Endometriosis lesions are abnormal growths that develop outside the uterus. They affect about 10% of women of reproductive age worldwide. These growths can cause severe pain and make it hard to get pregnant, greatly affecting a woman’s life quality.
We know that endometriosis lesions are a long-term condition. They can last from the start of a woman’s first period to menopause, without regard to ethnicity or social status. It’s important to understand what these lesions are and why they form. This knowledge helps in early detection and proper treatment.
Key Takeaways
- Endometriosis lesions are abnormal tissue growths occurring outside the uterus.
- These lesions affect approximately 10% of reproductive-age women globally.
- The condition can cause significant pain and fertility issues.
- Early recognition and management are critical for improving quality of life.
- Endometriosis lesions can persist from menarche through menopause.
Understanding Endometriosis and Its Global Impact

Endometriosis is a complex condition that affects millions of women worldwide. It’s important to understand its definition, prevalence, and demographics. This condition has far-reaching consequences for women globally.
What Defines Endometriosis as a Condition
Endometriosis is a chronic and often painful condition. Tissue similar to the lining inside the uterus grows outside the uterus. This causes inflammation, scarring, and adhesions.
This ectopic endometrial tissue leads to symptoms like pelvic pain, heavy menstrual bleeding, and infertility. The exact cause of endometriosis is unknown. But factors like genetic predisposition, hormonal influences, and environmental factors are thought to play a role.
Understanding endometriosis shows it’s a complex condition. It needs a thorough approach to management and treatment.
Prevalence Statistics and Demographics
Endometriosis affects about 10% of reproductive-age women worldwide. This means around 190 million people globally are impacted. The prevalence varies across different populations.
- Endometriosis can occur in women from the onset of their first period (menarche) through menopause.
- The condition affects women of all ethnic backgrounds and socio-economic statuses.
- There is a significant delay in diagnosis, with some women experiencing symptoms for up to 10 years before receiving a definitive diagnosis.
A recent study found the global burden of endometriosis is substantial. It has significant impacts on quality of life, productivity, and healthcare costs. This highlights the need for increased awareness and understanding of endometriosis.
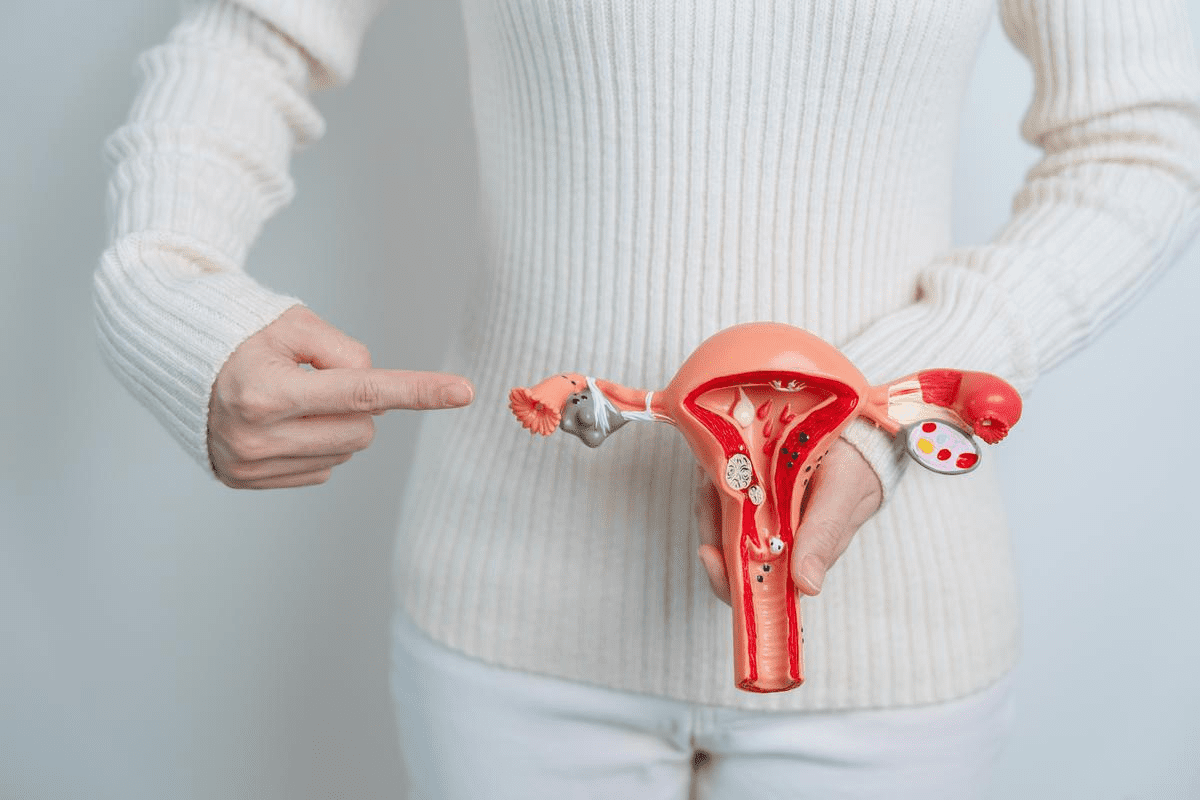
What Are Endometriosis Lesions?

