Last Updated on December 1, 2025 by Bilal Hasdemir

Every year, over 2,000 Americans try stem cell therapy to ease chronic pain and degenerative conditions.
what are stem cell injections? Regenerative medicine has changed how we heal, opening new doors for treating injuries and diseases. Stem cell injections use the body’s cells to fix damaged tissues.
But, not everyone can get stem cell treatment. Some health issues, age, and other factors can make you not eligible. Knowing the basics of stem cell therapy helps figure out if it’s right for you.
Key Takeaways
- Stem cell therapy involves using the body’s cells to repair damaged tissues.
- Regenerative medicine offers new possibilities for treating chronic conditions.
- Not everyone is a suitable candidate for stem cell treatment.
- Age, health conditions, and other factors affect eligibility for stem cell therapy.
- Understanding the basics of stem cell therapy is key to knowing if it’s right for you.
Understanding Stem Cell Therapy Basics
Stem cell therapy utilizes the body’s natural regenerative cells to repair damaged tissues. These cells can turn into many types of cells. This makes them very useful for medical treatments.
Definition and Types of Stem Cells
Stem cells can grow and change into different cell types. There are a few kinds of stem cells:
- Embryonic Stem Cells: These come from embryos and can become any cell type.
- Adult Stem Cells: Found in adults, these cells can repair but are more limited.
- Induced Pluripotent Stem Cells (iPSCs): Made from adult cells, they act like embryonic cells.
Each stem cell type has its own benefits and is studied for different treatments.
How Stem Cell Therapy Works
Stem cell therapy uses stem cells to fix damaged cells and tissues. The steps are:
- Harvesting: Stem cells are taken from the patient or a donor.
- Processing: The cells are cleaned and ready for use.
- Transplantation: The cells are put into the patient’s body to repair tissues.
A leading researcher says, “Stem cell therapy is promising for treating many diseases. It could be a cure where there were only treatments before.” This shows how stem cell therapy could change medicine.
Knowing about stem cell therapy helps patients understand their treatment choices.
What Are Stem Cell Injections And Their Applications
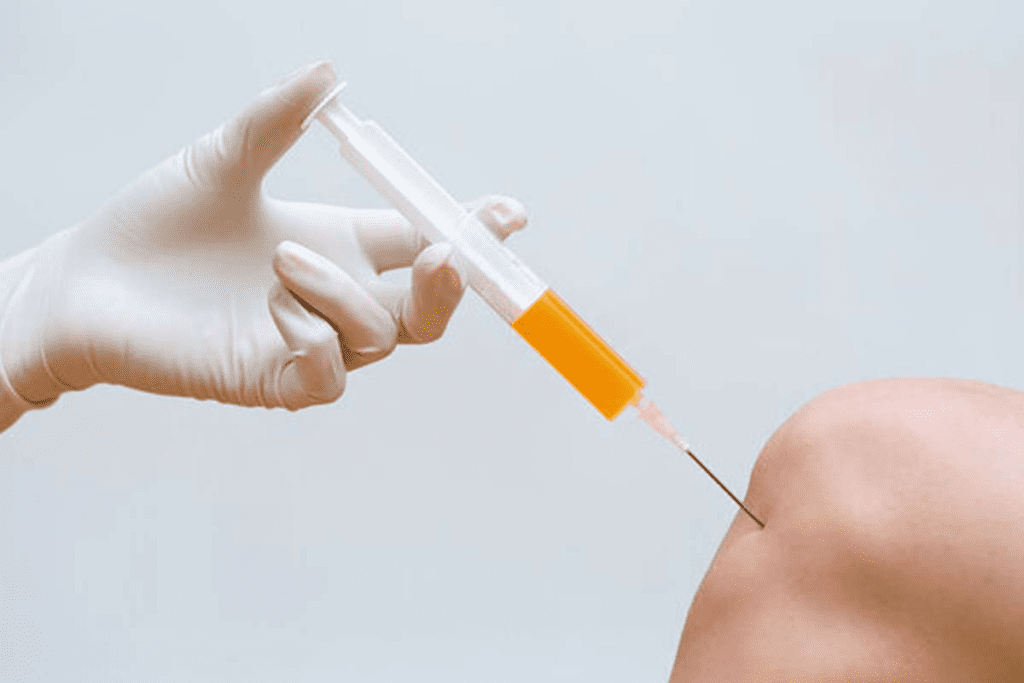
Stem cell injections are a therapy that’s getting a lot of attention. They might help treat many health issues, like joint pain and tissue damage.
