Last Updated on November 26, 2025 by Bilal Hasdemir

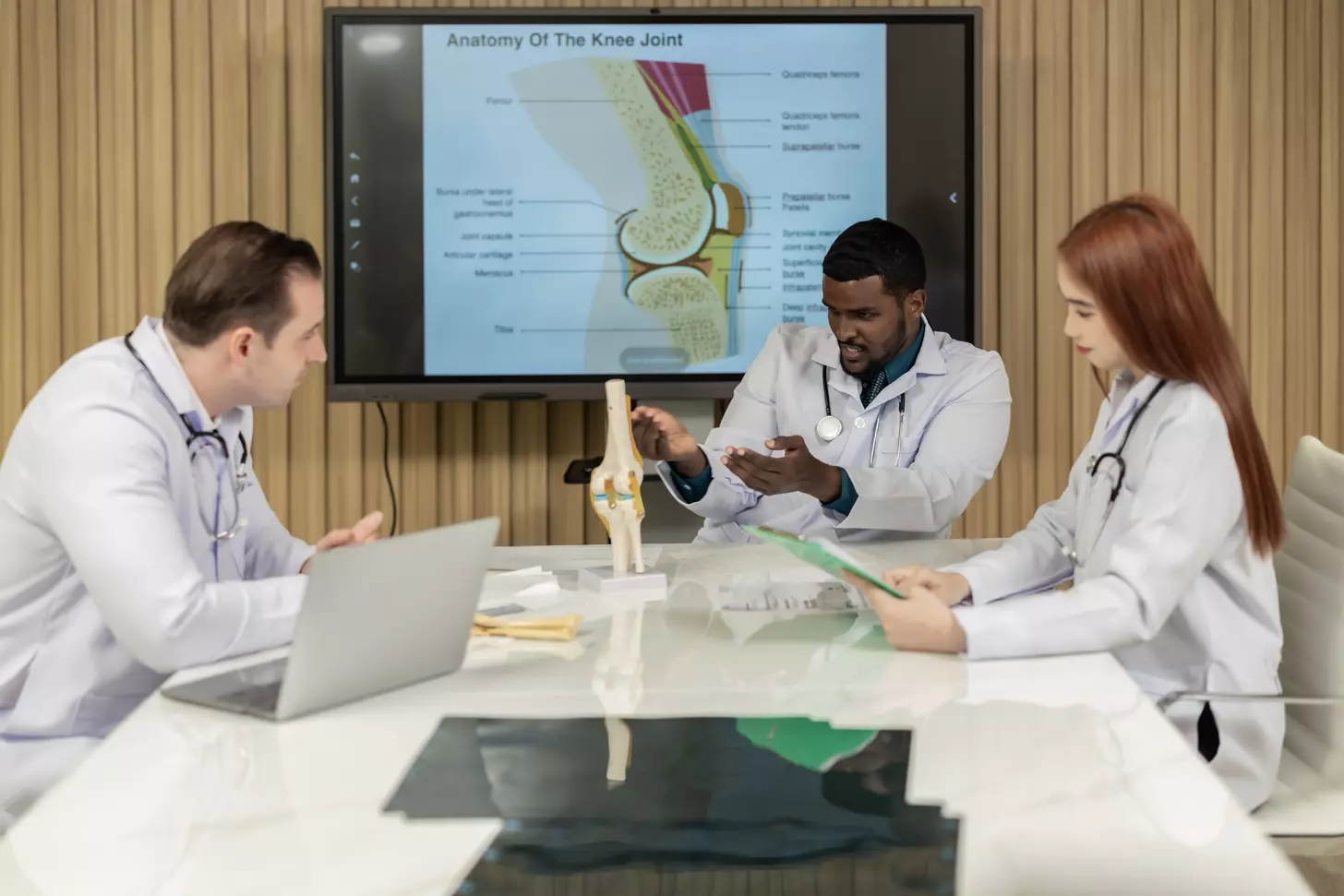
For patients facing stomach or ovarian cancer, understanding treatment options like intraperitoneal chemotherapy is crucial. At Liv Hospital, we provide world-class care, ensuring every diagnosis is met with the latest evidence-based therapies and a patient-centered approach.
