Aortic stenosis is a serious heart condition where the aortic valve narrows. This can lead to heart failure if not treated. It often develops quietly for years, making it key to know its causes and how it progresses.
Age-related calcific degeneration is the main cause, but congenital bicuspid aortic valve and rheumatic heart disease also matter. At Liv Hospital, we see the need for quick action to better patient lives and outcomes.
Knowing the risk factors and symptoms of aortic stenosis is key for early treatment. We aim to offer top-notch healthcare and support for patients from around the world.
Key Takeaways
- Aortic stenosis is mainly caused by age-related calcific degeneration.
- Congenital bicuspid aortic valve and rheumatic heart disease are also big causes.
- Early detection is key to stop it from getting worse.
- Understanding risk factors and symptoms is vital for timely action.
- Liv Hospital offers advanced medical care with a focus on the patient.
Understanding Aortic Stenosis: An Overview
To understand aortic stenosis, we need to look at the aortic valve’s structure and its problems. We’ll dive into the details of the aortic valve and how it can lead to stenosis.
Definition and Anatomy of the Aortic Valve
The aortic valve is key in the heart, controlling blood flow from the left ventricle to the aorta. This ensures oxygen-rich blood reaches the body. It has three cusps that open and close with each heartbeat, ensuring blood flows well.
Aortic stenosis happens when the valve’s cusps become stiff or calcified. This makes it hard for them to open fully. As a result, blood flow is blocked, forcing the heart to work harder. If not treated, it can lead to heart failure.
The Progressive Nature of Aortic Stenosis
Aortic stenosis usually gets worse over time, often taking decades. At first, people might not show any symptoms, making it hard to catch early. But as it gets worse, symptoms like shortness of breath, chest pain, and fainting may appear, showing it’s time to seek medical help.
“Aortic stenosis is a progressive disease with a prolonged latent period, during which patients are often asymptomatic, followed by a symptomatic phase characterized by severe and potentially life-threatening complications.”
The worsening of aortic stenosis can be due to several factors. These include age-related calcification, congenital issues like a bicuspid aortic valve, and other rare causes. Knowing these factors helps in managing the condition better.
| Factor | Description | Impact on Aortic Stenosis |
|---|---|---|
| Age-Related Calcific Degeneration | Calcification of the aortic valve cusps due to aging | Increases the risk of developing aortic stenosis |
| Congenital Bicuspid Aortic Valve | A birth defect resulting in an aortic valve with two cusps instead of three | Predisposes individuals to aortic stenosis at a younger age |
| Rheumatic Heart Disease | Complication of rheumatic fever, leading to valve damage | Can cause aortic stenosis among other valve problems |
Understanding the aortic valve’s anatomy and how aortic stenosis progresses helps us grasp the condition’s complexity. It also highlights the need for early medical treatment.
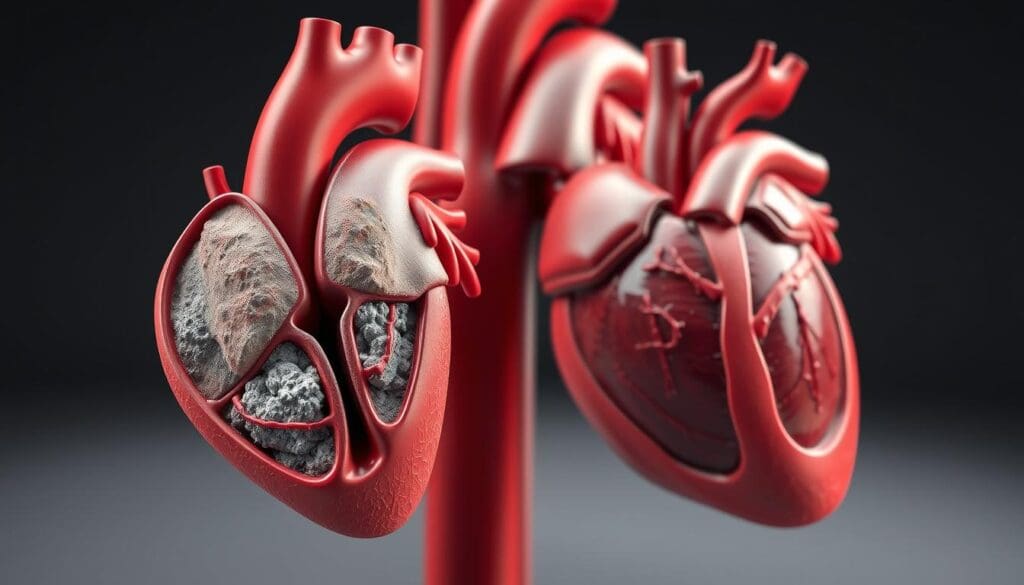
What Causes Aortic Stenosis: Primary Etiologies
Aortic stenosis has many causes, mainly age-related calcification, congenital issues, and rheumatic heart disease. We’ll dive into these main causes to understand how they affect the aortic valve.
