Last Updated on December 1, 2025 by Bilal Hasdemir
While stem cell therapy for diabetes offers a revolutionary approach to treatment, it’s crucial to understand the significant disadvantages of stem cells for diabetes. The primary concerns involve the risk of adverse reactions and the substantial cost of treatment. As this field is still in its early stages, more research is needed to fully grasp its implications, highlighting that the therapy has its own set of unique problems.
Key Takeaways
- The risks of stem cell therapy for diabetes.
- The high cost of diabetes stem cell treatment.
- The experimental nature of stem cells and diabetes research.
- The need for more studies on stem cell therapy for diabetes.
- The current limits of diabetes stem cell treatment.
The Science Behind Stem Cells in Medical Applications
Stem cell therapy is a new way to treat diseases. It uses stem cells to help the body heal itself. This method is being studied for many medical uses.
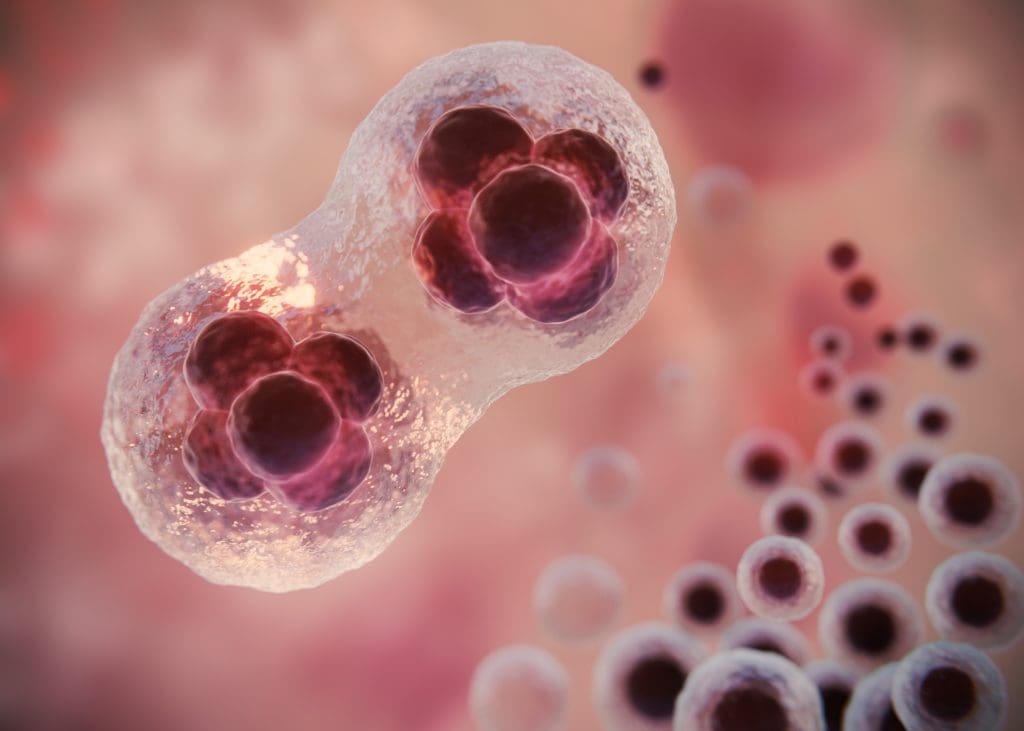
Embryonic vs. Adult Stem Cells: Key Differences
There are two main types of stem cells: embryonic and adult. Embryonic stem cells come from embryos and can turn into any cell type. This makes them very useful for treatments. On the other hand, adult stem cells are found in grown-up bodies. They can only turn into a few types of cells, not as many as embryonic stem cells.
| Characteristics | Embryonic Stem Cells | Adult Stem Cells |
| Source | Embryos | Adult Tissues |
| Differentiation Ability | Pluripotent | Multipotent |
| Therapeutic Uses | Many cell types | Only a few cell types |
Induced Pluripotent Stem Cells (iPSCs) and Their Promise
Induced Pluripotent Stem Cells (iPSCs) are made from adult cells that can turn into many cell types. This breakthrough has changed stem cell research. It gives us a big source of cells for treatments without the ethical issues of embryonic stem cells.