Intraperitoneal chemotherapy involves delivering anticancer drugs directly into the peritoneal cavity, where the cancer is located. This method allows for a higher concentration of chemotherapy to be applied directly to the tumor site, potentially improving treatment outcomes.
Unlike traditional chemotherapy, intraperitoneal chemotherapy targets the cancer more precisely, which may reduce side effects and enhance effectiveness for certain patients.
Key Takeaways
- Intraperitoneal chemotherapy delivers anticancer drugs directly into the peritoneal cavity.
- This method is used to treat stomach and ovarian cancer.
- It allows for a higher concentration of chemotherapy at the tumor site.
- Intraperitoneal chemotherapy may reduce side effects compared to traditional chemotherapy.
- Liv Hospital provides advanced care with a patient-centered approach.
Defining Chemo Shots in Stomach: The Basics of Intraperitoneal Therapy

The concept of ‘chemo shots in the stomach’ refers to intraperitoneal chemotherapy, a method that involves administering chemotherapy drugs directly into the peritoneal cavity. This approach allows for higher concentrations of the drug to be in contact with the cancer cells in the abdomen, potentially increasing the effectiveness of the treatment.
Intraperitoneal (IP) chemotherapy is a specialized form of cancer treatment that has gained attention for its potential to improve outcomes in patients with certain types of cancer, particularly those involving the peritoneum, such as ovarian and stomach cancers.
What Makes IP Chemotherapy Different from Traditional Methods
Unlike traditional intravenous chemotherapy, where drugs are administered through a vein and distributed throughout the body, IP chemotherapy delivers drugs directly to the site of the cancer. This localized approach can lead to higher drug concentrations at the tumor site, potentially improving the efficacy of the treatment while minimizing systemic side effects.
“Intraperitoneal chemotherapy represents a significant advancement in the treatment of cancers that are confined to or predominantly affect the peritoneal cavity,” says a leading oncologist. “By delivering chemotherapy directly to the tumor site, we can potentially achieve better outcomes for our patients.”
The Evolution of Direct Peritoneal Cancer Treatment
The development of IP chemotherapy marks a significant evolution in the treatment of peritoneal cancers. Initially used primarily for ovarian cancer, this method has expanded to include other cancers that affect the peritoneum. The technique has been refined over the years to improve its safety and efficacy, offering new hope to patients with these challenging diagnoses.
As research continues, we are learning more about the benefits and challenges of IP chemotherapy, including its potential to be used in combination with other treatments to enhance patient outcomes.
The Science Behind Intraperitoneal Chemotherapy Delivery
The delivery of chemotherapy directly into the peritoneal cavity is a complex process that has shown promising results in treating certain types of cancer. This method involves administering drugs into the abdominal cavity, where they can directly target cancer cells on the surfaces of the peritoneum, intestines, and other internal organs.
How Drugs Target Cancer Cells in the Peritoneal Cavity
Intraperitoneal chemotherapy works by delivering high concentrations of drugs directly to the cancer cells within the peritoneal cavity. This targeted approach allows for a more effective attack on cancer cells while minimizing the impact on healthy tissues elsewhere in the body.
The peritoneal cavity is lined with a thin membrane called the peritoneum, which can be a site for cancer metastasis, particularly in cancers such as ovarian cancer. By administering chemotherapy directly into this cavity, we can achieve higher local drug concentrations that are more effective at killing cancer cells.
Achieving Higher Drug Concentrations at Tumor Sites
Studies have shown that intraperitoneal chemotherapy can achieve significantly higher drug concentrations at the tumor site compared to intravenous administration. This is because the drugs are not diluted in the bloodstream before reaching the tumor, allowing for a more potent effect.
The pharmacokinetics of intraperitoneal chemotherapy involve the drug being absorbed into the tissues surrounding the peritoneal cavity, including cancerous tumors. This direct exposure results in improved efficacy against tumors that are resistant to traditional intravenous chemotherapy.
