Last Updated on October 22, 2025 by mcelik
Did you know that Mesenchymal Stromal Cells can turn into different cell types? They play a crucial role in tissue repair and regeneration. These multipotent stromal cells can keep growing and changing into many types of cells. This makes them very important in fixing damaged tissues.
Mesenchymal stem cells can become bone, cartilage, and fat cells. This shows they could help with many health problems. They might even help with diseases like autoimmune ones.
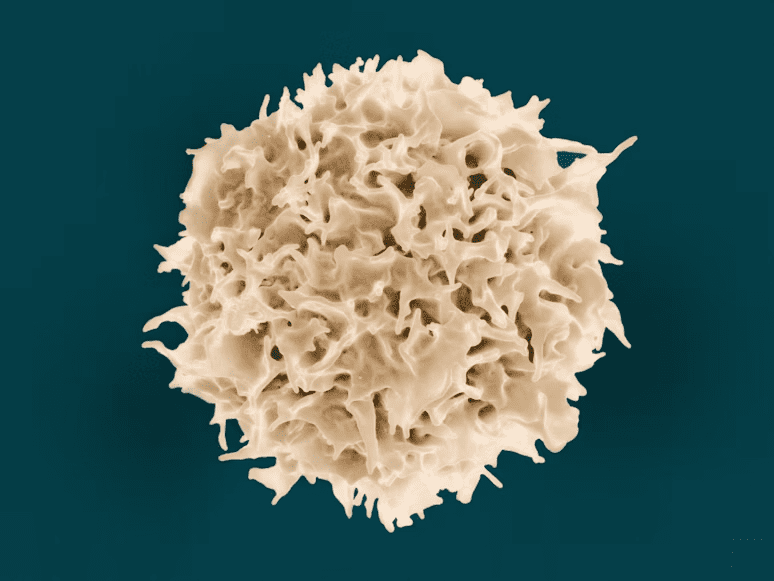
Mesenchymal stromal cells (MSCs) are a type of stem cell. They are important in regenerative medicine. These cells can grow themselves and turn into different cell types.
The term mesenchymal stromal cells describes a group of stem cells. They are known for being able to grow and change into many cell types. The name MSCs has changed over time. Now, “mesenchymal stromal cells” is the preferred term because it better describes their role.
The International Society for Cellular Therapy set rules for MSCs. They must stick to plastic, have certain markers, and grow into different cells. This includes osteoblasts, chondrocytes, and adipocytes.
These rules help scientists know what MSCs are. They make it easier to use MSCs in research and treatments. MSCs can turn into many cell types, which is good for fixing damaged tissues.
The discovery of mesenchymal stem cells (MSCs) was a big step in regenerative medicine. MSCs were first found in bone marrow. Later, research showed they are in many other tissues too.
At first, scientists focused on finding and studying MSCs. They were found in bone marrow and could grow and change into different cell types. This early work showed MSCs could be useful in cell therapy.
MSCs were first found in bone marrow. Researchers like Friedenstein and colleagues found cells in bone marrow that could grow and change into many types of cells.
Our knowledge of MSCs has grown a lot over time. Now we know MSCs are in many places in the body, like fat tissue and umbilical cord. This has opened up more ways to use MSCs in medicine.
Research has also shown MSCs can talk to immune cells and help control inflammation. This is important for treating diseases and helping tissues heal.
As scientists learn more about MSCs, we see more ways they can help people. The evolution of MSC understanding shows how fast regenerative medicine is moving.
MSCs have special abilities that make them key in regenerative medicine. They can self-renew and turn into different cell types. This makes them great for fixing tissues and regrowing them.
MSCs can keep themselves going, a trait called self-renewal. This lets them stay around and help keep tissues healthy for a long time. Their self-renewal is key for their use in medicine, allowing them to grow and help heal.
MSCs can also change into many types of cells. They can become osteoblasts, chondrocytes, adipocytes, and myocytes. This makes them useful for fixing bones, cartilage, and muscles.
How MSCs turn into these cells is complex. It involves many signals and what’s around them. For example, they can turn into bone cells with the right growth factors and conditions. This shows how important it is to understand how MSCs change.
MSCs’ ability to become many cell types is very important. It helps scientists find new ways to treat diseases and injuries. By using MSCs’ powers, they hope to create new treatments for many health problems.
Mesenchymal stem cells (MSCs) come from many places, each with its own benefits and challenges. This variety makes MSCs useful in research and treatments.
Bone marrow is a classic source of MSCs. It’s full of these cells. Bone marrow-derived MSCs can turn into different cell types. This makes them great for fixing damaged tissues.