Common Medical Uses For Stem Cell Injections
Stem cell injections are used in several ways in medicine. They include:
- Treatment of joint pain and osteoarthritis
- Repair of damaged tendons and ligaments
- Regeneration of tissue in orthopedic and sports injuries
- Potential treatment for certain autoimmune diseases
Stem cell therapy for joint pain is showing great promise. It helps patients with chronic pain and limited mobility due to joint diseases.
The procedure may be performed under local anesthesia or with imaging guidance to ensure accurate placement of the cells.
The stem cell injection procedure starts with getting stem cells from the patient. This is usually from bone marrow or fat tissue. Then, these cells are processed and injected into the needed area.
The procedure may be performed under local anesthesia or with imaging guidance to ensure accurate placement of the cells. Patients often recover quickly, feeling better soon after.
It’s key for patients to talk to a healthcare professional about stem cell treatment options. This helps figure out if it’s right for their condition and what benefits and risks there are.
The Screening Process For Stem Cell Therapy Candidates
To ensure safety and success, stem cell therapy candidates go through a detailed screening. This careful check is key to see if they’re right for stem cell therapy.
Medical History Evaluation
The first step is a medical history evaluation. This looks at the patient’s past health, treatments, and current health issues. It helps find any risks or things that might not work well with the therapy.
The evaluation checks the patient’s overall health, chronic diseases, and past surgeries. It’s important for the doctor to know the patient’s health history. This helps tailor the treatment just right.
Physical Examination And Testing Requirements
A comprehensive physical examination is done to check the patient’s current health. This, along with specific testing requirements, helps find any conditions that might affect the therapy’s success.
Tests might include blood work, X-rays, or MRI scans. These tests give important info about the patient’s health. They help decide the best treatment plan.
By looking at the medical history and test results, doctors can decide if a patient is a good fit for stem cell therapy. This careful process is vital. It helps make sure the treatment works well and is safe.
General Contraindications For Stem Cell Therapy
Stem cell therapy has its limits. These limits are divided into absolute and relative contraindications. Knowing these limits helps find the right candidates for therapy and lowers risks.
Absolute Contraindications
Absolute contraindications mean you can’t have stem cell therapy. This is because of big risks. For example, people with active malignancies or those fighting cancer should not get it. It could make tumors grow or mess up cancer treatment.
Other big no-nos include severe immunosuppression. This means your immune system is too weak. It makes you more likely to get sick and could make therapy harder.
Relative Contraindications
Relative contraindications are not as clear-cut. They might make therapy a bad idea but don’t always mean no. These include chronic infections, autoimmune diseases, and some heart problems. Each case needs careful thought.
For chronic infections like HIV or hepatitis, the choice depends on how bad the infection is. People with autoimmune diseases need extra attention. Their condition might change how therapy works.
Having contraindications doesn’t mean you can’t get therapy. But, it means doctors need to think hard about it. Knowing about these limits helps patients and doctors make smart choices about therapy.
Patients With Active Cancer Or History of Malignancy
Stem cell therapy is promising for many health issues. But, it’s not right for those with active cancer or a history of cancer. The worry is that it might help cancer cells grow or mess with how the body fights cancer.
Why Cancer Patients May Be Excluded
Cancer patients usually can’t get stem cell therapy because of the risks. Stem cells can turn into different cell types. But, in cancer, they might help tumors grow or come back.
Specific Cancer Types of Concern
Some cancers are riskier with stem cell therapy. For example, cancers that can come back easily or grow fast are a big worry. Breast cancer, leukemia, and lymphoma are cancers where we’re extra careful.
- Breast cancer
- Leukemia
- Lymphoma
Waiting Periods After Cancer Remission
Patients in remission often wait before getting stem cell therapy. The wait time depends on the cancer type, how advanced it was, and the treatments used. We want to make sure the cancer is fully gone before starting therapy.
Studies suggest a 2-5 year wait after remission is common. But, it can change based on each person’s situation.
Blood Disorders and Hematological Conditions
Blood disorders and hematological conditions can affect how safe and effective stem cell therapy is. These issues can make it hard for the blood to work right, which can complicate the therapy.
Bleeding Disorders and Coagulation Issues
People with bleeding disorders or coagulation issues face higher risks with stem cell therapy. Bleeding disorders, like hemophilia, make it hard for blood to clot. This can lead to problems during and after the treatment. Coagulation issues, such as thrombocytopenia, can also cause bleeding or clotting problems.
It’s important to manage and watch these conditions closely. Pre-treatment assessments help find any bleeding or coagulation risks. This might mean changing the treatment plan or giving medicines to lower these risks.