Intraperitoneal Port Systems: Your Gateway for Treatment
Intraperitoneal port systems play a crucial role in the administration of chemotherapy directly into the peritoneal cavity. These systems are designed to provide a safe and effective way to deliver treatment, minimizing the discomfort and complications associated with repeated injections.
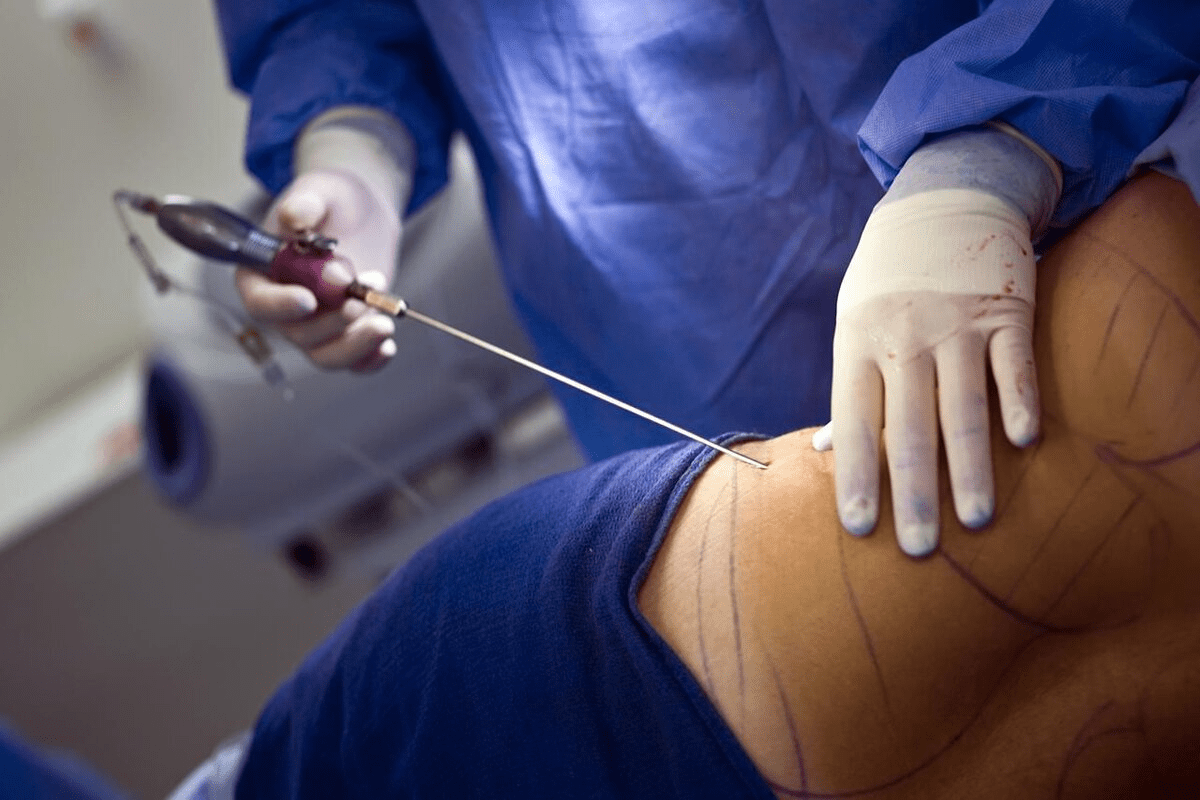
Implantation Process and Techniques
The implantation of an intraperitoneal port involves a minor surgical procedure, typically performed under local anesthesia. The port is placed under the skin, usually in the upper chest area, and a catheter is guided into the peritoneal cavity. Precision and care are essential during this process to ensure proper placement and minimize the risk of complications.
The technique used for port placement can vary depending on the patient’s anatomy and the physician’s preference. Imaging guidance, such as ultrasound or fluoroscopy, may be used to assist in the accurate placement of the catheter.
Living With and Caring for Your IP Port
Living with an intraperitoneal port requires some adjustments, but with proper care, patients can minimize the risk of complications. Regular flushing of the port is necessary to prevent blockages, and patients are taught how to care for their port at home.
