Last Updated on November 27, 2025 by Bilal Hasdemir
Cancer treatment is more than just fighting cancer cells. Managing side effects is key to better patient outcomes and life quality.
About 70% of cancer patients on chemotherapy face side effects. These can range from mild to severe. Premedication is vital in reducing these effects, helping patients stay on their treatment path.
So, what are pre meds for oncology? Premedication, or premeds, are drugs given before cancer treatment to lessen side effects. This article will dive into the types of premedication, how they’re given, and their benefits in cancer care.
Key Takeaways
- Premedication is essential in oncology to manage treatment side effects.
- Premeds can significantly improve patient outcomes and quality of life.
- Different types of premedication are used based on the cancer treatment regimen.
- Effective premedication strategies can reduce treatment interruptions.
- Understanding premeds is vital for both patients and healthcare providers.
Understanding Premedication in Oncology

Premedication is a key part of cancer treatment. It helps reduce side effects from treatments.
Definition and Purpose of Premedications
Premedication means taking medicine before cancer treatment. It helps prevent or lessen side effects. This way, patients can handle their treatment better.
Using premedication is common in oncology. It makes treatment easier for patients. It lowers anxiety, stops allergic reactions, and manages side effects.
The Role of Premedications in Cancer Treatment
Premedications have many roles in cancer treatment. They help make care effective and keep patients comfortable and safe. They reduce side effects, making treatments work better.
Using premedication wisely can greatly help cancer treatment. It lets treatments go on as planned. This improves treatment results.
The Importance of Premedication in Cancer Care
In oncology, premedication is a key factor in reducing side effects from treatments. It helps improve patient outcomes by lessening bad reactions to cancer treatments.
Reducing Treatment Side Effects
Premedication is vital in reducing side effects from cancer treatments, like chemotherapy. It helps doctors lessen the severity of these effects. This makes the treatment experience better for patients.
Common side effects mitigated by premedication include:
- Nausea and vomiting
- Allergic reactions
- Infusion reactions
Improving Treatment Efficacy
Premedication does more than just reduce side effects. It also makes cancer treatments more effective. This prepares the body for treatment, leading to better results for patients.
“The use of premedication has been shown to significantly enhance the tolerability of cancer treatments, allowing patients to complete their treatment regimens as planned.”
Enhancing Patient Comfort and Compliance
Patient comfort and sticking to the treatment plan are key to successful cancer care. Premedication helps reduce anxiety and manage symptoms. This makes patients more comfortable and more likely to follow their treatment plans.
By improving patient comfort, premedication can lead to:
- Increased treatment adherence
- Better overall patient outcomes
- Enhanced quality of life during treatment
Common Types of Premedication Used in Oncology
Premedication in oncology is now a key part of care. It makes patients more comfortable and helps treatments work better. This improves the quality of care for everyone.
Antiemetics for Nausea and Vomiting
Antiemetics are vital for stopping nausea and vomiting from cancer treatments. They help patients feel better and stick to their treatment plans. These include 5-HT3, NK1, and dopamine blockers.
“The use of antiemetics has changed how we handle nausea and vomiting from chemotherapy,” says oncology guidelines.
Corticosteroids for Inflammation
Corticosteroids are key for reducing swelling and inflammation. They help with brain tumors and prevent allergic reactions to some chemotherapy. They also make other treatments more effective.
Antihistamines for Allergic Reactions
Antihistamines prevent allergic reactions to some chemotherapy drugs. They block histamine receptors, making treatments safer for patients.
Anxiolytics for Anxiety Management
Anxiolytics help manage anxiety and stress from cancer. These medications help patients deal with the emotional side of their illness. This improves their well-being and treatment success.
Knowing about different premedications helps doctors tailor care for each patient. This makes treatments more effective and easier to handle.
Antiemetic Premedications for Chemotherapy
Antiemetic premedications are key in stopping nausea and vomiting from chemotherapy. These side effects are very hard for cancer patients. Good antiemetic care helps patients feel better and stick to their treatment.