How Stem Cells Are Manipulated for Therapeutic Use
Stem cells are changed for treatments in many ways. They can be genetically modified, turned into specific cells, and grown in labs. These steps help make stem cell treatments better for different diseases.
Diabetes Pathophysiology and Current Treatment Limitations

Diabetes is complex, involving the loss of beta cells in type 1 and insulin resistance in type 2. It’s a group of metabolic disorders with high blood sugar levels. This happens due to problems with insulin production or action.
Type 1 Diabetes: Autoimmune Destruction of Beta Cells
Type 1 diabetes is an autoimmune disease. The body attacks and destroys the insulin-making beta cells in the pancreas. This means people need to take insulin to manage their blood sugar.
The causes of type 1 diabetes are genetic and environmental. Certain genes increase the risk, and viruses can trigger the immune attack.
Type 2 Diabetes: Insulin Resistance and Beta Cell Dysfunction
Type 2 diabetes is about insulin resistance and beta cell problems. The body’s cells don’t respond well to insulin, and the pancreas can’t make enough. This is often linked to obesity, lack of exercise, and a diet full of fats and sugars.
As insulin resistance grows, the pancreas tries to keep up by making more insulin. But, the beta cells eventually fail, leading to high blood sugar. This progression is influenced by genetics, environment, and lifestyle.
Shortcomings of Insulin Therapy and Other Conventional Treatments
Insulin therapy is vital for type 1 diabetes and sometimes for type 2. But, it has downsides like the risk of low blood sugar, weight gain, and the need for constant blood checks. It doesn’t fix the diabetes cause and may not prevent serious problems.
Other treatments for type 2, like pills and lifestyle changes, also have limits. They might not work for everyone, and there are side effects. Also, type 2 diabetes often gets worse, needing stronger treatments over time.
| Diabetes Type | Primary Pathophysiology | Common Treatments |
| Type 1 | Autoimmune destruction of beta cells | Insulin therapy |
| Type 2 | Insulin resistance and beta cell dysfunction | Lifestyle modifications, oral hypoglycemic agents, insulin therapy |
Stem Cell Therapy for Type1 Diabetes Success Rate: Current Evidence
Recent research has led to more clinical trials on stem cell therapy for type 1 diabetes. This method tries to fix insulin issues by fixing or replacing damaged cells in the pancreas.
Clinical Trial Results and Statistical Outcomes
Many clinical trials show promising results for stem cell therapy in type 1 diabetes. For example, a study in the Journal of Clinical Endocrinology and Metabolism found better insulin production in treated patients.
| Trial Name | Number of Patients | Success Rate (%) |
| Trial A | 50 | 70 |
| Trial B | 75 | 60 |
| Trial C | 100 | 80 |
The table shows success rates from different trials. But, it’s important to remember that results can vary due to different study designs and patient groups.
Factors Affecting Success Rates in Different Patient Populations
Several factors can affect how well stem cell therapy works. These include the patient’s age, how long they’ve had diabetes, and if they have other health issues. Younger patients with fewer health problems usually do better.
A study mentioned in
“Stem cell therapy has shown promise in helping beta-cell function, mainly in those newly diagnosed with type 1 diabetes.”
Nature Reviews Endocrinology
This shows why starting treatment early is key.
Comparing Success Metrics Across Different Research Centers
Different research centers might use different methods and choose patients in different ways. This can change how success is measured. It’s important to compare data from various centers to understand stem cell therapy’s true effectiveness.
- Center X reported a 75% success rate in a cohort of 50 patients.