It’s essential to monitor the port site for signs of infection, such as redness, swelling, or pain. Patients should also be aware of the potential for other complications, including catheter malfunction or leakage.
| Care Activity | Frequency | Purpose |
|---|---|---|
| Flushing the port | Every 4-6 weeks | Prevent blockages |
| Inspecting the port site | Daily | Monitor for infection |
| Dressing changes | As needed | Maintain cleanliness |
By understanding the role of intraperitoneal port systems and how to care for them, patients can navigate their treatment with greater confidence and comfort.
Cancer Types That Benefit from IP Chemotherapy
Intraperitoneal chemotherapy has emerged as a crucial treatment option for specific types of cancer, particularly ovarian and stomach cancers. This method involves delivering chemotherapy drugs directly into the peritoneal cavity, where the cancer is located, allowing for higher concentrations of the drug to be in contact with the tumor cells.
We will explore how intraperitoneal chemotherapy is used to treat different types of cancer, focusing on the benefits and outcomes for patients with ovarian and stomach cancers.
Intraperitoneal Chemotherapy for Ovarian Cancer
Ovarian cancer is one of the primary indications for intraperitoneal chemotherapy. Studies have shown that IP chemotherapy can significantly improve survival rates for patients with advanced ovarian cancer. The rationale behind using IP chemotherapy for ovarian cancer lies in the fact that this type of cancer tends to remain localized within the peritoneal cavity for a considerable period.
By delivering chemotherapy drugs directly into the peritoneal cavity, we can achieve higher drug concentrations at the tumor site, leading to more effective killing of cancer cells. Clinical trials have demonstrated that patients receiving IP chemotherapy for ovarian cancer have improved progression-free survival and overall survival compared to those receiving intravenous chemotherapy alone.
Treating Stomach Cancer and Gastrointestinal Malignancies
In addition to ovarian cancer, intraperitoneal chemotherapy is also used to treat stomach cancer and other gastrointestinal malignancies. These cancers often spread within the peritoneal cavity, making IP chemotherapy a suitable treatment approach.
The benefits of IP chemotherapy for stomach cancer include the ability to deliver high doses of chemotherapy directly to the tumor site, reducing the risk of systemic side effects. This approach has shown promise in improving outcomes for patients with advanced stomach cancer.
To illustrate the effectiveness of IP chemotherapy for different types of cancer, let’s examine the following table:
| Cancer Type | IP Chemotherapy Benefits | Clinical Outcomes |
|---|---|---|
| Ovarian Cancer | Higher drug concentrations at tumor site, improved survival rates | Improved progression-free survival and overall survival |
| Stomach Cancer | High doses of chemotherapy directly to tumor, reduced systemic side effects | Improved outcomes for advanced stomach cancer patients |
| Gastrointestinal Malignancies | Effective for cancers spreading within the peritoneal cavity | Potential for improved survival and reduced recurrence |
As shown in the table, intraperitoneal chemotherapy offers various benefits for different types of cancer, leading to improved clinical outcomes for patients.
Chemotherapy Agents Used in IP Treatment Protocols
Intraperitoneal chemotherapy protocols often involve the use of specific chemotherapy agents tailored to the patient’s cancer type. The choice of these agents is critical in determining the effectiveness of the treatment. We will explore the most commonly used chemotherapy agents in IP therapy and how they are selected for different cancer scenarios.
Paclitaxel and Platinum-Based Drugs in IP Therapy
Paclitaxel and platinum-based drugs are among the most frequently used chemotherapy agents in intraperitoneal treatment protocols. Paclitaxel is a taxane that works by inhibiting cell division, thereby preventing the growth of cancer cells. Platinum-based drugs, including cisplatin and carboplatin, function by damaging the DNA of cancer cells, which ultimately leads to cell death.
The combination of paclitaxel and platinum-based drugs has shown significant efficacy in treating various types of cancers, particularly ovarian cancer. Studies have demonstrated that this combination can improve survival rates and reduce the risk of recurrence.
“The intraperitoneal administration of paclitaxel and cisplatin has been shown to improve survival in patients with advanced ovarian cancer.”