5-HT3 Receptor Antagonists
5-HT3 receptor antagonists have greatly helped manage nausea and vomiting. They block serotonin, a key player in nausea and vomiting, in the brain and stomach. Ondansetron and granisetron are examples.
NK1 Receptor Antagonists
NK1 receptor antagonists are also important in fighting nausea and vomiting. They stop substance P, a neuropeptide that triggers vomiting. Aprepitant is a well-known NK1 receptor antagonist.
Dopamine Antagonists
Dopamine antagonists, like metoclopramide, have been used for a long time. They block dopamine receptors in the brain, helping to stop vomiting.
Combination Antiemetic Approaches
Using different types of antiemetics together is now common. This approach is recommended for patients getting very strong chemotherapy. It includes a 5-HT3 receptor antagonist, an NK1 receptor antagonist, and a corticosteroid like dexamethasone.
Corticosteroids as Premedication in Oncology
Corticosteroids are now a key part of cancer treatment to lessen inflammation and side effects. These powerful anti-inflammatory drugs make cancer treatments easier to handle.
Mechanisms of Action
Corticosteroids work in several ways, mainly by calming the immune system and reducing swelling. They attach to specific receptors, changing how genes work. This leads to less inflammation and a weaker immune response.
They also stop pro-inflammatory cytokines and start anti-inflammatory proteins. This helps lessen the swelling caused by cancer treatments.
Common Corticosteroids Used
Many corticosteroids are used in cancer treatment, like dexamethasone, prednisone, and methylprednisolone. The right one depends on the cancer, treatment type, and patient health.
| Corticosteroid | Potency | Common Use in Oncology |
| Dexamethasone | High | Antiemetic prophylaxis, managing infusion reactions |
| Prednisone | Moderate | Treating inflammation, part of chemotherapy regimens |
| Methylprednisolone | High | Managing acute inflammation, spinal cord compression |
Dosing Strategies
The dose of corticosteroids varies based on the treatment and patient needs. They are given in amounts that work well but cause fewer side effects.
Dexamethasone is often given 8-20 mg intravenously before chemotherapy to prevent nausea and vomiting. The exact dose and timing depend on the chemotherapy’s strength.
“The right use of corticosteroids as premedication can make cancer treatments easier and improve patient results.” –
Oncology Expert
Knowing how corticosteroids work, which ones are used, and how to dose them helps doctors improve patient care. This makes cancer treatment better for everyone.
Premedication Protocols for Different Chemotherapy Regimens
Premedication plans change a lot based on how likely chemotherapy is to cause nausea and vomiting. Doctors sort chemotherapy into groups based on how much it might upset a patient’s stomach. Then, they pick the right premedication plan for each group.
High Emetogenic Chemotherapy
For chemotherapy that’s very likely to cause stomach problems, doctors use strong premedication plans. These plans mix different medicines to help prevent nausea and vomiting.
| Chemotherapy Regimen | Premedication Protocol |
| Cisplatin-based chemotherapy | 5-HT3 receptor antagonist + NK1 receptor antagonist + corticosteroid |
| Cyclophosphamide + Anthracycline | 5-HT3 receptor antagonist + corticosteroid |
Moderate Emetogenic Chemotherapy
Chemotherapy that’s likely to cause some stomach upset gets a less intense premedication plan. But it’s just as important for keeping nausea and vomiting away.
- Carboplatin-based chemotherapy: 5-HT3 receptor antagonist + corticosteroid
- Oxaliplatin-based chemotherapy: 5-HT3 receptor antagonist + corticosteroid
Low Emetogenic Chemotherapy
Chemotherapy that’s unlikely to upset the stomach might not need a premedication plan. But doctors keep an eye out for any signs of nausea or vomiting.