Blood Cancers and Stem Cell Therapy Risks
Blood cancers, like leukemia and lymphoma, pose special challenges for stem cell therapy. The main worry is that the therapy might not work or could even be harmful for patients with active or recent blood cancers.
The risks include cancer coming back or introducing cancer cells into the treatment. So, patients with blood cancer history usually have to wait before getting stem cell therapy.
It’s key for both patients and doctors to understand how blood disorders and conditions affect stem cell therapy. By carefully looking at these conditions and managing risks, we can make stem cell treatments safer and more effective.
Autoimmune Disease Patients and Contraindications
Autoimmune diseases are a big challenge for stem cell therapy. They need careful thought about possible contraindications. These conditions make the immune system attack the body’s own cells, which can change how well stem cell treatment works.
How Autoimmune Conditions Affect Stem Cell Therapy Outcomes
Autoimmune diseases can change stem cell therapy results in a few ways. First, the immune system’s problems might stop stem cells from working well. Second, the ongoing inflammation can make the stem cell environment less effective.
The immune system’s reaction to stem cell therapy is hard to predict in patients with autoimmune diseases. Sometimes, it can help, but other times, it might make things worse or cause new problems.
Specific Autoimmune Diseases of Concern
Some autoimmune diseases are more worrying when thinking about stem cell therapy. These include:
- Rheumatoid Arthritis: This disease causes long-term inflammation in the joints. It’s hard to treat with stem cells because it affects the whole body.
- Lupus: This disease can harm many organs and might make stem cell therapy tricky because of immune system issues.
- Multiple Sclerosis: This disease attacks the central nervous system. It’s a big challenge for stem cell therapy, mainly because of the need to control the immune system and repair nerves.
It’s key to know the specific autoimmune disease and how severe it is to decide if stem cell therapy is right. A detailed look at the patient’s health history and current state is needed to weigh the risks and benefits.
Infection Risks: Acute and Chronic Infections
It’s key to check for infection risks before starting stem cell therapy. Infections can affect how well and safely the treatment works.
Active Infections as Barriers to Treatment
Active infections are a big worry for those getting stem cell therapy. They can cause problems like infection spread, slow healing, and bad reactions to the treatment. People with active infections are usually told to wait until their infection clears up.
The kind of infection matters too. For example, bacterial infections might need a different plan than viral ones. Doctors look at the infection’s type and how bad it is to decide what to do next.
HIV, Hepatitis, and Other Chronic Infectious Diseases
Chronic diseases like HIV and hepatitis bring their own set of challenges. They can mess with the immune system, changing how the body reacts to stem cells. People with these diseases need a careful look at the risks and benefits of stem cell therapy.
Handling chronic diseases means more than just treatment. It also means regular checks and possibly antiviral meds. For HIV, antiretroviral therapy (ART) is key to managing the disease and lowering risks. Hepatitis patients might also need antiviral meds to keep their disease in check.
In short, infection risks are a big deal for stem cell therapy patients. Knowing about acute and chronic infections helps doctors take better care of their patients and get the best results.
Age-Related Considerations and Limitations
The age of a patient is key when thinking about stem cell therapy. As this therapy grows, knowing how age affects it is vital. This is important for doctors and those considering treatment.
Age as a Factor in Stem Cell Therapy Success
Age can greatly change how well stem cell therapy works. Biological changes with aging can impact treatment success. For example, older people might have more health issues or less ability to heal.
Younger patients, like kids, might do better with the therapy. They are generally healthier and can heal faster. But, doctors must think about how it might affect their growth and development.
Special Considerations for Pediatric and Geriatric Patients
Kids getting stem cell therapy need extra care because of their age. Doctors must think about how it might affect their growth and safety. They also need to consider long-term effects.
Older adults face unique challenges with stem cell therapy. Common health problems in older adults, like heart disease or diabetes, can change how well the treatment works. So, a detailed check is needed to see if it’s right for them.
In summary, age is very important for stem cell therapy success and suitability. By understanding these age-related factors, doctors can make treatments better fit each patient. This helps improve results for people of all ages.
Pregnancy and Reproductive Considerations
Women who are pregnant or planning to get pregnant need to know about stem cell therapy. This treatment uses stem cells to fix or replace damaged cells. But, it’s important to think carefully about using it when you’re pregnant or planning to have a baby.
Risks for Pregnant Women and Developing Fetuses
Pregnant women thinking about stem cell therapy should know the risks. The therapy changes cells, which could be risky for the baby. Research is ongoing to fully understand these risks, but it’s key to talk to a doctor first.
There are worries about how stem cells might affect the baby’s growth or introduce genetic changes. Even though we don’t know all the risks yet, caution is advised for pregnant women considering this treatment.