Selecting the Right Drugs for Different Cancer Scenarios
The selection of chemotherapy agents for IP therapy depends on several factors, including the type of cancer, the stage of the disease, and the patient’s overall health. For instance, paclitaxel is often used in the treatment of ovarian cancer, while platinum-based drugs are commonly used for a variety of gastrointestinal malignancies.
| Cancer Type | Commonly Used Chemotherapy Agents |
|---|---|
| Ovarian Cancer | Paclitaxel, Cisplatin |
| Gastrointestinal Malignancies | Oxaliplatin, Carboplatin |
Understanding the specific chemotherapy agents used in IP treatment protocols and their applications in different cancer scenarios is crucial for healthcare providers to make informed treatment decisions. By tailoring the treatment to the individual patient’s needs, we can optimize outcomes and improve the quality of life for patients undergoing intraperitoneal chemotherapy.
HIPEC: Hyperthermic Intraperitoneal Chemotherapy Explained
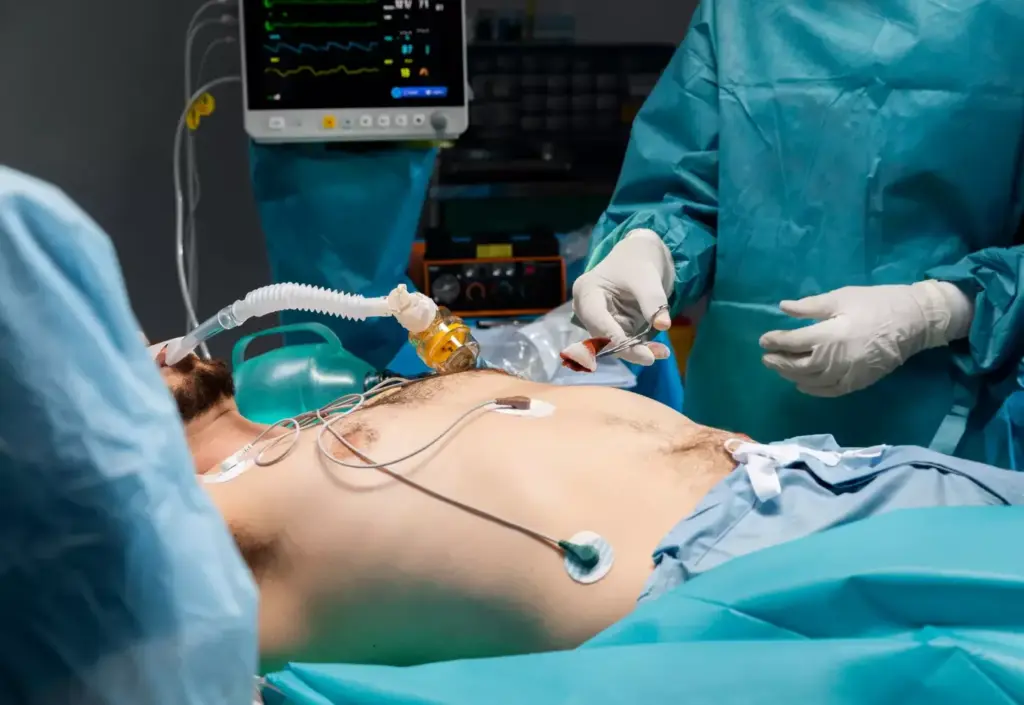
Hyperthermic Intraperitoneal Chemotherapy, or HIPEC, represents a groundbreaking approach in cancer treatment, combining the effectiveness of heated chemotherapy with surgical precision. This innovative therapy is designed for patients with specific types of cancer that are confined to the abdominal cavity.
HIPEC is typically performed in conjunction with a surgical procedure known as cytoreductive surgery, where the surgeon removes visible tumor nodules from the abdominal cavity. Following the surgical removal of tumors, heated chemotherapy drugs are circulated directly within the peritoneal cavity to target any remaining cancer cells.
The Surgical Procedure and Administration Process
The administration of HIPEC involves several key steps. First, the surgeon performs cytoreductive surgery to remove as much of the tumor as possible. Once the visible tumors are removed, the heated chemotherapy solution is pumped into the abdominal cavity through specialized equipment. The chemotherapy is heated to a temperature slightly higher than normal body temperature, typically around 42°C (107.6°F), to enhance its penetration and effectiveness against cancer cells.