Fat tissue is another key source of MSCs. Getting MSCs from fat is easier than from bone marrow. Adipose-derived MSCs are good for fixing and growing new tissues.
The umbilical cord is also a good source of MSCs, after birth. Umbilical cord-derived MSCs grow well and are easy to get. This makes them great for treatments.
Dental tissues like pulp and ligament can also give MSCs. Other places include menstrual blood, placenta, and amniotic fluid. These sources offer more ways to use MSCs in medicine.
| Source | Characteristics | Advantages |
| Bone Marrow | Rich in MSCs, ability to differentiate into various cell types | Well-established source, versatile differentiation |
| Adipose Tissue | Less invasive harvesting, abundant MSCs | Easy to obtain, high yield of MSCs |
| Umbilical Cord | High proliferative capacity, easily accessible | Non-invasive source, high therapeutic use |
| Dental Tissues | MSCs found in dental pulp and periodontal ligament | Potential for dental and oral tissue regeneration |
The many sources of MSCs show their big promise in fixing damaged tissues and growing new ones. Knowing about MSCs from different places helps us use them better in medicine.
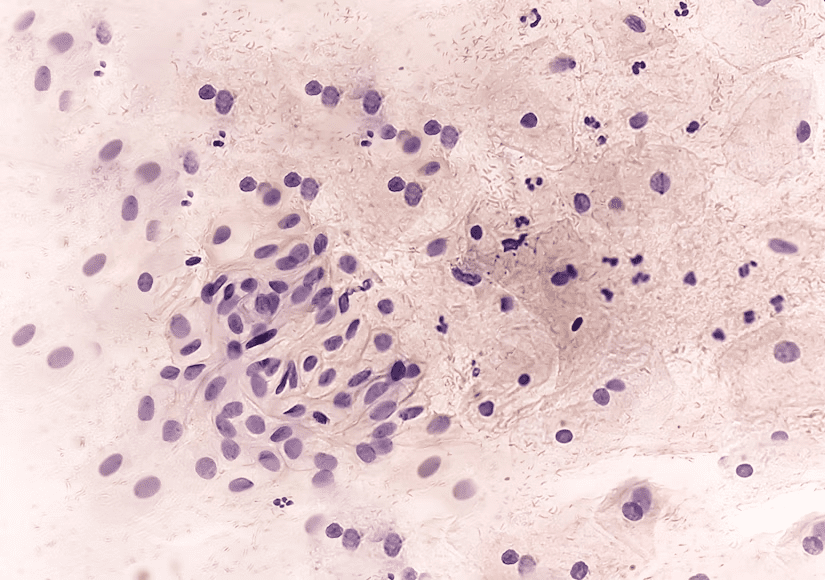
Getting MSCs ready for use in regenerative medicine is key. It involves several important steps. These steps make sure MSCs are of high quality and can be used in different ways.
There are many ways to get MSCs from different sources. Density gradient centrifugation separates MSCs by density. Plastic adherence uses MSCs’ ability to stick to plastic to separate them from other cells.
These methods are essential for getting pure MSCs. Pure MSCs are needed for successful growth and use in treatments.
After getting MSCs, they need the right conditions to grow. The culture medium has growth factors and serum to help them grow.
The main things that affect MSC growth are:
Getting these conditions right is important. It helps MSCs grow enough for use in treatments.
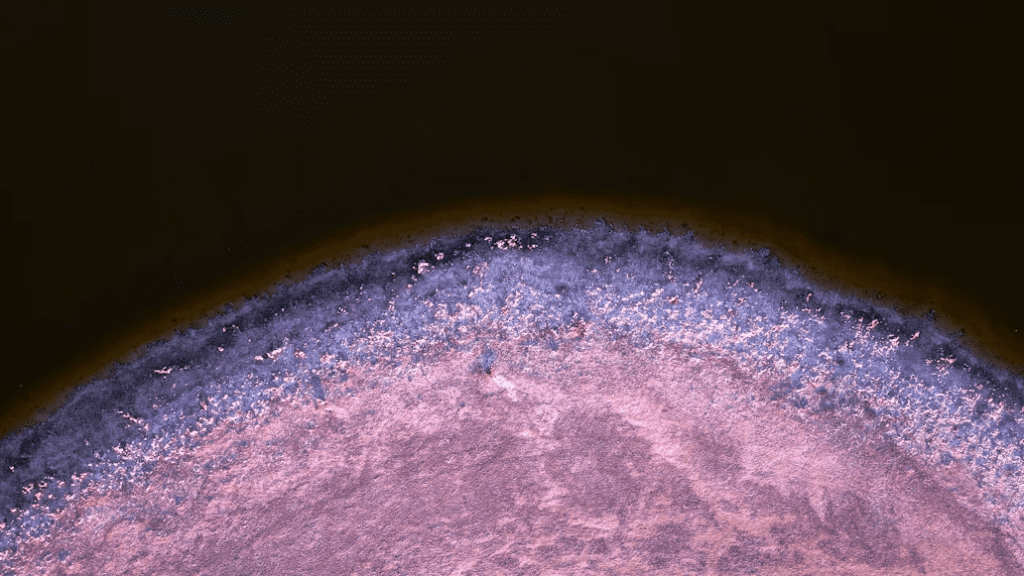
MSCs come from pericytes, which are key in keeping blood vessels stable and helping tissues heal. Pericytes wrap around the blood vessel’s endothelial cells. They are vital for the blood vessel’s health and function.