Age-Related Calcific Degeneration
Calcific degeneration is the top reason for aortic stenosis in older people. It happens when calcium builds up on the aortic valve, making it stiff and narrow. This buildup is similar to atherosclerosis, caused by inflammation, lipid buildup, and calcification.
Factors like high blood pressure, high cholesterol, and smoking increase the risk of calcific aortic stenosis. As more people age, this condition will become a bigger health issue.
Congenital Bicuspid Aortic Valve
Congenital bicuspid aortic valve is a major cause of aortic stenosis in younger people. It happens when the valve has only two cusps instead of three. This abnormal structure increases the risk of valve problems over time.
People with bicuspid aortic valve often have other heart defects. While some may not show symptoms for years, others may need treatment for valve issues.
Key features of congenital bicuspid aortic valve include:
- Abnormal valve structure with two cusps
- Increased risk of calcification and stenosis
- Association with other congenital heart defects
- Variable age of onset for symptoms
Rheumatic Heart Disease
Rheumatic heart disease is another major cause of aortic stenosis, mainly in areas where rheumatic fever is common. The inflammation from rheumatic fever can scar and stiffen the valve, causing stenosis.
This disease often affects the mitral valve more, but it can also harm the aortic valve. When it does, it can lead to severe stenosis, needing surgery.
Rheumatic heart disease is a big problem worldwide, hitting low-income countries hard. It’s important to fight rheumatic fever to reduce the impact of rheumatic heart disease, including aortic stenosis.
Less Common Causes of Aortic Stenosis
There are several rare conditions that can cause aortic stenosis. These less common causes are important to understand fully.
Infective Endocarditis
Infective endocarditis is a serious infection of the heart’s inner lining and valves. It can damage the valve leaflets, making them thick and potentially causing stenosis. The risk is higher in people with heart conditions or a history of intravenous drug use.
We know that infective endocarditis is a big risk because it can directly harm the aortic valve. It’s important to treat it quickly to avoid lasting damage.
Metabolic Disorders
Some metabolic disorders can lead to aortic stenosis. For example, problems with calcium metabolism can cause the valve to calcify. These metabolic factors are important to consider when looking at patients with aortic stenosis.
| Metabolic Disorder | Effect on Aortic Valve |
|---|---|
| Abnormal Calcium Metabolism | Calcification |
| Hyperparathyroidism | Valvular Calcification |
Systemic Conditions: Alkaptonuria and Ochronosis
Alkaptonuria is a rare genetic disorder that affects amino acid metabolism. It leads to the buildup of homogentisic acid, causing ochronosis. Ochronosis can damage the valve and cause stenosis.
While Alkaptonuria and ochronosis are rare, they are important causes of aortic stenosis. Early diagnosis and treatment can help reduce their impact on the heart.