The heated chemotherapy is circulated throughout the abdominal cavity for a specified duration, usually about 60 to 90 minutes, to ensure thorough coverage of all surfaces. This process allows the chemotherapy to directly target cancer cells that may remain after surgery, potentially improving treatment outcomes.
How Heat Enhances Chemotherapy Effectiveness
The application of heat during HIPEC serves several purposes. Firstly, it increases the penetration of chemotherapy drugs into tissues, allowing for a more effective targeting of cancer cells. Secondly, heat enhances the cytotoxic effects of chemotherapy, making cancer cells more susceptible to the treatment. Lastly, the hyperthermic condition can stimulate an immune response against cancer cells, potentially providing additional anti-tumor benefits.
The combination of surgical removal of tumors and HIPEC represents a comprehensive approach to treating certain types of abdominal cancers. By directly targeting cancer cells with heated chemotherapy, HIPEC offers a promising therapeutic strategy for improving patient outcomes.
| Key Components of HIPEC | Description | Benefits |
|---|---|---|
| Cytoreductive Surgery | Surgical removal of visible tumors | Reduces tumor burden |
| Heated Chemotherapy | Chemotherapy drugs heated to 42°C | Enhances drug penetration and effectiveness |
| Circulation Process | Heated chemotherapy circulated in the abdominal cavity for 60-90 minutes | Targets remaining cancer cells |
Combining IP and IV Chemotherapy: A Dual Approach
For certain types of cancer, doctors often recommend a dual approach using both IP and IV chemotherapy. This combined strategy leverages the strengths of both methods to provide a more comprehensive treatment plan.
Rationale Behind Multiple Treatment Methods
Doctors recommend combining IP and IV chemotherapy because it allows for a multi-faceted attack on cancer cells. IV chemotherapy circulates throughout the body, targeting cancer cells that may have spread beyond the original site. In contrast, IP chemotherapy delivers drugs directly into the peritoneal cavity, where certain cancers are more likely to recur.
Key benefits of this dual approach include:
- Enhanced effectiveness against tumors within the peritoneal cavity
- Ability to target cancer cells that have spread systemically
- Potential for improved patient outcomes through a comprehensive treatment strategy
Typical Treatment Schedules and Duration
The treatment schedule for combined IP and IV chemotherapy can vary depending on the type of cancer, the stage of the disease, and the patient’s overall health. Typically, treatment cycles range from 3 to 6 weeks, with IP chemotherapy administered every 3 weeks and IV chemotherapy given on a weekly or every-other-week schedule.
Here’s an example of a typical treatment schedule:
| Treatment Cycle | Week 1 | Week 2 | Week 3 |
|---|---|---|---|
| Cycle 1 | IV Chemotherapy | IV Chemotherapy | IP Chemotherapy |
| Cycle 2 | IV Chemotherapy | IV Chemotherapy | IP Chemotherapy |
The duration of the combined treatment can last several months, typically ranging from 4 to 6 months. The exact duration depends on the patient’s response to the treatment and their ability to tolerate the therapy.
Understanding “Chemo Belly” and Abdominal Side Effects
Abdominal side effects, including swelling and discomfort, are common among patients receiving intraperitoneal chemotherapy, a condition often termed “chemo belly.” This phenomenon is a significant concern for many patients undergoing this treatment. We will explore the symptoms, causes, and recovery timeline associated with “chemo belly” to better understand this condition.
Symptoms and Causes of Peritoneal Inflammation
The symptoms of “chemo belly” can vary among patients but typically include abdominal swelling, discomfort, and pain. These symptoms are often a result of peritoneal inflammation caused by the chemotherapy drugs administered directly into the abdominal cavity. The inflammation can lead to the accumulation of fluid, further contributing to the discomfort and swelling.
Peritoneal inflammation is a common side effect of intraperitoneal chemotherapy. The chemotherapy agents can irritate the peritoneal lining, leading to inflammation and the associated symptoms. Understanding the causes and symptoms is crucial for managing and mitigating these side effects.