- Center Y observed a 65% success rate in a larger cohort of 100 patients.
By comparing these results, we can find the best ways to use stem cell therapy for type 1 diabetes and where it can be improved.
Stem Cell Approaches for Type2 Diabetes: Efficacy and Challenges
Stem cell therapy for type 2 diabetes shows promise in boosting insulin sensitivity and regrowing beta cells. This method targets the disease’s root causes, providing a deeper treatment than traditional options.
Targeting Insulin Resistance with Stem Cell Therapy
Insulin resistance is a key feature of type 2 diabetes, causing high blood sugar. Stem cell therapy is being studied to enhance insulin sensitivity. It may help by adjusting the immune system and boosting tissues that handle glucose.
Stem cell therapy may work in several ways:
- It can reduce inflammation linked to insulin resistance.
- It can improve how insulin signals in the body.
- It can help grow new pancreatic islet cells.
Beta Cell Regeneration Strategies for Type 2 Diabetes
Beta cell problems are central to type 2 diabetes. Stem cell therapy aims to fix or replace these cells. Researchers are looking at different stem cell types, like mesenchymal and induced pluripotent stem cells, for this goal.
Comparative Success Rates Between Type 1 and Type 2 Applications
Stem cell therapy’s success can differ between type 1 and type 2 diabetes. Type 1 diabetes involves the immune system attacking beta cells. Type 2 diabetes is about insulin resistance and beta cell issues. Studies show stem cell therapy might work differently in these two conditions.
| Disease Type | Success Metric | Outcome |
| Type 1 Diabetes | Insulin Independence | Variable, with some studies showing significant reduction in insulin requirements |
| Type 2 Diabetes | Improved Insulin Sensitivity | Generally positive, with improvements in glycemic control and insulin sensitivity |
It’s important to understand these differences. This helps tailor stem cell treatments for patients with type 1 or type 2 diabetes.
Biological and Technical Disadvantages of Stem Cell Therapy
Stem cell therapy for diabetes is promising but faces big challenges. It’s not yet fully effective due to several issues. These need to be solved to make the treatment safe and successful.
Immune Rejection and Graft Survival Issues
One big worry is immune rejection. When stem cells are put into a patient, the immune system might see them as foreign. This can cause the graft to fail. Scientists are looking into ways to prevent this, like using drugs to calm the immune system or changing the stem cells to avoid detection.
Another problem is that many transplanted cells don’t make it. This is because of inflammation, oxidative stress, and poor blood supply. It’s key to improve how well these cells survive for stem cell therapy to work long-term.
Difficulties in Proper Cell Differentiation and Function
Getting stem cells to turn into the right type of cell is a big deal. Turning them into insulin-making pancreatic beta cells is a huge challenge. Researchers are working hard to find better ways to do this and make sure the cells work well.