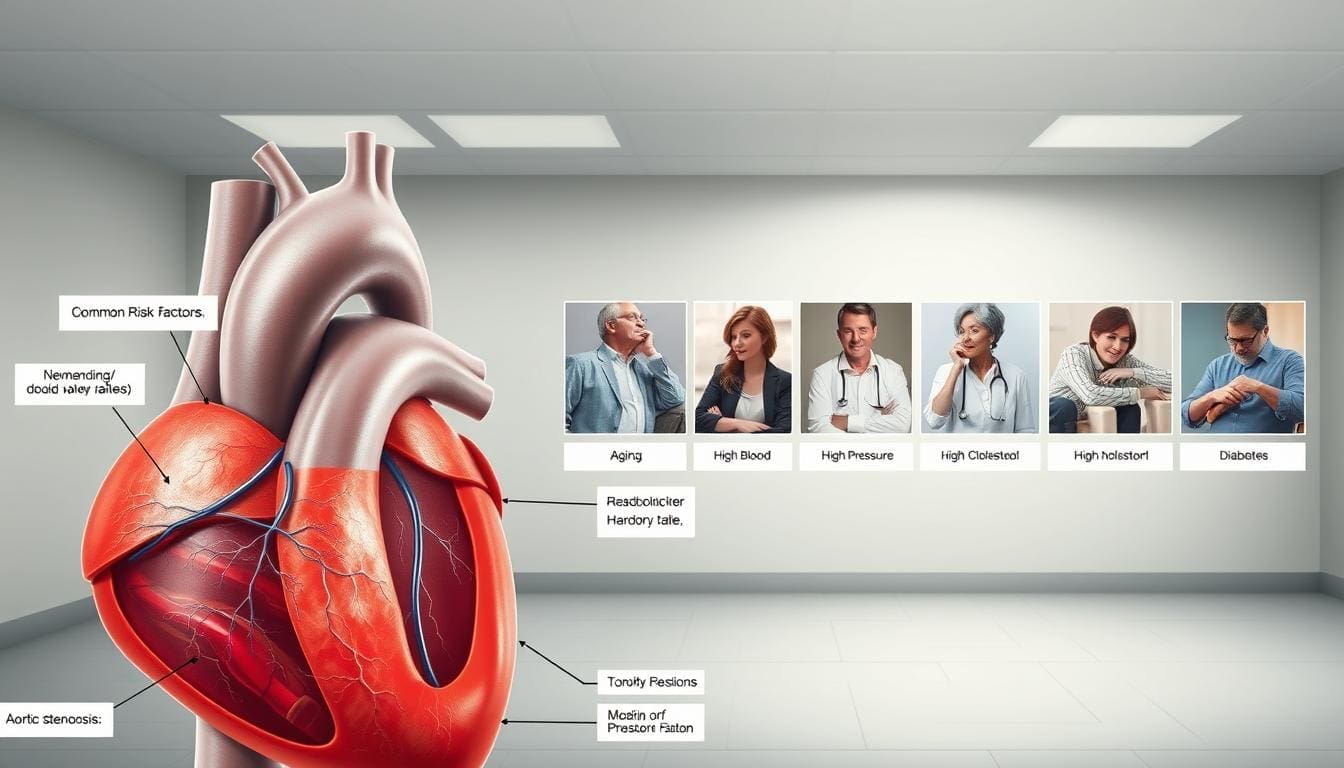
Risk Factors for Developing Aortic Stenosis
Aortic stenosis can be caused by genetics, environment, and lifestyle. Knowing these factors helps us spot who’s at risk early. This can help prevent or slow down the condition.
Age and Gender Considerations
Age is a big risk factor for aortic stenosis, with older adults more likely to get it. Calcific aortic stenosis, the most common type, is linked to aging. As we get older, our aortic valve can calcify, causing stenosis. Men are more at risk than women, even in younger years.
Studies show a big jump in aortic stenosis cases after 65. Regular heart checks are key for seniors. Men tend to get aortic stenosis younger than women, but why isn’t fully understood.
Genetic Predispositions
Genetics also play a part in aortic stenosis risk. Those with a family history of heart valve issues or certain genetic conditions face higher risks. A bicuspid aortic valve, with only two cusps, is prone to stenosis or regurgitation.
“Genetic predispositions play a significant role in the development of aortic stenosis, particular in cases of congenital heart defects like bicuspid aortic valve.”
Lifestyle and Environmental Factors
Lifestyle and environment also affect aortic stenosis risk. A diet rich in saturated fats and cholesterol can lead to calcific aortic stenosis. Smoking harms the heart and increases disease risk.