Breakthrough Symptom Management
Even with premedication, some patients might get nausea or vomiting. Doctors then use more medicines or other treatments to help manage these symptoms.
Good premedication plans are key to helping patients feel better during chemotherapy. By knowing how different treatments might affect the stomach, doctors can make plans that help patients feel their best.
Premedication for Immunotherapy and Targeted Therapies
Immunotherapy and targeted therapies often need premedication to handle infusion reactions and other side effects. These treatments are very effective against cancer but can cause immune responses. These responses need to be managed to keep patients safe and comfortable.
Managing Infusion Reactions
Infusion reactions are common with immunotherapy and targeted therapies. Premedication with antihistamines, corticosteroids, or acetaminophen can greatly reduce these risks and their severity. For example, drugs like rituximab, used in treating some cancers, can cause infusion reactions. So, premedication is a common practice.
Preventing Cytokine Release Syndrome
Cytokine release syndrome (CRS) is a serious condition linked to some immunotherapies, like CAR-T cell therapy. Premedication, including corticosteroids and anti-IL-6 receptor antibodies like tocilizumab, helps prevent or lessen CRS. It’s important to quickly spot and manage CRS to avoid severe problems.
Specific Premedication Requirements
Each immunotherapy and targeted therapy has its own premedication needs. For instance, checkpoint inhibitors like pembrolizumab may need premedication to manage side effects. Healthcare providers must understand these needs to create effective premedication plans.
In summary, premedication is key for safely using immunotherapy and targeted therapies. By knowing the specific needs of each treatment and patient, healthcare providers can reduce risks and improve outcomes.
Administration Methods and Timing of Premedication
Understanding how premedication is given and when is key for better cancer care. The success of premedication in fighting cancer depends on how it’s given and when. This timing is very important.
Oral Administration
Oral premedication is popular because it’s easy and doesn’t hurt. Patients can take these medicines at home, which helps them stick to their treatment plan. But, how well the body absorbs these medicines can affect their success.
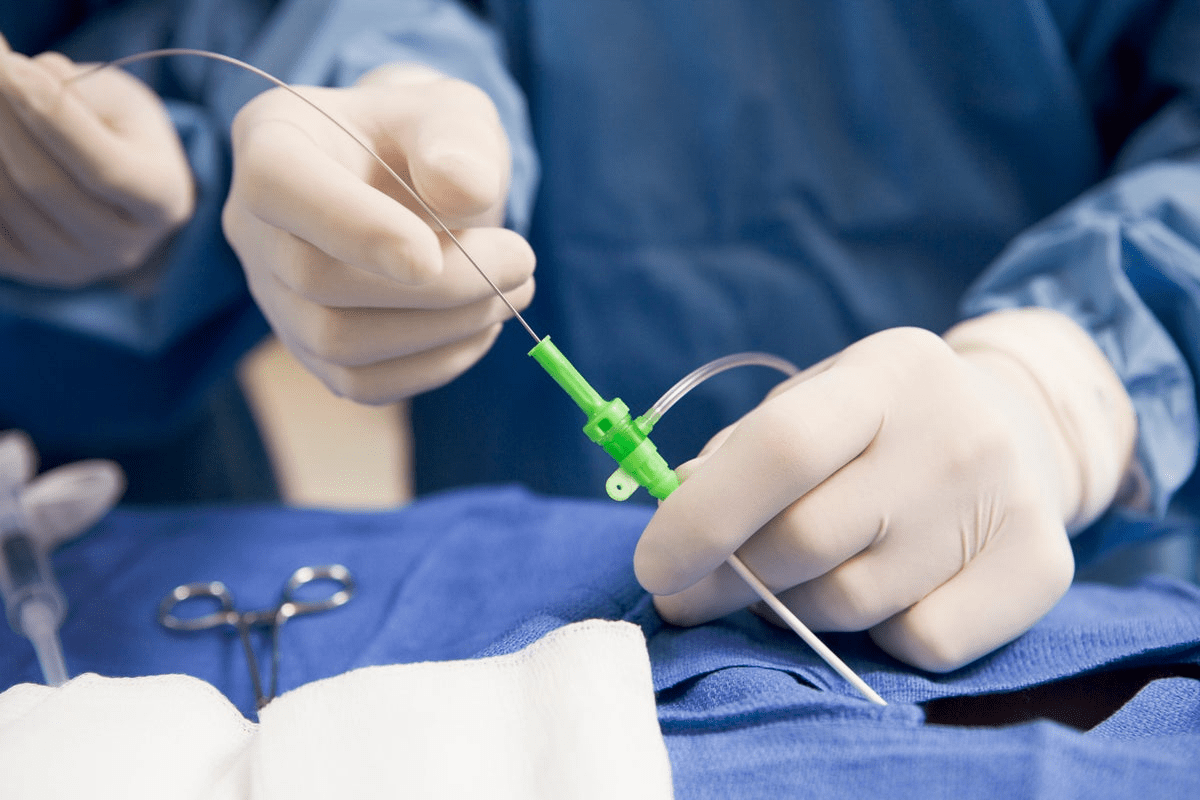
Intravenous Delivery
Intravenous (IV) premedication is used in hospitals for quick action. IV delivery lets doctors control the dose and speed of action. This is important for handling sudden side effects from cancer treatments.
Optimal Timing Before Procedures
When to give premedication is very important. Premedications are given at certain times before treatment starts. This makes sure the medicine is working when the treatment begins. The best time varies with the type of premedication and treatment plan.