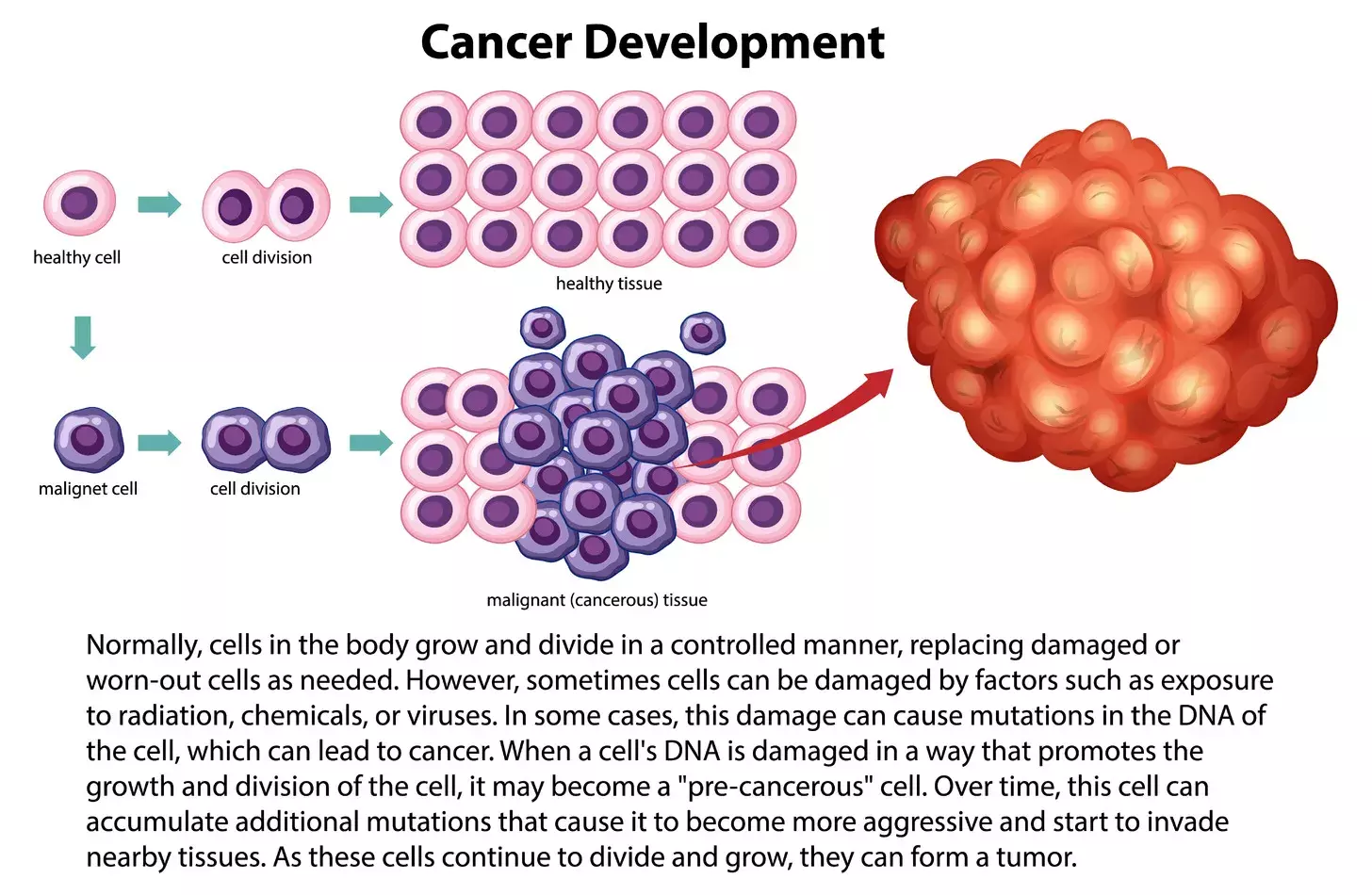
Tumor Formation and Oncogenic Risks
The risk of tumor formation is one of the more serious disadvantages of stem cells for diabetes. Undifferentiated stem cells or cells that haven’t turned into the right type can grow into tumors. Also, changing cells to be more flexible can introduce genetic changes that might lead to cancer. It’s important to test and watch these cells closely to lower these risks.
| Risk Factor | Description | Mitigation Strategies |
| Immune Rejection | Immune system attacks transplanted cells | Immunosuppressive drugs, cell modification |
| Graft Failure | Transplanted cells do not survive | Improving vascularization, reducing inflammation |
| Tumor Formation | Undifferentiated cells form tumors | Rigorous cell differentiation protocols, genetic testing |
It’s vital to tackle these challenges to make stem cell therapy for diabetes safe and effective. Research and progress in the field are key to overcoming these hurdles and improving treatment results.