The perivascular location theory says MSCs come from pericytes near blood vessels. This idea is backed by MSCs being found near blood vessels in many tissues. The area around blood vessels is special for MSCs to thrive.
Pericytes are important because they can turn into different cell types. They also help control the immune system. These skills are key for fixing and growing tissues.
MSCs are found in many places, like bone marrow, fat, umbilical cord, and teeth. They help keep tissues healthy and fix them when needed.
Each tissue has its own MSCs with special abilities. For example, MSCs from bone marrow help blood cells, while those from fat help grow fat tissue.
MSCs being in many tissues shows their flexibility and usefulness in medicine. Knowing where MSCs come from and where they are helps us use their healing powers.
MSCs have a key role in controlling the immune system and reducing inflammation. This makes them a great tool for treating immune-related diseases.
MSCs work with different immune cells like T cells and B cells. They help control the immune response by stopping the growth and activation of these cells. This prevents too much inflammation and damage to tissues.
Key mechanisms of MSC-immune cell interaction include:
A recent study found that “MSCs can suppress T cell proliferation and induce regulatory T cells, which play a critical role in maintaining immune tolerance”
This immunomodulatory effect is key for preventing autoimmune diseases and helping grafts accept in transplants.
MSCs fight inflammation in several ways, including by releasing anti-inflammatory cytokines like IL-10 and TGF-β. These cytokines balance out the pro-inflammatory signals, reducing inflammation and helping tissues heal.
The therapeutic value of MSCs in treating inflammatory and autoimmune diseases is huge. By managing the immune response and lowering inflammation, MSCs offer a hopeful path for treating diseases like rheumatoid arthritis, multiple sclerosis, and inflammatory bowel disease.
Trophic factor secretion and paracrine effects are key ways MSCs help heal and repair tissues. MSCs release many bioactive molecules that aid in healing and tissue growth.
MSCs make a variety of growth factors and cytokines important for fixing tissues. These include VEGF, FGF, and PDGF, among others. These factors help with blood vessel growth, cell growth, and cell change, all vital for healing.
“The MSCs are not just a source of cells for repair, but they are also a source of trophic factors that can modulate the environment to support regeneration.”
MSCs also release EVs and exosomes, which are tiny, membrane-bound particles. These vesicles carry proteins, lipids, and nucleic acids to other cells, helping them heal and repair.
Studies on MSC-derived EVs and exosomes show great promise in treating injuries and diseases.
The trophic factor secretion and paracrine effects of MSCs are key to their healing power. They offer new ways to treat many diseases and injuries.
MSCs have a wide range of uses, from fixing damaged tissues to treating autoimmune diseases and improving heart health. They help in regrowing damaged tissues, controlling the immune system, and fixing heart tissues.
MSCs are key in fixing and growing new tissues. They can turn into different cell types. This makes them great for fixing bones, cartilage, and muscles, helping in orthopedic and musculoskeletal treatments. MSCs help heal and grow tissues by making growth factors and cytokines.
MSCs are also good for treating autoimmune diseases. They can calm down the immune system, reducing inflammation and helping the body accept itself. This makes them a promising treatment for diseases like multiple sclerosis, rheumatoid arthritis, and lupus. MSCs can talk to immune cells and change how they work, which is key in treating autoimmune diseases.
MSCs are being studied for heart disease treatment. They can turn into cells that help make new blood vessels and heart muscle. This supports fixing damaged heart tissue. Using MSCs in heart treatments is an area of ongoing research, looking into their safety and effectiveness.