Extended Premedication Schedules
Sometimes, premedication is needed for longer periods. Extended premedication helps manage long-lasting side effects or prevent late reactions. How long and how often depends on the treatment and how the patient responds.
Choosing the right way to give premedication and when is key. Healthcare providers can make treatments more effective and make patients more comfortable and likely to follow their treatment plans.
Premedication for Radiation Therapy
Premedication is key in reducing side effects from radiation therapy. This treatment can cause serious side effects that affect a patient’s quality of life. Using premedication can help lessen these effects, making treatment more comfortable and increasing patient compliance.
Managing Radiation-Induced Nausea
Nausea is a common side effect, often seen when the abdomen or brain is treated. Antiemetics can greatly reduce nausea and its severity. 5-HT3 receptor antagonists are often used because they work well against nausea from radiation therapy.
A study in the Journal of Clinical Oncology showed ondansetron’s effectiveness. It found that patients taking ondansetron had much less nausea than those who didn’t.
“The use of antiemetics as premedication before radiation therapy can substantially improve patient outcomes by reducing the incidence of nausea and vomiting.”
Reducing Inflammation and Tissue Reactions
Corticosteroids are used to lessen inflammation and tissue reactions from radiation therapy. These drugs help reduce side effects like skin reactions and mucositis.
| Corticosteroid | Dose | Timing |
| Dexamethasone | 4-8 mg | Before radiation therapy |
| Prednisone | 20-40 mg | Daily during radiation therapy |
Pain Management Approaches
Pain management is vital for patients getting radiation therapy. Using analgesics before treatment can help manage pain. NSAIDs and opioids are often used for this.
Effective premedication strategies, including analgesics and other supportive drugs, can improve patient comfort and treatment outcomes. A personalized approach to pain management is essential, considering each patient’s needs and medical history.
Special Considerations for Pediatric Oncology Premedication
Pediatric oncology premedication needs a special touch for kids with cancer. It’s all about how kids react differently and need the right amount of medicine.
Age-Appropriate Dosing
Getting the right dose of medicine is key for kids. Their bodies handle drugs in ways that differ from adults. Doctors must carefully figure out the dose based on age, weight, and body size.
This careful planning helps make sure the medicine works well. It also helps avoid bad side effects.
For example, antiemetic medications to stop nausea and vomiting need to be given just right for kids. The dose might change based on the child’s age and the type of chemotherapy.