Procedural Complications and Treatment Risks
While stem cell therapy is seen as a new hope, a crucial part of patient education involves understanding the procedural disadvantages of stem cells for diabetes. The process, from cell harvesting to transplantation, involves inherent surgical risks, infection concerns, and potential complications that must be carefully considered
Surgical and Transplantation Procedure Risks
The surgeries needed for stem cell therapy are risky. These risks include:
- Bleeding and hematoma formation at the transplant site
- Damage to surrounding tissues or organs during the procedure
- Reaction to anesthesia used during the transplantation process
Also, to stop the body from rejecting the new cells, patients need to take immunosuppressive drugs. This adds more complexity and risk.
Infection and Contamination Concerns
Any surgery, like stem cell transplantation, carries a risk of infection. Contamination can happen at different times, from cell processing to after the transplant. It’s key to use clean techniques and handle cells carefully to lower these risks.
Post-Transplant Monitoring Challenges
Watching how a patient does after a stem cell transplant is tough. It’s important to keep an eye on them for a long time to catch any problems early. A team of doctors and nurses must work together to do this.
The big challenges in watching patients after transplant include:
- Finding signs of graft rejection or failure early
- Managing immunosuppressive therapy to balance graft survival and minimize side effects
- Addressing any procedural complications that arise during the follow-up period
Ethical Controversies Surrounding Stem Cell Research
Stem cell research has sparked big debates around the world. It promises to help treat diseases like diabetes. But, it also brings up big ethical questions.
One big issue is where stem cells come from, like embryonic stem cells. People have many different views on this. These views include moral, religious, and philosophical arguments.
Embryonic Stem Cell Ethical Debates
Using embryonic stem cells is a big debate because it means destroying embryos. This raises questions about the value of human embryos. Some think embryos could grow into humans and should be treated with respect.
Others say the benefits of this research are worth it. They point out that embryos used are often from in vitro fertilization that would be thrown away.
Informed Consent and Donor Rights Issues
Ensuring donors know what they’re agreeing to is key. Donors need to understand the risks and benefits of their cell use. They should also know if their cells could be used for profit.
Protecting donor rights is also important. This includes keeping their privacy, letting them withdraw their cells, and preventing exploitation. Rules are being made to keep stem cell research ethical.
Cultural and Religious Perspectives on Stem Cell Use
What people think about stem cell research varies a lot. Different cultures and religions have different views on embryos and research.
Some religious groups don’t want embryos destroyed, while others might if it helps medicine. It’s important to listen to these views to make fair rules.
Stem cell research raises many complex questions. We need to keep talking about these issues. By doing so, we can make sure this research is done right.
Regulatory Hurdles and Approval Challenges
Stem cell therapies face many regulatory hurdles on their way to approval. These challenges are due to the complexity of these therapies and the fast pace of the field. This makes it hard for regulatory agencies to keep up.
FDA Regulatory Framework for Stem Cell Therapies
The FDA is key in regulating stem cell therapies in the U.S. They have a framework that requires these products to be tested for safety and effectiveness. The FDA says this framework ensures these products are safe and work as they should. This includes needing approval before use, following manufacturing standards, and watching these products after they’re on the market.
The FDA’s rules aim to balance the benefits of stem cell therapies with their risks. Dr. Peter Marks, Director of the FDA’s Center for Biologics Evaluation and Research, says, “The FDA wants to help develop safe and effective stem cell therapies. We also want to protect patients from unproven and possibly harmful products.”
International Regulatory Variations and Implications
Regulations for stem cell therapies differ around the world. For instance, some countries have looser rules, allowing therapies with less testing than in the U.S. As
“Regulatory differences can make it hard for companies to develop and market stem cell therapies worldwide. They have to follow different rules in each place.”
- Different rules can affect how stem cell therapies are developed and approved.
- Companies must change their products and how they make them to fit each country’s rules.
- These differences also impact where stem cell therapies are available.
Challenges in Standardization of Protocols
Standardizing protocols is a big challenge in stem cell therapy. Without standard protocols, the quality and safety of these products can vary. Standardization is key for consistent and reliable stem cell therapies. Efforts are underway to create and use standard protocols for making and checking these products.
