Last Updated on November 25, 2025 by Ugurkan Demir

Coronary artery disease (CAD) can cause serious health problems. These include heart attack, heart failure, and arrhythmias. It’s important for patients to know about these complications and the risks of cardiac catheterization.Find out what are the major complications of coronary artery disease and how cardiac catheterization risks are managed.
At Liv Hospital, we focus on advanced care that puts patients first. Cardiac catheterization is a key procedure for diagnosing and treating heart issues. It involves putting a catheter into a heart vessel or chamber. We aim to provide top-notch care for CAD and reduce risks from cardiac catheterization.
Key Takeaways
- Coronary artery disease can lead to serious complications, including heart attack and heart failure.
- Cardiac catheterization is a common procedure used to diagnose and treat cardiovascular conditions.
- Understanding the risks associated with cardiac catheterization is important for patients.
- Liv Hospital provides advanced care with a patient-centered approach.
- Comprehensive care is essential in managing CAD and minimizing risks.
Understanding Coronary Artery Disease (CAD)
It’s important to understand Coronary Artery Disease (CAD) to tackle its global health impact. CAD happens when the coronary arteries narrow or block due to atherosclerosis. This is when plaque builds up inside the arteries.
Pathophysiology of CAD
The pathophysiology of CAD is complex. Atherosclerosis is when plaque, made of fat, cholesterol, and more, builds up in arteries. This can narrow or block the arteries, cutting off blood to the heart.
Many factors lead to atherosclerosis. These include high blood pressure, high cholesterol levels, smoking, and diabetes. These can damage the artery lining, making it easier for plaque to stick.
Prevalence and Impact on Global Health
CAD is a common heart disease and a major cause of illness and death worldwide. Millions suffer from CAD, and its numbers are expected to rise. This is due to aging populations and more obesity and diabetes.
CAD’s impact on global health is huge. It affects many people and costs healthcare systems a lot. Treatment and management are expensive, including medicines, surgeries, and lifestyle changes.
| Region | Prevalence of CAD | Estimated Annual Deaths |
| North America | High | 400,000+ |
| Europe | High | 500,000+ |
| Asia | Moderate to High | 1,000,000+ |
Knowing CAD’s prevalence and impact shows we need more research, awareness, and prevention. This is key to fighting this disease.
What Are the Major Complications of Coronary Artery Disease?
Coronary Artery Disease (CAD) can lead to serious health problems. These include heart attack, heart failure, arrhythmias, stroke, and sudden cardiac death. These issues can greatly affect a patient’s life and even lead to death.
Overview of CAD Complications
The complications of CAD are complex and can greatly impact a patient’s life. A heart attack happens when a blockage cuts off blood to the heart, causing damage. Heart failure occurs when the heart can’t pump enough blood for the body’s needs.
Arrhythmias, or irregular heartbeats, can also happen due to CAD. These can be mild or life-threatening. CAD also raises the risk of stroke, which is when the brain doesn’t get enough oxygen and nutrients.
Risk Factors for Developing Complications
Several factors increase the risk of CAD complications. These include hypertension, diabetes mellitus, high cholesterol, smoking, and a family history of heart disease. It’s important to manage these risk factors to prevent CAD complications.
We suggest a detailed approach to managing CAD. This includes lifestyle changes and, if needed, medication to control risk factors. Understanding CAD complications and their risk factors helps healthcare providers create better treatment plans.
Heart Attack (Myocardial Infarction)
A heart attack, or myocardial infarction, is a serious condition. It happens when blood flow to the heart is blocked. This blockage can damage or kill heart muscle because of lack of oxygen and nutrients.
Mechanism and Presentation
A heart attack usually starts with a rupture of a plaque in a coronary artery. This rupture causes a blood clot (thrombosis) that blocks blood flow. Symptoms include chest pain or discomfort, shortness of breath, nausea, and fatigue. Symptoms can be different in women, older adults, and people with diabetes.