Child-Specific Side Effect Management
Handling side effects in kids with cancer is unique. Kids can react differently to medicines than adults do.
- It’s important to watch for side effects like allergic reactions, mood changes, or unexpected physical responses.
- Doctors must be ready to change how they use premedication based on how the child reacts.
Psychological Support Approaches
Psychological support is a big part of caring for kids with cancer. Using premedication can be helped by ways to reduce anxiety and make treatment better for the child.
Things like play therapy, relaxation exercises, and getting parents involved can really help. They make the child feel more comfortable and willing to cooperate.
By using a full approach that includes the right dose, managing side effects, and psychological support, doctors can make premedication work better for kids. This can lead to better treatment results and a better life for young patients.
Managing Side Effects of Premedication
Premedication is key to reducing treatment side effects but can cause new issues. As cancer treatments grow more complex, it’s vital to manage these side effects well. This is key for patient care.
Common Side Effects
Premedication can lead to various side effects, from mild to severe. Common ones include fatigue, nausea, and allergic reactions. For example, corticosteroids can cause insomnia, mood changes, and increased appetite. Healthcare providers must watch these closely.
Risk-Benefit Assessment
It’s important to do a detailed risk-benefit assessment for premedication. This means looking at the good it does versus its possible side effects. For instance, the benefits of antiemetics to prevent nausea must be weighed against constipation or headache side effects.
Mitigation Strategies
There are ways to lessen premedication side effects. Dose adjustment is one, where the dose is changed to reduce side effects without losing effectiveness. Another is combining premedications with different side effects to improve tolerance. Also, patient education is key in managing expectations and improving adherence.
Evidence-Based Premedication Guidelines
Oncology professionals use evidence-based guidelines for premedication. These guidelines are made from thorough reviews of clinical data. They ensure premedication strategies are safe and effective for cancer treatment.
ASCO Guidelines
The American Society of Clinical Oncology (ASCO) sets guidelines widely used in oncology. These cover managing nausea and vomiting, infusion reactions, and other side effects from treatment.
NCCN Recommendations
The National Cancer Network (NCCN) also gives premedication advice. NCCN guidelines are detailed and based on evidence. They help doctors decide on premedication for various cancer treatments.
International Consensus Approaches
International guidelines are made by experts worldwide. They develop premedication strategies for different healthcare settings. These guidelines help manage complex cases and show new trends in premedication.
Implementation in Clinical Practice
Putting these guidelines into practice involves several steps. This includes educating staff, creating protocols, and watching patient outcomes. Doing this well can improve patient care and reduce complications.
The following table summarizes key aspects of the guidelines from ASCO and NCCN:
| Guideline | Focus Area | Key Recommendations |
| ASCO | Chemotherapy-induced nausea and vomiting | Use of 5-HT3 receptor antagonists, NK1 receptor antagonists, and corticosteroids |
| NCCN | Infusion reactions and hypersensitivity | Premedication with antihistamines and corticosteroids; monitoring for infusion reactions |
| International Consensus | Emerging trends and complex cases | Personalized premedication approaches based on patient risk factors and treatment regimens |
Future Directions in Oncology Premedication
New trends and research are changing premedication in cancer care. Our knowledge of cancer grows, so does our ability to make better premedication plans.
Emerging Medications
New drugs are being made to tackle challenges in premedication. For example, novel antiemetics are coming with better safety and effectiveness. These include new 5-HT3 and NK1 receptor blockers that help more with nausea and vomiting from chemo.
Also, targeted therapies are being worked on to lessen side effects of cancer treatments. These new drugs aim to be more precise, cutting down on bad reactions and improving results for patients.
Personalized Premedication Approaches
The future of premedication is in personalized medicine. Using genetic info and patient details, doctors can make premedication plans just for each person. This makes premedications work better and have fewer side effects.