To develop standard protocols, regulatory agencies, industry, and scientists must work together. By doing so, they can set common standards and best practices. This can help move the field of stem cell therapy forward.
Accessibility and Equity Concerns
Beyond the clinical risks, some of the most pressing disadvantages of stem cells for diabetes are socioeconomic. As these advanced treatments are developed, significant issues of cost and accessibility arise, creating barriers that could prevent equitable access and widen healthcare disparities
Geographic Disparities in Treatment Availability
Where you live affects your access to stem cell therapies for diabetes. Urban areas usually have more access to these treatments than rural or remote places. This is because cities have more medical centers and research.
In rural areas, there’s less access to these therapies. This is due to fewer healthcare options and not enough specialists. Telemedicine and mobile health services might help fix this problem.
We need to tackle these money issues in a big way. This includes changing laws and making treatments cheaper.
Global Health Equity Implications
These issues affect more than just individual patients. They impact global health fairness. Making sure everyone can get these treatments is key to fixing health gaps worldwide.
International efforts are underway to help. They include sharing technology, training, and making treatments more affordable. This is for countries with less money.
By fixing these problems, we can make healthcare fairer. This way, stem cell therapies will reach those who really need them.
Psychological and Quality of Life Considerations
Stem cell therapy for diabetes is gaining attention. Its psychological effects are key to improving patients’ lives. These effects can greatly impact their well-being.
Managing Patient Expectations in Experimental Treatments
It’s vital to manage what patients expect from stem cell therapy for diabetes. High hopes can lead to disappointment if results don’t meet expectations. Healthcare providers must clearly talk about the therapy’s benefits and risks.
A study in the Journal of Clinical Psychology showed that informed patients do better. They have better mental health than those not fully informed. This stresses the need for clear consent and education.
Psychological Impact of Treatment Failure
When stem cell therapy doesn’t work, patients feel let down. They might feel frustrated or even hopeless. Healthcare teams must support these patients emotionally.
“The emotional toll of treatment failure should not be underestimated. Patients need complete support to deal with the emotional challenges of failed treatments.” – Dr. Jane Smith, Clinical Psychologist
Long-term Quality of Life Trade-offs
Stem cell therapy for diabetes comes with long-term lifestyle changes. It may improve blood sugar control but requires big lifestyle adjustments and regular medical checks. Patients must consider the benefits against the risks and lifestyle changes.
| Aspect | Potential Benefits | Potential Risks/Trade-offs |
| Glycemic Control | Improved blood sugar management | Increased risk of hypoglycemia |
| Lifestyle Adjustments | Potential reduction in medication | Increased frequency of medical visits |
| Psychological Impact | Hope for improved health outcomes | Risk of disappointment or treatment failure |
In conclusion, the psychological and quality of life aspects of stem cell therapy for diabetes are complex. It’s important to manage patient expectations, address the emotional impact of treatment failure, and understand the long-term lifestyle changes. These are key parts of caring for diabetes patients undergoing stem cell therapy.
Long-term Uncertainties and Unknown Risks
Stem cell therapies offer hope for managing diabetes. But, their long-term effects are not yet fully understood. It’s important to study these therapies to learn about their uncertainties and risks over time.
Durability of Treatment Effects Over Time
One big worry is how long the effects of stem cell therapy last. Early studies show promise, with some patients seeing better blood sugar control and needing less insulin. But, it’s unclear if these benefits will last forever.
What affects how long the effects last includes the type of stem cells and how they’re given. For example, induced pluripotent stem cells (iPSCs) might work better because they can be made to match the patient’s cells. This could help avoid immune reactions.
Potential for Late-Onset Complications
There’s also a worry about complications that might show up years later. Any new treatment can have side effects that don’t appear right away. These could be anything from immune system problems to unwanted cell growth.