“The sooner a heart attack is diagnosed and treated, the better the chances of survival and minimizing damage to the heart muscle,” emphasizes the importance of prompt medical intervention.
Long-term Consequences
The long-term effects of a myocardial infarction can be serious. Heart failure is a common complication, where the heart can’t pump enough blood. Arrhythmias, or irregular heartbeats, can also happen. Plus, the risk of more heart problems increases after a heart attack.
Managing and preventing these risks is key. This includes making lifestyle changes, taking medication, and seeing healthcare providers regularly.
We know a heart attack can change lives, not just for the patient but for their loved ones too. Our healthcare team is dedicated to giving full care and support. We aim to help patients recover and manage their condition well.
Heart Failure as a Complication of CAD
Heart failure is a big problem caused by CAD. It happens when the heart can’t pump enough blood. This makes life much harder and needs careful handling.
Systolic vs. Diastolic Heart Failure
Heart failure comes in two main types: systolic and diastolic. Systolic heart failure means the heart can’t contract well. This leads to less blood being pumped out. Diastolic heart failure is when the heart can’t relax and fill up properly.
Knowing which type you have is key to finding the right treatment. Systolic heart failure often means the heart’s left ventricle doesn’t pump well. Diastolic heart failure means the heart can’t fill up right, even if it pumps okay.
Management Approaches
Managing heart failure involves many steps. This includes medicines, changes in lifestyle, and devices. Medicines like ACE inhibitors and beta-blockers help control symptoms and slow the disease.
- Changing your diet, being more active, and quitting smoking are important lifestyle changes.
- Some patients might need devices like pacemakers or ICDs.
Handling heart failure well means tailoring a plan for each patient. This plan considers the patient’s health, other conditions, and what they prefer. With the right plan, heart failure patients can live better lives.
Arrhythmias Associated with Coronary Artery Disease
Arrhythmias are a common problem with Coronary Artery Disease. They affect the heart’s rhythm and function. These irregular heartbeats can happen because of ischemia or scar tissue from CAD.
Types of Arrhythmias in CAD
There are several arrhythmias linked to CAD, including:
- Atrial Fibrillation: A rapid and irregular heart rhythm from the atria.
- Ventricular Tachycardia: A fast heart rate from the ventricles, which can be dangerous.
- Ventricular Fibrillation: A severe arrhythmia where the ventricles fibrillate instead of beating right.
These arrhythmias can cause serious health issues and even death if not treated.
Detection and Treatment Options
To find arrhythmias in CAD patients, we use:
- Electrocardiography (ECG): A non-invasive test that records the heart’s electrical activity.
- Holter Monitoring: A 24-hour ECG monitoring to catch arrhythmias that happen sometimes.
- Event Monitoring: Longer monitoring to record arrhythmic events.
For treating arrhythmias in CAD, we have:
- Medications: Anti-arrhythmic drugs to control the heart rhythm.
- Device Therapy: Pacemakers or ICDs to manage arrhythmias.
- Catheter Ablation: A procedure to destroy abnormal electrical pathways in the heart.
We choose the best treatment for each patient. We look at the type and severity of the arrhythmia and the patient’s health.
Stroke and Other Thromboembolic Events
It’s important to know how CAD and stroke are connected. This knowledge helps us create better ways to prevent strokes and improve patient care. Coronary Artery Disease can cause blood clots that may travel to the brain, leading to a stroke.
Relationship Between CAD and Stroke Risk
The connection between CAD and stroke risk is complex. Many factors play a role in increasing the chance of blood clots in the brain. We will look at these factors closely.
- Atherosclerosis: The buildup of plaque in arteries, a sign of CAD, can cause blood clots.
- Cardiac Sources of Embolism: Conditions like atrial fibrillation, linked to CAD, raise the risk of clots.
- Shared Risk Factors: Hypertension, diabetes, and smoking are common risks for both CAD and stroke.