Fertility Concerns and Stem Cell Treatment
Fertility is another big thing to think about with stem cell therapy. If you’re planning to have kids in the future, it’s important to know how this treatment might affect you. Some treatments could harm your reproductive health or change your body’s immune system.
It’s important to talk to your doctor about your plans to have kids. They can help you understand any risks to your fertility. Personalized advice based on your health and treatment plans can help reduce risks.
Medication Interactions and Contraindications
When looking at stem cell therapy, it’s key to think about medication interactions. The safety and success of the treatment can be affected by the medicines a patient takes.
Blood Thinners and Anticoagulants
People on blood thinners or anticoagulants face a higher risk of bleeding. These drugs can make it hard for the body to clot, leading to too much bleeding.
Medicines like warfarin, heparin, and aspirin are examples. Whether to stop or change these drugs before treatment depends on the patient’s health and the risk of blood clots.
Immunosuppressive Medications
Immunosuppressive medications can change how the body reacts to stem cell therapy. Patients on these drugs might have a weaker immune system, affecting treatment results.
It’s important to weigh the benefits of stem cell therapy against the risks for those on immunosuppressants. They might need to adjust their medication before treatment.
Required Medication Adjustments Before Treatment
Often, medication adjustments are needed before stem cell therapy. This could mean stopping some drugs or changing their dose to lower risks.
The exact changes needed depend on the drug, the patient’s health, and the type of stem cell therapy. A healthcare expert must carefully evaluate each case to find the right solution.
Severe Organ Dysfunction and End-Stage Disease
Stem cell therapy for severe organ issues or end-stage disease needs careful thought. People with failing organs or terminal illnesses face big challenges. These must be considered to ensure treatment is safe and works well.
Liver and Kidney Disease Considerations
Liver and kidney diseases play a big role in deciding if stem cell therapy is right. Patients with severe liver dysfunction might face more risks. This is because the liver is key in breaking down drugs and toxins. Kidney disease can also make it hard for the body to clear waste, adding to the therapy’s challenges.
Doctors say, “A detailed check of the patient’s health is needed before stem cell therapy. This is to see if the benefits are worth the risks for those with liver or kidney issues.”
This careful look is key to deciding if stem cell therapy is right for these patients.
Heart and Lung Conditions That Increase Risk
Heart and lung problems are also important to think about. People with severe heart failure or long-term lung diseases might face more risks with stem cell therapy. These organs are vital, and their health must be closely watched.
- Heart failure
- Chronic obstructive pulmonary disease (COPD)
- Pulmonary fibrosis
These conditions need careful management and monitoring to lessen the risks of stem cell therapy.
Neurological Disorders and Limitations
Neurological disorders add another level of complexity. Diseases like Parkinson’s disease, multiple sclerosis, and amyotrophic lateral sclerosis (ALS) are hard to treat with stem cells. The chance of bad effects or not working well must be thought about.
“The complexity of neurological disorders often requires a multidisciplinary approach to determine the suitability of stem cell therapy,” as emphasized by healthcare experts.
Psychological and Compliance Factors
Psychological factors and compliance are key in deciding if stem cell therapy is right for someone. This treatment is complex. It needs a deep medical check and a look at the patient’s mental state and ability to follow up.
Mental Health Considerations
The mental health of a patient is very important when considering stem cell therapy. Some mental health issues might make it hard for a patient to stick to the treatment plan. Or, they could get worse with the treatment.
Healthcare providers must do a detailed psychological check. They need to find out if any mental health problems could affect the treatment’s success. This might mean talking to mental health experts to make sure the patient is mentally stable enough for the therapy.
Patient Compliance and Follow-up Requirements
Patient compliance is also very important for stem cell therapy to work well. Patients must be able to follow the treatment plan and keep all their follow-up appointments. If they don’t, the treatment might not work as well, or there could be more risks.
The follow-up steps for stem cell therapy include watching for side effects, checking how the treatment is working, and making any needed changes. Patients need to be serious about following these steps to get the best results.
In short, while stem cell therapy has great benefits, it’s vital to check if a patient is mentally ready and can follow the treatment plan. This helps make sure the treatment is safe and works well.
Unrealistic Expectations: When Stem Cell Therapy Isn’t the Answer
Stem cell therapy is becoming more popular, but it’s important to have realistic hopes. It’s not right for everyone. Like any medical treatment, it has its limits.
Conditions With Poor Response to Stem Cell Treatment
Some medical conditions don’t do well with stem cell therapy. For example, advanced degenerative diseases might not see much improvement. A study in the Journal of Stem Cell Research found that late-stage conditions often don’t get better much.