Does Chemo Belly Go Away? Timeline for Recovery
The recovery timeline for “chemo belly” can vary depending on several factors, including the type of chemotherapy used, the dosage, and individual patient response. In many cases, the symptoms of “chemo belly” can resolve once the treatment is completed. However, the timeline for recovery can differ significantly among patients.
For some patients, the symptoms may start to subside shortly after the completion of intraperitoneal chemotherapy, while for others, it may take longer. It’s essential for patients to discuss their specific situation and any concerns with their healthcare provider. Patients undergoing intraperitoneal chemotherapy for ovarian cancer may find additional information on managing their condition and related side effects on our website, https://int.livhospital.com/do-you-lose-weight-with-ovarian-cancer/.
| Symptom | Typical Duration | Management Strategies |
|---|---|---|
| Abdominal Swelling | Several weeks to months | Drainage, medication |
| Discomfort/Pain | Variable, often resolves with treatment completion | Pain management medication, rest |
| Peritoneal Inflammation | Typically resolves with treatment completion | Anti-inflammatory medication, monitoring |
Intravenous vs. Intraperitoneal Chemotherapy Side Effects
When comparing intravenous and intraperitoneal chemotherapy, understanding their side effects is crucial for patients. Both methods are used to treat various cancers, but they differ in how the chemotherapy is administered and how it affects the body.
Common Side Effects Shared by Both Methods
Both intravenous and intraperitoneal chemotherapy can cause similar side effects due to the nature of the treatment. Some of these common side effects include:
- Fatigue
- Nausea and vomiting
- Hair loss
- Increased risk of infection
- Bleeding or bruising easily
As stated by the American Cancer Society, “Chemotherapy can cause side effects, which can vary depending on the type of drugs used, the dose, and the length of treatment.”
Unique Challenges of IP Treatment and How to Address Them
Intraperitoneal chemotherapy has its unique set of challenges due to its direct delivery into the peritoneal cavity. Some of these challenges include:
- Abdominal pain or discomfort
- Infection at the port site
- Bowel complications
- Potential for catheter-related issues
Managing these side effects is crucial for the success of the treatment. “The key to successful IP chemotherapy is careful patient selection, meticulous technique, and attentive care to minimize complications,” emphasizes the importance of a multidisciplinary approach to IP chemotherapy.
To address these challenges, patients should work closely with their healthcare team to monitor their condition and adjust the treatment plan as needed. This may include pain management strategies, infection prevention measures, and dietary adjustments to minimize bowel complications.
The Patient Journey Through IP Chemotherapy Treatment
The journey through IP chemotherapy begins with preparation, and we’re here to guide you through every step of the way. As you embark on this significant treatment journey, understanding what to expect can greatly enhance your experience.
Preparing for Your First IP Chemotherapy Session
Preparing for your first IP chemotherapy session involves several important steps. It’s crucial to follow your doctor’s instructions carefully and ask any questions you may have about the process. We recommend that you:
- Arrange for support: Having a friend or family member accompany you to the session can provide emotional support and help with transportation.
- Plan your logistics: Understand the treatment schedule, including the duration of the session and any necessary follow-up appointments.
- Prepare your home: Ensure you have any necessary supplies or medications at home to manage potential side effects.
Self-Care Strategies Between Treatments
Self-care is vital during IP chemotherapy treatment. Maintaining a healthy lifestyle can help mitigate some of the side effects and improve your overall well-being. Consider the following self-care strategies:
- Nutrition: Focus on a balanced diet rich in nutrients to help your body recover between treatments.
- Rest: Ensure you get plenty of rest and allow your body time to recover.
- Stay hydrated: Drink plenty of fluids to help flush out the chemotherapy drugs.
- Manage stress: Engage in stress-reducing activities such as meditation, yoga, or deep breathing exercises.
By incorporating these self-care strategies and being prepared for your treatment sessions, you can navigate your IP chemotherapy journey more effectively.