Prevention Strategies
To prevent stroke and thromboembolic events in CAD patients, we need a variety of approaches. Here are some strategies we suggest:
- Anticoagulation Therapy: Medications that stop blood clotting or break up clots.
- Lifestyle Modifications: Eating right, exercising, and quitting smoking can greatly reduce risk.
- Management of Risk Factors: It’s key to control hypertension, diabetes, and high cholesterol.
By understanding the link between CAD and stroke risk, and using these prevention strategies, we can greatly improve outcomes for heart disease patients.
Sudden Cardiac Death in CAD Patients
Coronary artery disease (CAD) greatly raises the risk of sudden cardiac death. This is a major cause of death globally. It often happens due to abnormal heart rhythms or cardiac arrest in those with CAD.
Risk Stratification
It’s vital to spot patients at high risk of sudden cardiac death early. Factors like poor heart function, history of abnormal heart rhythms, and how severe CAD is play a big role.
| Risk Factor | Description | Impact on Risk |
| Left Ventricular Dysfunction | Reduced ejection fraction indicating poor heart function | High |
| Ventricular Arrhythmias | Abnormal heart rhythms originating in the ventricles | High |
| Extent of CAD | Number and severity of coronary artery blockages | Moderate to High |
Those with these risk factors need close monitoring. This helps assess their risk of sudden cardiac death.
Preventive Measures
There are steps to lower the risk of sudden cardiac death in CAD patients. These include using implantable cardioverter-defibrillators (ICDs), certain medications, and making lifestyle changes.
- Implantable Cardioverter-Defibrillators (ICDs): Devices that can detect and correct life-threatening arrhythmias.
- Medications: Beta-blockers and anti-arrhythmic drugs to manage arrhythmias and reduce risk.
- Lifestyle Modifications: Dietary changes, exercise, and smoking cessation to improve overall heart health.
By knowing the risk factors and taking preventive steps, we can lower sudden cardiac death rates in CAD patients.
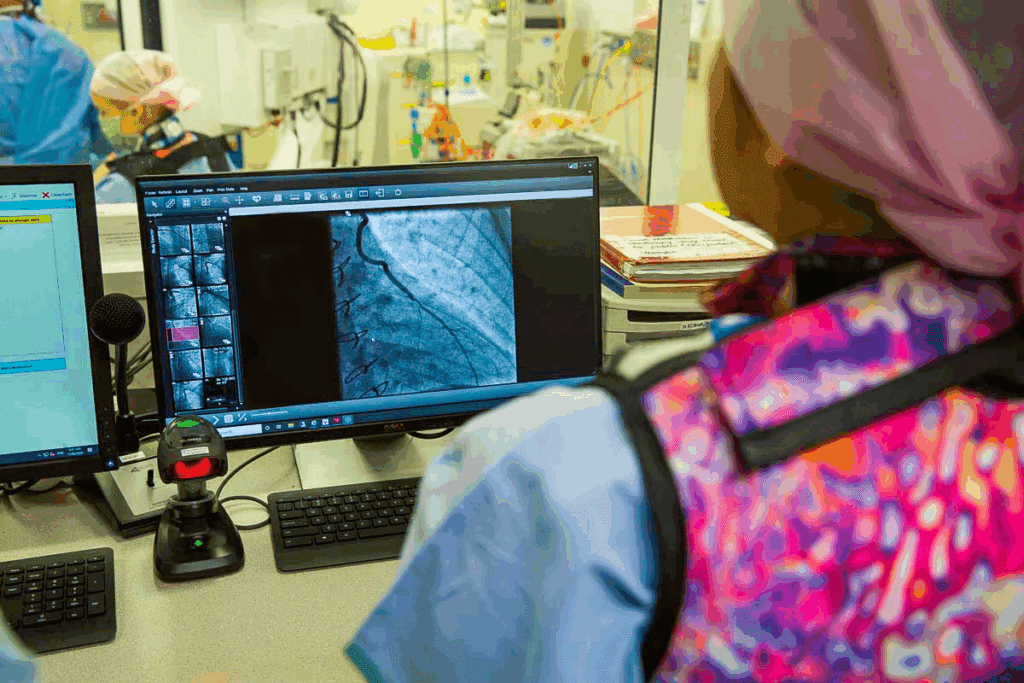
Cardiac Catheterization: Procedure and Indications
Cardiac catheterization is a key tool for checking heart health. It involves putting a catheter into a blood vessel, usually in the groin or arm. Then, it’s guided to the heart.