Personalized premedication means looking at a patient’s genes, medical history, and current health. This tailored approach will grow as genetic testing and data analysis get better.
| Premedication Approach | Benefits | Future Directions |
| Personalized Premedication | Tailored to individual patient needs, improving efficacy and reducing side effects | Integration of genetic testing and advanced data analysis |
| Emerging Medications | Novel antiemetics and targeted therapies with improved safety and efficacy | Continued research and development of new drug classes |
| Research Developments | Advancements in understanding cancer biology and treatment side effects | Translating research findings into clinical practice guidelines |
Research Developments
Research is key to improving premedication in oncology. Studies are looking into how premedications work, finding the best doses, and finding new ways to help.
One big area of study is how premedications and cancer treatments work together. By learning more about these interactions, we can make premedication safer and more effective.
The future of premedication in oncology looks promising. With ongoing research and new trends, we’ll see big improvements in patient care. As we learn more about cancer and its treatments, we’ll be able to offer better premedication plans that help patients more.
Conclusion
Premedication is key in oncology, making care better and outcomes better for patients. Knowing about different premedications and how to give them helps doctors manage side effects. This makes treatments work better.
Good premedication plans are important in fighting cancer. They help avoid bad reactions and make patients more comfortable. Antiemetics, corticosteroids, and antihistamines are often used. Guidelines from groups like ASCO and NCCN help doctors know when and how to use them.
The importance of premedication will only grow as cancer treatments get better. Keeping up with new premedication info and following guidelines is vital. This way, doctors can give the best care to those fighting cancer.
FAQ
What is premedication in oncology?
Premedication in oncology means giving medicines before cancer treatment. This includes chemotherapy, immunotherapy, or radiation therapy. It helps prevent or lessen side effects and makes patients more comfortable.
Why is premedication important in cancer care?
Premedication is key in cancer care. It reduces side effects, makes treatments work better, and improves patient comfort. This leads to better treatment results.
What are the common types of premedication used in oncology?
In oncology, common premedications include antiemetics for nausea and vomiting. Corticosteroids for inflammation, antihistamines for allergic reactions, and anxiolytics for anxiety are also used.
How are antiemetic premedications used in chemotherapy?
Antiemetic premedications prevent nausea and vomiting in chemotherapy. They include 5-HT3 receptor antagonists, NK1 receptor antagonists, dopamine antagonists, and combination approaches.
What is the role of corticosteroids as premedication in oncology?
Corticosteroids are used to reduce inflammation and manage side effects in oncology. They work by suppressing the immune system and reducing inflammation.
How are premedication protocols determined for different chemotherapy regimens?
Premedication protocols are based on the chemotherapy agents’ emetogenic (nausea-causing) levels. High, moderate, and low levels need different premedication strategies.
What are the specific premedication requirements for immunotherapy and targeted therapies?
Immunotherapy and targeted therapies need specific premedications. These include managing infusion reactions and preventing cytokine release syndrome. They also help mitigate side effects.
How are premedications administered, and what is the optimal timing?
Premedications can be given orally or intravenously. The best time varies by premedication type and treatment. Some are given before treatment, while others are given on a longer schedule.
What are the special considerations for premedication in pediatric oncology?
In pediatric oncology, special considerations include age-appropriate dosing and managing side effects in children. Psychological support is also important to minimize treatment impact.
What are the common side effects of premedication, and how are they managed?
Common side effects include various adverse reactions. They are managed through risk-benefit assessment and mitigation strategies. This may involve adjusting the premedication regimen or adding additional medications.
What are the evidence-based premedication guidelines, and how are they implemented in clinical practice?
Guidelines from ASCO and NCCN provide recommendations for premedication strategies. They are implemented through education, policy development, and quality improvement initiatives in clinical practice.
What are the future directions in oncology premedication?
Future directions include emerging medications and personalized premedication approaches. Ongoing research aims to improve premedication strategies and patient outcomes.