Examples of conditions with limited response include:
- Advanced osteoarthritis
- Late-stage Parkinson’s disease
- Certain types of chronic liver disease
It’s important to remember that stem cell therapy is not a cure-all. a leading researcher, says, “Stem cell therapy is promising, but it’s not for every condition. Patients should know what to expect based on science.”
“The key to successful stem cell therapy lies in proper patient selection and understanding the limitations of the treatment.” -Stem Cell Researcher
Managing Patient Expectations vs. Scientific Evidence
It’s key to manage what patients hope for in stem cell therapy. Doctors must balance the hope for new treatments with what science shows. This means talking to patients and teaching them about what stem cell therapy can and can’t do.
Patients should know that:
- Stem cell therapy is a growing field.
- Not all conditions respond the same way to treatment.
- Science is key to knowing if stem cell therapy works for certain conditions.
By matching what patients hope for with what science says, doctors can help. This way, stem cell therapy can be used in a more informed and realistic way. As research keeps going, we’ll learn more about what it can do and what it can’t.
Ethical and Regulatory Considerations
Ethical and regulatory rules are key in stem cell therapy. They affect how well treatments work and how safe they are for patients. These rules vary a lot from one place to another.
Knowing the difference between FDA-approved treatments and experimental ones is important. FDA-approved treatments have gone through lots of tests to show they are safe and work well. Experimental treatments might be new and interesting, but they haven’t been tested as much.
FDA Approved vs. Experimental Treatments
Patients thinking about stem cell therapy need to know the difference between FDA-approved and experimental treatments. Approved treatments have been tested a lot and are known to be safe and effective.
- FDA-approved stem cell therapies are for specific health problems, like some blood issues or bone injuries.
- Experimental treatments might help but are not proven safe or effective yet.
International Treatment Options and Risks
Some people look for stem cell therapy in other countries. They might find treatments not approved in their country or ones that are experimental. This could be risky.
Looking for treatment abroad can mean different care standards, no follow-up, and legal issues. It’s important to know the laws and care standards of the country you’re going to.
In short, understanding the rules and ethics of stem cell therapy is important. Patients need to know the treatment’s status and where it’s given. This helps them make choices that weigh the benefits against the risks.
Conclusion: Making Informed Decisions About Stem Cell Therapy
Stem cell therapy is a new hope in regenerative medicine. It offers hope for many medical conditions. But, it’s important to know the good, bad, and what it can’t do before trying it.
We’ve looked at the basics and uses of stem cell therapy. We’ve also talked about when it might not work. Knowing these things helps you make smart choices.
Thinking about stem cell treatment? Talk to a doctor first. They can tell if it’s right for you. This way, you know if it fits your health needs.
Stem cell therapy could change medicine a lot. By learning and working with doctors, you can get its benefits safely.
FAQ
What are stem cell injections?
Stem cell injections put stem cells into the body to help heal and grow new tissues. These cells can turn into different types of cells. This makes them useful for treating many health issues.
How does stem cell therapy work?
Stem cell therapy uses the healing power of stem cells to fix or replace damaged tissues. It uses stem cells from sources like bone marrow, fat tissue, or umbilical cord blood.
What are the benefits of stem cell therapy?
Stem cell therapy can help grow new tissues, reduce swelling, and improve health. It’s being studied for treating bone problems, autoimmune diseases, and other degenerative conditions.
Who is not a good candidate for stem cell therapy?
People with active cancer, severe organ problems, or chronic infections might not be good candidates. Also, those with high hopes but can’t follow treatment plans are not suitable.
What is the screening process for stem cell therapy?
The screening process includes a detailed medical history, physical check-up, and tests to see if treatment is right.
Are there any risks associated with stem cell therapy?
Yes, there are risks like bad reactions, infections, or unexpected problems. It’s important to talk about these risks and benefits with your doctor.
How do autoimmune diseases affect stem cell therapy outcomes?
Autoimmune diseases can make stem cell therapy less effective. Conditions like rheumatoid arthritis or lupus need special care.
Can stem cell therapy be used during pregnancy?
No, stem cell therapy is not usually recommended during pregnancy because of risks to the baby. Talk to your doctor about your plans to have children.
How do medications interact with stem cell therapy?
Some medicines, like blood thinners or drugs that suppress the immune system, can affect stem cell therapy. Always tell your doctor about all the medicines you’re taking.
References
- U.S. Food and Drug Administration. (2023). Stem cell therapy.
- International Society for Stem Cell Research. (2023). Patients and public.