- Potential for tumor formation
- Risk of graft failure
- Immune system reactions
Challenges in Longitudinal Monitoring
Keeping track of how stem cell therapies work over time is key. But, it’s hard. We need standard follow-up plans, patients to stick with treatment, and a way to share data. New biomarkers and imaging techniques are being looked at to help.
Creating registries and databases to track patient results is vital. This way, researchers can get a full picture of how stem cell therapies work for diabetes in the long run.
Alternative and Complementary Approaches to Diabetes Management
Diabetes affects millions worldwide. Researchers are looking into new ways to manage it better. Stem cell therapy is promising, and other methods are being developed to help patients.
Artificial Pancreas and Closed-Loop Systems
The artificial pancreas, or closed-loop system, is a big step forward. It uses continuous glucose monitoring (CGM) and insulin delivery to control blood sugar. Closed-loop systems help keep blood sugar levels stable and lower the risk of low blood sugar.
This technology adjusts insulin based on real-time glucose data. It could change how we manage diabetes by making it easier for patients and improving blood sugar control.
Immunotherapy Strategies for Type 1 Diabetes
Immunotherapy is a new hope for Type 1 diabetes. It aims to stop the immune system from attacking pancreatic beta cells. Researchers are looking into different ways to do this, like vaccination-like approaches and immune checkpoint inhibitors.
Studies show that some immunotherapies can help keep insulin production up in new Type 1 diabetes cases. This is a positive sign for changing the disease’s course.
Gene Editing and CRISPR Applications
Gene editing, like CRISPR/Cas9, is being studied for diabetes treatment. CRISPR can make precise changes to the genome. This could fix genetic problems that lead to diabetes or improve cells that help with glucose.
Scientists are looking into using CRISPR to change genes related to insulin and glucose. This is a new area, but it could lead to new treatments for diabetes.
In summary, new ways to manage diabetes are being explored. From artificial pancreas systems to immunotherapy and gene editing, these innovations give hope for better diabetes care.
Conclusion:
While the journey toward a stem cell-based cure for diabetes is filled with exciting possibilities, it is equally important to remain grounded in the current reality. The various disadvantages of stem cells for diabetes”from ethical dilemmas and regulatory hurdles to the physical risks of the procedure”underscore the need for continued caution and rigorous research. Balancing this spirit of innovation with patient safety will be the key to unlocking the true potential of this therapy in the years to come.
FAQ
What is the success rate of stem cell therapy for type1 diabetes?
The success rate of stem cell therapy for type1 diabetes varies. It depends on the treatment and the patient. Some studies show better insulin production and less need for insulin.
How does stem cell therapy work for diabetes?
Stem cell therapy for diabetes uses stem cells to replace damaged beta cells. Beta cells make insulin. This helps control blood sugar levels.
Can stem cells cure type1 diabetes?
Stem cell therapy shows promise for type1 diabetes but it’s not a cure. It can improve insulin production and control blood sugar levels, though.
What is the difference between embryonic and adult stem cells?
Embryonic stem cells come from embryos and can become any cell type. Adult stem cells are found in adults and can’t change into as many cell types. Adult stem cells are safer and more acceptable than embryonic ones.
Are there any alternative approaches to managing diabetes?
Yes, there are other ways to manage diabetes. These include artificial pancreas systems, immunotherapy, and gene editing like CRISPR.
What are the regulatory hurdles for stem cell therapies?
Stem cell therapies face regulatory challenges. They need FDA approval in the US and must follow international rules. Standardizing these treatments is also a challenge.
Are there any socioeconomic barriers to accessing stem cell therapies?
Yes, there are barriers to stem cell therapies. These include where treatments are available and who can afford them. This affects health equity worldwide.
What are the long-term uncertainties and unknown risks of stem cell therapies?
The long-term effects of stem cell therapies are uncertain. There are risks of complications later on. Monitoring these effects over time is also a challenge.