matters a lot when picking a treatment. Things like BMI, health problems, and past weight loss efforts are important. For example, those with a high BMI or who haven’t lost weight before might do better with surgery.
Health issues can also guide the choice between drugs and surgery. For instance, people with severe stomach problems might not be good candidates for some medicines.
Clinical Factor | Weight Loss Drugs | Bariatric Surgery |
BMI | Suitable for BMI ≥ 30 | Typically considered for BMI ≥ 40 or ≥ 35 with comorbidities |
Comorbidities | Can be used in presence of certain comorbidities | Often recommended for patients with significant comorbidities |
Previous Weight Loss Attempts | Ideal for those who have not tried surgery | Considered for those who have failed other weight loss methods |
Psychological and Behavioral Considerations
Mind and behavior are also important. Mental health, motivation, and sticking to lifestyle changes matter a lot. For example, those with eating disorders need careful treatment.
Behavioral assessments help find who will do best with a treatment. They look at eating, exercise, and mental readiness for weight loss.
Personalized Medicine Approaches
The future is in personalized medicine. Treatments will be made just for each person. Genetic tests and biomarkers will help figure out who will respond best to what.
Healthcare providers will make better choices by looking at both health and mind. This way, they can pick the best treatment for each patient.
Emerging Combination Therapies
Combination therapies are becoming a key strategy in fighting obesity. They mix weight loss drugs with surgery. This combo aims to boost the benefits of both methods for better results.
Pre-surgical Medication Protocols
Before bariatric surgery, patients take weight loss meds. This can lower BMI and cut down on surgery risks. Research shows that losing weight before surgery can lead to fewer problems during and after the operation.
The perks of pre-surgery meds include:
- Smaller liver size, making surgery easier
- Better metabolic health, lowering surgery risks
- Better choice of patients for surgery with more weight loss
Post-surgical Pharmacological Support
After bariatric surgery, weight loss meds help keep weight off. This is important because weight gain is common after surgery. Keeping up with meds after surgery helps patients lose weight for good.
A study showed that:
Treatment Approach | Average Weight Loss | Weight Regain Rate |
Bariatric Surgery Alone | 25% | 30% |
Bariatric Surgery with Post-surgical Medication | 35% | 15% |
Integrated Treatment Models
Integrated models mix medical, surgical, and lifestyle treatments for obesity care. They see obesity as a complex disease needing many treatments.
By combining different treatments, doctors can tailor care to each patient. This approach may lead to better long-term results.
Future Innovations and Research Directions
The field of obesity treatment is on the verge of a big change. New weight loss medications and surgical methods are being developed. These advancements aim to make treatments more effective, safe, and accessible.
Next-Generation Weight Loss Medications
New weight loss medications are being researched. These drugs target different ways the body regulates weight. They might work better and have fewer side effects. Some promising areas include:
- Dual-action therapies that combine the effects of existing medications
- Novel targets that address the underlying causes of obesity
- Improved delivery methods, such as sustained-release formulations
Advances in Surgical Techniques
Surgical methods for obesity treatment are also getting better. New technologies and techniques aim to reduce recovery times and improve weight loss results. Some key developments include:
Technique | Description | Benefits |
Robotic-assisted surgery | Uses robotic systems for better precision and control | Less recovery time, less blood loss |
Laparoscopic procedures | Minimally invasive, reduces tissue damage | Less pain, quicker recovery |
Single-incision surgery | Performs surgery through one incision, less scarring | Improved looks, less risk of problems |
Novel Treatment Paradigms
New treatment methods are being explored. They combine medications, surgery, and behavioral therapies. This integration aims to achieve better weight loss and health. The benefits include:
- More effective weight loss
- Improved metabolic health
- Better control of related health issues
As research continues, these innovations will be key in the future of obesity treatment. They offer hope for those struggling with weight management.
Conclusion: The Future of Obesity Treatment
The way we treat obesity is changing. Weight loss drugs and bariatric surgery are becoming key parts of treatment. As obesity rates keep going up in the U.S., it’s important to understand these treatments well.
Weight loss drugs and bariatric surgery each have their own benefits and drawbacks. Bariatric surgery can lead to big weight loss and health improvements. But, it’s a major surgery with risks. On the other hand, weight loss drugs are less invasive but their success can vary, and long-term safety is being studied.
The future of treating obesity might involve using both drugs and surgery, depending on the patient. New research and advancements in both areas are promising. Healthcare professionals will need to keep up with these changes to help patients with obesity the best way possible.
FAQ
What is the current prevalence of obesity in America?
The CDC reports that over 40% of adults in the United States are obese. This has big health and economic effects.
How effective are traditional weight management strategies for severe obesity?
Diet and lifestyle changes often don’t work well for severe obesity. This shows we need other treatments.
What are the different types of bariatric surgery procedures?
Bariatric surgery includes gastric bypass, sleeve gastrectomy, and adjustable gastric banding. Each has its own way of working and who it’s for.
How do weight loss medications work?
Weight loss medications reduce appetite, block fat absorption, and change metabolism. New breakthroughs are making them more effective.
How do weight loss drugs compare to bariatric surgery in terms of effectiveness?
Studies show bariatric surgery can lead to more weight loss than medications. But, both can work for some patients.
What are the possible complications and side effects of bariatric surgery and weight loss medications?
Bariatric surgery can have surgery risks. Medications might cause nausea, diarrhea, and a faster heart rate, among other side effects.
What are the long-term safety considerations for weight loss medications?
We’re just starting to learn about the long-term safety of weight loss medications. Ongoing monitoring is needed to understand their safety fully.
How do the costs of bariatric surgery and weight loss medications compare?
Bariatric surgery is usually more expensive at first. Medications have ongoing costs. Insurance and out-of-pocket expenses vary a lot.
What factors influence the choice between weight loss drugs and bariatric surgery?
What treatment is best depends on many things. This includes health, behavior, and what the patient wants.
What is the possible for combination therapies in obesity treatment?
Research shows combining medications with surgery might improve results. But, more study is needed to know the benefits and challenges.
What are the future trends in obesity treatment?
New medications, better surgery techniques, and new treatment ideas are coming. They offer hope for those fighting obesity.
How do healthcare providers recommend treatments for obesity?
Doctors look at many things when choosing a treatment. This includes the patient’s health, goals, and what research says.
What is the role of patient education in obesity treatment?
Teaching patients about their options is key. It helps them make good choices and lose weight successfully.
How do insurance policies and coverage trends impact access to obesity treatments?
Insurance and how it pays for treatments affects who can get them. Advocacy efforts aim to improve coverage.
What are the implications of the comparison between weight loss drugs and bariatric surgery for the future of obesity treatment?
The comparison shows we need a wide range of treatments for obesity. Both medications and surgery are important.
References
New England Journal of Medicine. Evidence-Based Medical Insight. Retrieved from https://www.nejm.org/doi/full/10.1056/nejmoa1600869