Staying active is good for the heart, but those with heart issues should talk to their doctor first. Making lifestyle changes can reduce some aortic stenosis risks.
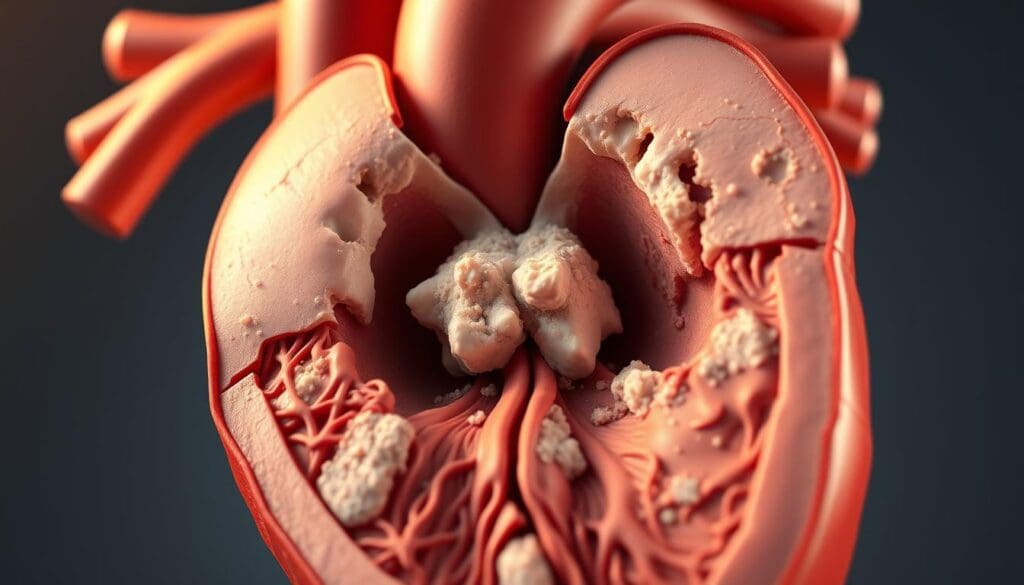
The Pathophysiology of Aortic Stenosis
Understanding aortic stenosis is key to knowing how it affects the heart. This condition narrows the aortic valve opening. This narrowing blocks blood flow from the left ventricle to the aorta. It changes the heart’s structure and function a lot.
Normal Valve Function vs. Stenotic Valve
In a healthy heart, the aortic valve lets blood flow freely. But in aortic stenosis, the valve narrows, blocking blood flow. This makes the left ventricle work harder to pump blood through the narrow valve.
Normal Aortic Valve Function: The aortic valve has three cusps that open and close with each heartbeat. This ensures blood flows without any blockage.
Stenotic Aortic Valve: The cusps get stiff and calcified. This makes the valve unable to open fully, blocking blood flow.
Hemodynamic Changes in Aortic Stenosis
As aortic stenosis gets worse, blood flow gets blocked. This increases pressure in the left ventricle. The increased pressure helps keep blood flowing to the aorta and the body.
“The development of aortic stenosis is associated with significant hemodynamic changes, including increased left ventricular pressure and wall thickness.” –
The changes in blood flow can be summarized as follows:
| Hemodynamic Parameter | Normal | Aortic Stenosis |
|---|---|---|
| Left Ventricular Pressure | Normal | Increased |
| Left Ventricular Wall Thickness | Normal | Increased |
| Aortic Valve Area | Normal (>2.0 cm) | Reduced (2) |
The Pressure-Overload Phenomenon
The left ventricle works harder due to the stenotic valve. At first, it thickens its walls to cope. But over time, it can’t keep up, leading to heart failure.
The shift from coping to failure involves complex changes at a cellular and molecular level. When the left ventricle can’t pump well, symptoms like shortness of breath, chest pain, and fainting may appear.
We can summarize the key points of the pressure-overload phenomenon as follows:
- Increased left ventricular pressure due to stenotic valve
- Left ventricular hypertrophy as a compensatory mechanism
- Eventual progression to heart failure
As stenosis gets worse, the left ventricle keeps thickening. But it eventually fails to pump enough blood, leading to heart failure.