Understanding endometriosis lesions is key to knowing about endometriosis, a common condition in women. These lesions are abnormal growths that look like the uterus lining but are found outside the uterus.
Definition and Basic Characteristics
Endometriosis lesions are abnormal growths that look like the uterus lining but are found outside the uterus. They can cause inflammation, scarring, and adhesions. There are three main types of lesions based on their location and characteristics.
- Superficial peritoneal endometriosis refers to lesions on the peritoneal surface.
- Ovarian endometrioma, also known as “chocolate cysts,” are cysts filled with old blood.
- Deep infiltrating endometriosis involves lesions that penetrate deeply into the tissue.
How Lesions Differ from Normal Endometrial Tissue
Endometriosis lesions look similar to normal endometrial tissue but behave differently. Unlike normal tissue, which sheds and bleeds with hormonal changes, endometriosis lesions cause persistent inflammation and pain. The abnormal environment around these lesions helps them grow and stay, leading to endometriosis symptoms.
Research shows that endometriosis lesions and normal endometrial tissue differ due to genetics, hormones, and environment. Knowing these differences is important for finding effective treatments.
Types of Endometriosis Lesions
There are three main types of endometriosis lesions. Each has its own features. Knowing these differences helps doctors diagnose and treat better.
Superficial Peritoneal Endometriosis
Superficial peritoneal endometriosis is the most common type. It happens when endometrial tissue grows on the peritoneum. This tissue lines the pelvic cavity. Symptoms include pelvic pain and discomfort, often during menstrual periods.
Ovarian Endometriomas
Ovarian endometriomas, or “chocolate cysts,” are filled with old blood. They look dark. These cysts can cause a lot of pain and raise the risk of ovarian cancer. Surgery is often needed to remove them and reduce pain and cancer risk.
Deep Infiltrating Endometriosis
Deep infiltrating endometriosis (DIE) is a severe form. The endometrial tissue goes deep into tissues and organs like the bowel or bladder. This can lead to a lot of pain and problems, like bowel blockage. Treating DIE often needs a team effort, with surgery and medicine.
The main types of endometriosis lesions are:
- Superficial Peritoneal Endometriosis: Affects the peritoneum’s surface.
- Ovarian Endometriomas: Cysts on ovaries filled with old blood.
- Deep Infiltrating Endometriosis: Goes deep into tissues and organs.
Each type of endometriosis lesion has its own challenges. Understanding these helps doctors give better care to patients.
Visual Appearance and Morphology of Lesions
Understanding the look of endometriosis lesions is key for doctors to diagnose and treat it well. These lesions can look different, depending on their shape and color. They can be categorized into several types based on these features.
White Lesions: Early and Subtle Signs
White lesions are often seen early in endometriosis. They can be hard to spot at first glance. These lesions show where endometrial tissue has grown outside the uterus.
Red Lesions: Active and Inflammatory
Red lesions show that endometriosis is active and causing inflammation. They have a lot of blood, which makes them look red. This means the disease is likely causing strong symptoms.
Black “Powder Burn” Lesions: Older Deposits
Black “powder burn” lesions are older and have changed due to the menstrual cycle. They look dark because of hemosiderin, a byproduct of old blood. These lesions are common in long-standing cases of endometriosis.