MSCs have many uses in regenerative medicine, giving hope for treating many diseases and conditions. As research finds more about MSCs, their use in medicine is expected to grow. They will help in fixing tissues, treating autoimmune diseases, and improving heart health.
MSCs are being tested in clinical settings with promising results. They are a key area in regenerative medicine. This is because of their possible benefits in treating various diseases.
Many clinical trials are exploring MSC therapy’s safety and effectiveness. These studies aim to understand MSCs’ role in treating conditions like osteoarthritis and autoimmune disorders.
Ongoing Clinical Trials:
| Condition | Trial Phase | Status |
| Osteoarthritis | II | Recruiting |
| Graft-versus-host disease | III | Active |
| Autoimmune Disorders | I/II | Not yet recruiting |
Recent studies have shown MSCs’ effectiveness in treating diseases. They have shown to reduce inflammation and improve outcomes in autoimmune diseases.
The field is seeing major breakthroughs. Ongoing research will help understand MSC therapy’s benefits and limitations. As more data comes in, MSCs’ therapeutic use will grow.
MSC therapy faces several challenges and limitations. These issues affect its effectiveness and safety. Researchers are working hard to overcome these hurdles for MSC therapy to succeed in medicine.
One big problem is the lack of standardization in MSC therapy. MSCs from different sources and conditions vary in their effects. Standardizing how MSCs are isolated and grown is key to consistent quality. This means setting clear guidelines for culture media, cell numbers, and tests to ensure MSCs are effective and safe.
Safety is a top concern in MSC therapy. MSCs are mostly safe, but there are risks like immune rejection, tumor formation, and unwanted differentiation. It’s important to test MSCs thoroughly before using them in treatments. This helps find ways to avoid any bad effects.
Getting MSCs to the right place and making them stick is hard. The way MSCs are given, how much, and when can affect how well they work. Improving how MSCs are delivered, like using special systems or preparing MSCs better, is being studied. It’s vital for MSCs to reach and work well in the target area.
In summary, MSC therapy is promising but needs to tackle standardization, safety, and delivery issues. Research is ongoing to solve these problems. The goal is to make MSC-based treatments available and effective for patients.
The field of MSC research is growing fast, but it faces ethical challenges. As MSCs are used more in treatments, we must think about the ethics involved.
Rules for MSC research differ around the world. In the U.S., the FDA is key in checking MSC use in trials and treatments.
Important parts of these rules include:
MSC research raises many ethical questions. These include where MSCs come from, how they can change, and possible risks. Key issues include:
Dealing with these ethical issues is key for MSC research to move forward. A strong set of rules and ongoing talks about ethics help ensure MSC treatments are safe and work.
Key Takeaways:
Mesenchymal stem cells (MSCs) are becoming key in regenerative medicine and cell therapy. They can grow and change into different cell types. This makes them useful for many treatments.
MSCs are showing great promise in fixing damaged tissues and treating autoimmune diseases. They also help with heart problems. But, there are challenges like making sure treatments work the same way and keeping them safe.
As scientists learn more about MSCs, their role in medicine will grow. More work is needed to fully use MSCs for new treatments. The future of MSC-based therapies is bright, with new studies and trials underway.
MSCs are special cells that can grow and change into different types of cells. They can become bone, cartilage, fat, and muscle cells. These cells also help control the immune system and can be found in bone marrow, fat, and umbilical cord.
To be called MSCs, these cells must stick to plastic, show certain markers on their surface, and grow into bone, cartilage, and fat cells.
MSCs come from places like bone marrow, fat, umbilical cord, and teeth. Each source has its own benefits and challenges.
MSCs are found using methods like density gradient centrifugation and magnetic-activated cell sorting. They are then grown in special conditions to help them multiply and stay healthy.
MSCs can talk to immune cells and change how the immune system works. They can slow down T cell growth and have anti-inflammatory effects.
MSCs could be used to fix damaged tissues, treat autoimmune diseases, and help with heart problems.
Using MSCs for treatment faces challenges like standardizing procedures, ensuring safety, and figuring out how to get them to work properly in the body.
Research on MSCs is ongoing, with many clinical trials looking at their safety and effectiveness in treating different diseases.
MSC research raises ethical questions, like how to regulate it and what are the moral implications. It’s important to address these to ensure MSCs are used safely and responsibly.
MSCs release important factors that help fix damaged tissues. They also send out tiny particles called exosomes that can help the immune system and aid in healing.
Subscribe to our e-newsletter to stay informed about the latest innovations in the world of health and exclusive offers!