From Compensation to Failure: The Heart’s Response
As aortic stenosis gets worse, the heart changes a lot to keep working. At first, the heart tries to handle the extra work from the blocked valve.
Left Ventricular Hypertrophy as an Adaptive Mechanism
The heart gets thicker to push blood harder. This is called left ventricular hypertrophy. It helps the heart keep pumping blood, even with the blockage.
But, this thickening needs more oxygen. It can cause an oxygen imbalance, leading to heart problems.
Diastolic Dysfunction Development
The thickened heart has trouble relaxing and filling. This is called diastolic dysfunction. It makes the heart work harder to fill up.
This can cause breathing problems, even if the heart is pumping well. It’s a big step towards heart failure.
Transition to Systolic Dysfunction
With time, the heart can’t push blood out as well. This is systolic dysfunction. It means the heart can’t pump enough blood.
The heart’s journey from coping to failing is complex. Knowing these changes helps manage aortic stenosis complications better.
In summary, the heart tries to adapt to aortic stenosis at first. Then, it develops diastolic and systolic dysfunction. Spotting these changes early is key to helping the heart.
How Aortic Stenosis Leads to Heart Failure
Aortic stenosis turning into heart failure is a complex process. It involves many changes in the body. The heart struggles more as the valve gets narrower.
The Failing Compensatory Mechanisms
At first, the heart tries to work harder because of the narrowed valve. It does this through left ventricular hypertrophy. But, these efforts fail as the stenosis gets worse.
The left ventricle, which pumps blood, gets overworked. It becomes thick, known as hypertrophy. This is not a long-term solution.
Reduced Cardiac Output and Its Consequences
As aortic stenosis gets worse, the heart can’t pump blood well. This leads to reduced cardiac output. Symptoms include fatigue, shortness of breath, and less ability to exercise.
People may also feel chest pain (angina) and faint (syncope). These signs show the heart’s struggle to keep blood flowing.
The Vicious Cycle of Heart Failure
Heart failure starts a vicious cycle. The heart’s reduced pumping ability puts more strain on it. This makes the condition worse.
When the heart can’t meet the body’s needs, fluid builds up. Heart pressure increases, and cardiac function declines. Without treatment, this can lead to severe problems.
It’s important to understand how aortic stenosis leads to heart failure. Recognizing symptoms and knowing the causes helps doctors treat it better. This can improve patient outcomes.
Recognizing Aortic Stenosis: Symptoms and Clinical Presentation
Aortic stenosis often starts quietly, making it key to know its signs. It’s important to catch it early. Early detection can greatly improve treatment and results.
The Asymptomatic Phase
In the early stages, aortic stenosis may not show symptoms, known as the asymptomatic phase. Even though it’s quiet, the valve can be severely narrowed. Regular health checks and echocardiograms are essential for catching and tracking aortic stenosis in those without symptoms.
Classic Triad: Dyspnea, Angina, and Syncope
As aortic stenosis gets worse, a classic triad of symptoms appears: dyspnea (shortness of breath), angina (chest pain), and syncope (fainting). These signs mean the disease is advanced and need quick medical attention.
- Dyspnea happens because the heart has trouble pumping, raising lung pressure.
- Angina occurs when the heart muscle doesn’t get enough oxygen-rich blood.
- Syncope happens when the heart can’t pump more during effort, causing fainting.
Signs of Advancing Heart Failure
In later stages, aortic stenosis can cause heart failure. Symptoms include tiredness, leg swelling, and breathing problems even when sitting. Spotting these signs is critical, as they signal a serious and potentially deadly condition.
Knowing the symptoms and signs of aortic stenosis is key for early diagnosis and treatment. We stress the need for regular health checks and educating patients to better manage this condition.
Treatment Options for Aortic Stenosis
Today, treating aortic stenosis includes many methods, from managing symptoms to new surgeries. The right treatment depends on how severe the symptoms are, the patient’s health, and any other health issues.