The table below shows the main features of different endometriosis lesions:
Lesion Type | Appearance | Activity Level |
White Lesions | White or clear | Early or subtle |
Red Lesions | Red or pink | Active and inflammatory |
Black “Powder Burn” Lesions | Black or dark brown | Older deposits |
In summary, the look and shape of endometriosis lesions tell us a lot about the disease. Knowing these differences is essential for making the right diagnosis and treatment plan.
Why Do Endometriosis Lesions Form?
Understanding why endometriosis lesions form is key to finding better treatments. The process is complex, and while we don’t know all the details, several theories exist.
Retrograde Menstruation Theory
The retrograde menstruation theory is a top explanation for endometriosis lesions. It says that during menstruation, some menstrual tissue flows back through the fallopian tubes. This tissue then implants on nearby tissues and organs in the pelvic cavity.
Key aspects of retrograde menstruation include:
- Menstrual flow contains endometrial cells
- Cells implant on pelvic surfaces
- Implanted cells proliferate and form lesions
Alternative Theories of Lesion Development
While the retrograde menstruation theory is strong, it doesn’t cover all cases of endometriosis. Other theories include:
- Lymphatic or Circulatory Spread: Endometrial cells might travel through the lymphatic or circulatory systems to other parts of the body.
- Metaplasia: Cells in the pelvic cavity could change into endometrial-like cells.
- Immune Dysfunction: Problems with the immune system might help endometriosis lesions develop and stay.
Dr. [Researcher’s Name] said in a study, “The exact ways endometriosis lesions form are not fully known. It’s likely that many factors play a role in this condition.”
“The pathogenesis of endometriosis is complex and multifactorial, involving hormonal, genetic, and environmental factors.”
Genetic and Environmental Contributors
Genetic predisposition and environmental factors are thought to influence endometriosis lesions.
Factor | Description | Impact |
Genetic Predisposition | Family history of endometriosis | Increased risk |
Environmental Toxins | Exposure to dioxins and other pollutants | Potential contributor |
Hormonal Influences | Estrogen levels and hormonal balance | Lesion growth and maintenance |
By understanding the factors behind endometriosis lesions, we can improve diagnosis and treatment.
How Endometriosis Lesions Affect the Body
It’s important to know how endometriosis lesions affect the body. This knowledge helps in creating better treatment plans. It also improves how well patients do.
Pain Mechanisms
The pain from endometriosis is complex. Lesions can cause pain in many ways. Inflammation is a big part of it, as it makes prostaglandins and other chemicals that hurt.
Where and how deep the lesions are also matters. For example, lesions on the uterosacral ligaments or deep in tissues can hurt more.
Fertility Impact
Endometriosis can really hurt fertility. Lesions can distort anatomy, cause adhesions, and lead to inflammation. This can mess up ovulation, fertilization, and implantation.
Ovarian endometriomas can also hurt egg quality and number. This makes it harder for women to get pregnant.
Effects on Surrounding Organs
Lesions can also harm nearby organs like the bowels, bladder, or ureter. When they stick to or go into these organs, they can cause problems. This includes bowel blockages, urinary issues, and swelling in the kidneys.
Deep infiltrating endometriosis is very serious. It can hurt important structures a lot.
This shows we need to treat the whole person, not just the lesions. We must care for the patient’s overall health and well-being.
Diagnosis of Endometriosis Lesions
Diagnosing endometriosis lesions requires a mix of clinical checks and advanced tests. We’ll look at how to spot endometriosis, from non-invasive scans to surgery and new methods.
Non-Invasive Imaging Techniques
Non-invasive scans are key in first checking for endometriosis. They find and measure lesions without surgery.
Some common scans include:
- Ultrasound: Good for finding ovarian cysts and checking deep endometriosis.
- Magnetic Resonance Imaging (MRI): Gives clear views of the pelvis, showing where lesions are.
Imaging Technique | Advantages | Limitations |
Ultrasound | Non-invasive, easy to find, and affordable | Not great for small or deep lesions |
MRI | Shows detailed images, good for deep lesions | Costly, not as common as ultrasound |
Surgical Diagnosis Through Laparoscopy
Laparoscopy is the top way to find endometriosis lesions. It lets doctors see the pelvis and take tissue samples.
Laparoscopy’s benefits are:
- Direct Visualization: Finds lesions accurately.
- Histological Confirmation: Confirms endometriosis by examining tissue.