Conclusion: Advancements and Future Directions in IP Chemotherapy
As we have explored throughout this article, intraperitoneal chemotherapy represents a significant advancement in the treatment of certain cancers, particularly those affecting the peritoneal cavity. By delivering chemotherapy directly to the site of the cancer, IP chemotherapy can achieve higher drug concentrations at tumor sites, potentially improving treatment outcomes.
Ongoing research and advancements in IP chemotherapy techniques are expected to further enhance its effectiveness. We are seeing emerging trends in the development of new chemotherapy agents and improved delivery systems, which are likely to play a crucial role in shaping the future of IP chemotherapy.
The future directions of IP chemotherapy are promising, with potential advancements in hyperthermic intraperitoneal chemotherapy (HIPEC) and the integration of IP and IV chemotherapy protocols. As our understanding of cancer biology and treatment modalities continues to evolve, we can expect IP chemotherapy to remain a vital component of comprehensive cancer care.
FAQ
What is intraperitoneal chemotherapy?
Intraperitoneal chemotherapy, also known as “chemo shots in the stomach,” is a treatment method that involves delivering chemotherapy directly into the peritoneal cavity, where cancer cells are present. This approach allows for higher concentrations of chemotherapy agents to target cancer cells more effectively.
How does intraperitoneal chemotherapy differ from traditional chemotherapy?
Unlike traditional intravenous chemotherapy, which circulates chemotherapy throughout the body, intraperitoneal chemotherapy delivers drugs directly to the peritoneal cavity, where cancer cells are more likely to be present. This targeted approach can lead to improved efficacy and reduced side effects.
What is an intraperitoneal port, and how is it implanted?
An intraperitoneal port is a device implanted under the skin to facilitate the delivery of chemotherapy into the peritoneal cavity. The implantation process involves a minor surgical procedure, where the port is placed under the skin, typically in the abdominal area, and connected to a catheter that delivers chemotherapy to the peritoneal cavity.
What types of cancer can benefit from intraperitoneal chemotherapy?
Intraperitoneal chemotherapy is often used to treat cancers that involve the peritoneum, such as ovarian cancer and stomach cancer. This treatment approach can also be used for other types of gastrointestinal malignancies.
What is “chemo belly,” and how long does it last?
“Chemo belly” refers to abdominal swelling and discomfort that can occur after intraperitoneal chemotherapy. The symptoms are usually temporary and can be managed with proper care. The condition typically resolves within a few weeks after treatment.
What are the side effects of intraperitoneal chemotherapy compared to intravenous chemotherapy?
While both methods share some common side effects, intraperitoneal chemotherapy can cause additional side effects related to the abdominal cavity, such as abdominal pain, swelling, and bowel complications. However, the targeted approach of IP chemotherapy can also reduce systemic side effects.
How are chemotherapy agents selected for intraperitoneal treatment protocols?
Chemotherapy agents used in intraperitoneal treatment protocols, such as paclitaxel and platinum-based drugs, are selected based on the type of cancer, individual patient factors, and the specific treatment goals. The choice of drugs is often tailored to the patient’s needs and medical history.
What is Hyperthermic Intraperitoneal Chemotherapy (HIPEC), and how does it work?
HIPEC is a specialized form of intraperitoneal chemotherapy that involves delivering heated chemotherapy drugs directly into the peritoneal cavity during surgery. The heat enhances the effectiveness of the chemotherapy, allowing for more effective killing of cancer cells.
Can intraperitoneal chemotherapy be combined with intravenous chemotherapy?
Yes, intraperitoneal chemotherapy can be combined with intravenous chemotherapy as part of a dual treatment approach. This combination can be used to target cancer cells both locally and systemically, potentially improving treatment outcomes.
How can patients prepare for their first intraperitoneal chemotherapy session?
Patients can prepare for their first intraperitoneal chemotherapy session by following their doctor’s instructions, which may include dietary changes, medication adjustments, and other preparatory steps. It’s also essential to discuss any concerns or questions with their healthcare team.
What self-care strategies can help manage the side effects of intraperitoneal chemotherapy?
Patients can manage the side effects of intraperitoneal chemotherapy by following a healthy diet, staying hydrated, getting enough rest, and engaging in gentle exercise. They can also work with their healthcare team to develop a personalized self-care plan.