This method is widely used for managing coronary artery disease (CAD) and other heart issues. It helps doctors see the coronary arteries, check the heart’s function, and do interventions when needed.
Diagnostic vs. Interventional Catheterization
Cardiac catheterization comes in two types: diagnostic and interventional. Diagnostic catheterization helps find blockages and check heart function. It gives insights into the heart’s structure. Interventional catheterization, on the other hand, includes procedures like angioplasty and stenting to open blocked or narrowed arteries.
Choosing between these two types depends on the patient’s condition and what information is needed. Sometimes, a diagnostic test might lead to an interventional one if a treatable condition is found.
| Procedure | Diagnostic Catheterization | Interventional Catheterization |
| Purpose | Diagnose heart conditions | Treat heart conditions |
| Common Uses | Coronary angiography, assessing heart function | Angioplasty, stenting, treating blockages |
When Is Cardiac Catheterization Necessary?
It’s needed for patients with suspected or confirmed coronary artery disease. This includes those with symptoms like chest pain or shortness of breath. It’s also for patients who have had a heart attack or are at high risk of heart problems.
The decision to do cardiac catheterization is based on a detailed evaluation. This includes looking at the patient’s medical history, symptoms, and results from tests like electrocardiograms (ECGs) and stress tests.
Understanding the indications and types of cardiac catheterization helps healthcare providers make better decisions. They balance the benefits of the procedure against the risks.
How Safe Is a Heart Catheterization? Addressing Common Concerns
Heart catheterization is mostly safe, but knowing the risks is key. It helps in making smart choices. This method is vital for diagnosing and treating heart disease.
Looking into safety, we must talk about success rates and risks. Many studies and data show heart catheterization is safe.
Success Rates and Safety Statistics
Most heart catheterizations go well without big problems. Studies say less than 2% face complications, and serious ones are rare. This is good news.
But, risks can differ for each person. This depends on health, other diseases, and the procedure type.
Factors That Influence Risk
Several things can change the risk of heart catheterization. Age, kidney disease, diabetes, and heart disease severity matter. So does the doctor’s experience and the hospital’s volume.
Knowing these can help lower risks. For example, those with kidney disease need special care to avoid kidney problems.
Patient Selection and Preparation
Choosing the right patient and preparing them well is critical. This means checking their health history and the procedure’s benefits and risks.
Patients get clear instructions on how to get ready. This includes managing medicines, fasting, and other steps. Proper preparation and selection can greatly reduce risks.
In summary, heart catheterization has some risks, but it’s mostly safe. Taking the right precautions and choosing the right patients can lead to good results.
Complications of Cardiac Catheterization Within 24 Hours
Cardiac catheterization is usually safe but can cause serious problems in the first 24 hours. We will look at the possible issues that can happen during this time.
Bleeding and Vascular Complications
Bleeding is a common issue after cardiac catheterization. It can be minor or severe. Vascular complications include things like hematomas and pseudoaneurysms. These can be treated with proper care and monitoring.
Things that increase the risk of bleeding and vascular problems include:
- Large catheter size
- Anticoagulation therapy
- Sheath size and type
- Patient comorbidities such as hypertension and renal failure
Cardiac Complications
Cardiac issues can happen because of the procedure. These include arrhythmias, cardiac tamponade, and myocardial infarction. Arrhythmias can be mild or serious. Quick action is key to avoid bad outcomes.