Emerging Diagnostic Approaches
New methods are coming to make diagnosing endometriosis easier and more accurate.
These new ways include:
- Simple Symptom Checklists: Spot people at risk by their symptoms.
- Blood Tests: Looking for biomarkers to diagnose through blood.
- Self-Tests Using Saliva or Menstrual Blood: Non-invasive tests for diagnosing endometriosis.
These new methods are promising, but more research is needed to prove they work well.
Treatment Options for Endometriosis Lesions
There are many ways to treat endometriosis lesions. Doctors use medicine, surgery, and other methods. The main goal is to ease symptoms and improve life quality.
Medical Management Strategies
Medical treatment is often the first step. It includes:
- Hormonal therapies to slow down endometrial tissue growth.
- Pain relief medications to manage symptoms.
These treatments help manage symptoms. They are often used together with other methods.
Surgical Approaches to Lesion Removal
Surgery is considered when medicine doesn’t work or lesions are severe. Surgical options include:
- Laparoscopic surgery to remove or destroy endometrial lesions.
- In some cases, more extensive surgery such as hysterectomy may be considered.
Surgery can bring significant relief to many patients.
Complementary and Integrative Approaches
Complementary therapies also help manage endometriosis. These include:
- Dietary changes and nutritional supplements.
- Acupuncture and other alternative therapies.
These methods can help ease symptoms and improve well-being.
Conclusion
Understanding endometriosis lesions is key to tackling this condition. It affects millions of women globally. We’ve looked into what these lesions are, their types, and how they look. We’ve also talked about how they affect women’s health.
Endometriosis lesions are more than just growths. They show how hormones, genes, and the environment interact. These lesions can cause a lot of pain, make it hard to get pregnant, and affect a woman’s life quality.
We’ve covered different ways to treat endometriosis. This includes medicine, surgery, and other therapies. It’s important to treat each patient differently, based on their needs.
In summary, endometriosis lesions are a big part of understanding and treating endometriosis. By understanding this condition and its effects, we can offer better care and support to those affected.
FAQ
What are endometriosis lesions?
Endometriosis lesions are abnormal growths of endometrial tissue outside the uterus. They cause pain, inflammation, and symptoms in women with endometriosis.
What is the difference between endometrial lesions and endometriosis lesions?
Endometrial lesions grow inside the uterus. Endometriosis lesions grow outside the uterus, often on the pelvic peritoneum, ovaries, or other tissues.
What are the different types of endometriosis lesions?
There are three main types of endometriosis lesions. These include superficial peritoneal endometriosis, ovarian endometriomas, and deep infiltrating endometriosis. Each type has its own characteristics and health impacts.
What are powder burn lesions in endometriosis?
Powder burn lesions, or black lesions, are a type of endometriosis. They look like dark, burnt spots on the pelvic peritoneum. They show older, more established endometrial tissue deposits.
How do endometriosis lesions affect fertility?
Endometriosis lesions can affect fertility. They cause inflammation, scarring, and adhesions in reproductive organs. This can disrupt ovulation, fertilization, or embryo implantation.
What are the mechanisms of pain production in endometriosis lesions?
Endometriosis lesions cause pain through inflammation, nerve irritation, and pain chemicals. This leads to symptoms like pelvic pain, dysmenorrhea, and dyspareunia.
How are endometriosis lesions diagnosed?
Diagnosing endometriosis lesions involves imaging like ultrasound or MRI. Laparoscopy is also used for direct visualization and biopsy of the lesions.
What are the treatment options for endometriosis lesions?
Treatments include medical management, surgical removal, and complementary approaches. These include hormonal therapies, surgery, and pain management.
Can endometriosis lesions be a sign of a more serious underlying condition?
Endometriosis lesions can sometimes indicate a more complex condition. This includes adenomyosis or other gynecological disorders. Thorough diagnosis is key.
Are there any genetic or environmental factors that contribute to the development of endometriosis lesions?
Both genetics and environment play a role in endometriosis lesions. Hormonal influences, menstrual characteristics, and toxin exposure are factors. The exact causes are complex and multifactorial.
References
National Center for Biotechnology Information. Endometriosis Lesions: Formation, Prevalence, and Impact on Women. Retrieved from
https://pubmed.ncbi.nlm.nih.gov/25424120/