Medical Management of Symptoms
For those without symptoms, regular check-ups are key. But, when symptoms appear, treatment is needed to ease them and slow the disease. Doctors use medicines to control symptoms and manage related problems like high blood pressure and heart failure. They might prescribe diuretics, beta-blockers, and ACE inhibitors.
Surgical Valve Replacement
Surgical aortic valve replacement (SAVR) is a common and effective treatment for severe aortic stenosis. It’s a surgery that replaces the old valve with a new one. But, it’s a big surgery with risks, mainly for older patients or those with other health issues.
Choosing SAVR is a big decision. We consider the patient’s age, health, and other heart problems to decide if it’s the best option.
Transcatheter Aortic Valve Replacement (TAVR)
Transcatheter aortic valve replacement (TAVR) is a less invasive option, mainly for those at high risk for surgery. It uses a catheter to put in a new valve, either through the leg or a small chest incision. This method can help patients who can’t have open-heart surgery.
TAVR technology has improved a lot, with newer devices leading to better results and more uses. We choose between TAVR and SAVR based on the patient’s condition and needs.
In summary, treating aortic stenosis involves many options, including managing symptoms, SAVR, and TAVR. We tailor our treatment to each patient, aiming to improve their life and health.
Conclusion: Prevention Strategies and Prognosis
Understanding how to prevent and manage aortic stenosis is key. Early detection and proper care can greatly improve outcomes. By focusing on prevention, we can lower the risk of this condition and its complications.
The outlook for aortic stenosis patients depends on several factors. These include how severe the condition is and if they have other health issues. Regular check-ups and timely treatment are vital to manage the condition and prevent heart failure. We suggest that those at risk get regular echocardiograms to watch their valve health.
By being proactive in preventing and managing aortic stenosis, we can better the outlook for those affected. This includes making lifestyle changes, managing other health conditions, and getting timely surgery or procedures. A team effort is needed to effectively manage aortic stenosis, and we’re dedicated to providing top-notch care.
What is aortic stenosis?
Aortic stenosis is when the aortic valve gets narrower. This can lead to heart failure if not treated.
What are the primary causes of aortic stenosis?
Main causes include age-related calcification, congenital bicuspid aortic valve, and rheumatic heart disease.
How does age-related calcific degeneration contribute to aortic stenosis?
Calcium builds up on the aortic valve with age. This causes it to narrow and become stenotic.
What is the role of congenital bicuspid aortic valve in aortic stenosis?
A congenital bicuspid aortic valve has only two cusps. This increases the risk of aortic stenosis.
What are the risk factors for developing aortic stenosis?
Risk factors include age, male gender, and genetic predispositions. Lifestyle factors like smoking and high blood pressure also play a role.
How does aortic stenosis progress to heart failure?
Aortic stenosis leads to heart failure when the heart can’t handle the pressure. This reduces cardiac output and leads to heart failure.
What are the symptoms of aortic stenosis?
Symptoms include shortness of breath, chest pain, and fainting. These can worsen to signs of heart failure like fatigue and swelling.
What are the treatment options for aortic stenosis?
Treatments include managing symptoms, surgical valve replacement, and TAVR.
Can aortic stenosis be prevented?
Some risk factors can’t be prevented. But managing high blood pressure and a healthy lifestyle can reduce risk.
What is the prognosis for patients with aortic stenosis?
Prognosis depends on the condition’s severity and treatment success. Early detection and management improve outcomes.
What is calcific aortic stenosis?
Calcific aortic stenosis is caused by calcium deposits on the aortic valve. This leads to narrowing.
How does rheumatic heart disease cause aortic stenosis?
Rheumatic heart disease can cause aortic stenosis by scarring and fusing the valve leaflets. This results in valve stenosis.
References
NCBI Bookshelf (National Library of Medicine): Aortic Stenosis (Specific NCBI ID)
PubMed (NCBI): Aortic Valve Stenosis and Mortality (Specific PubMed ID)
American Academy of Family Physicians (AAFP): Aortic Stenosis (Journal Article)




