The reasons for cardiac problems are:
- Mechanical irritation of the heart chambers and vessels
- Embolic events during the procedure
- Contrast-induced effects on cardiac function
Contrast-Related Complications
Contrast-induced nephropathy (CIN) is a big worry after cardiac catheterization. It’s when kidney function drops after contrast use. Pre-existing renal impairment and diabetes raise the risk of CIN.
Ways to lessen contrast-related problems include:
- Using low-osmolar contrast agents
- Adequate hydration before and after the procedure
- Minimizing the volume of contrast used
Knowing about these complications and their risks is key for healthcare providers. It helps them prevent and manage these issues. This way, we can make sure patients do better and have fewer problems after cardiac catheterization.
Conclusion: Balancing Risks and Benefits in CAD Management
Effective CAD management is all about finding a balance. We’ve looked at the big problems with coronary artery disease and the dangers of cardiac catheterization.
It’s key to have a detailed plan for CAD management. This includes making lifestyle changes, using medicines, and choosing treatments that fit each patient’s needs. Knowing the good and bad of each treatment helps doctors make better choices for their patients.
When managing CAD, it’s important to weigh all the factors. This includes the patient’s health, their medical history, and the risks of tests and treatments like cardiac catheterization.
By focusing on each patient’s needs, we can make CAD management better. This way, we can reduce problems and improve life for those with this condition.
FAQ
What are the major complications of coronary artery disease?
Coronary artery disease can lead to heart attacks, heart failure, and arrhythmias. It also increases the risk of stroke and sudden cardiac death. Knowing these risks helps in managing and preventing them.
How safe is a heart catheterization procedure?
Heart catheterization is usually safe, with low risks of complications. But, like any invasive procedure, there are risks. These include bleeding, vascular issues, and heart problems.
What are the risks associated with cardiac catheterization?
Risks include bleeding, vascular and heart issues, and problems from the contrast used. The risk depends on the patient’s health and how well they are prepared.
What are the symptoms of a heart attack?
Heart attack symptoms vary. They can include chest pain, shortness of breath, and pain in the arms, back, neck, jaw, or stomach.
How is heart failure managed in patients with coronary artery disease?
Managing heart failure involves medications, lifestyle changes, and devices. The goal is to improve symptoms and quality of life.
What are the different types of arrhythmias associated with coronary artery disease?
Arrhythmias include atrial fibrillation, ventricular tachycardia, and ventricular fibrillation. Treatment depends on the type and severity.
How can stroke risk be reduced in patients with coronary artery disease?
Stroke risk can be lowered with anticoagulation therapy, lifestyle changes, and managing risk factors like high blood pressure and high cholesterol.
What are the preventive measures for sudden cardiac death in CAD patients?
Preventive measures include implantable devices, medications, and lifestyle changes. Identifying high-risk patients is key.
What are the complications that can occur within 24 hours after cardiac catheterization?
Complications within 24 hours include bleeding, vascular and heart issues, and problems from the contrast. Quick action is needed to minimize harm.
How can the risks of cardiac catheterization be minimized?
Risks can be lowered by careful patient selection, preparation, and post-procedure care. Advanced technologies, like radial access, also help reduce risks.
What is the relationship between coronary artery disease and stroke risk?
CAD increases stroke risk due to shared risk factors like high blood pressure and atherosclerosis. Managing these factors is vital.
Are heart caths dangerous?
Heart catheterization is generally safe when done by experts in a proper setting. The benefits often outweigh the risks for those who need it.
What are the signs of a groin hematoma after heart cath?
Signs include swelling, pain, and bruising at the access site. Seeking medical help is necessary if these symptoms appear.
How can post-cardiac catheterization complications be managed?
Complications are managed by quick recognition, proper treatment, and sometimes additional interventions. Close monitoring and follow-up care are essential.
References
Complications of coronary artery disease. In Bookshelf – NCBI. https://www.ncbi.nlm.nih.gov/books/NBK355309/