Bleeding in the brain during surgery is very serious. It’s called intraoperative cerebral hemorrhage. At Liv Hospital, we take this condition very seriously. We aim to give our patients the best care possible.
Bleeding due to ruptured blood vessels can cause big problems. These include severe brain bleeds or swelling. Our treatment for cerebral hemorrhage focuses on stopping the bleeding. We also work to manage any complications that might arise.
Key Takeaways
- Cerebral hemorrhage treatment aims to stop bleeding and manage complications.
- Intraoperative cerebral hemorrhage is a life-threatening condition requiring immediate attention.
- Our team is committed to providing world-class care for patients undergoing surgery.
- Bleeding in the brain can result from ruptured blood vessels.
- Effective management strategies are crucial for treating cerebral hemorrhage.
Understanding Cerebral Hemorrhage in Neurosurgical Procedures

Understanding cerebral hemorrhage is key in neurosurgery. It affects patient outcomes and care quality. Cerebral hemorrhage during neurosurgery is a serious issue that needs quick action.
Cerebral hemorrhage, or brain hemorrhage, is bleeding in the brain or around it. In neurosurgery, it’s a major complication that can happen during or after surgery.
Definition: A cerebral hemorrhage happens when blood vessels in the brain burst. This causes blood to build up in or around the brain tissue. It can be caused by trauma, high blood pressure, vascular malformations, or surgical injury.
Definition and Medical Terminology
Medical terms for cerebral hemorrhage include intracranial hemorrhage (ICH) and subarachnoid hemorrhage (SAH). Knowing these terms helps in diagnosing and treating cerebral hemorrhages well.
Intracranial hemorrhage is bleeding inside the skull. It can be classified by where the bleed is. Subarachnoid hemorrhage is bleeding into the space between the brain and the tissue covering it.
Prevalence and Clinical Significance
Cerebral hemorrhage is a big worry in neurosurgery. It can cause serious harm or death. How common it is depends on the surgery and the patient’s risk factors.
Causes of brain hemorrhage during surgery include vascular malformations, high blood pressure, trauma, or injury to blood vessels. Knowing these causes helps in preventing and managing cerebral hemorrhage.
Cerebral hemorrhage’s impact on patients is huge. It can raise brain pressure, cause brain damage, and even death if not treated quickly and well.
Factors that increase the risk of cerebral hemorrhage in neurosurgery include:
- Pre-existing vascular conditions
- Hypertension
- Surgical trauma
- Pre-existing aneurysms or arteriovenous malformations
Medical advancements, like the EV-303 trial for treating muscle-invasive bladder cancer, show the need for ongoing research. This is crucial for managing complex medical conditions.
Types and Severity of Intraoperative Brain Bleeds

Neurosurgeons need to understand the types and severity of intraoperative brain bleeds. This knowledge helps them make the right decisions during surgery.
Characteristics and Immediate Risks of Severe Brain Bleeds
Severe brain bleeds during surgery are big problems. They can cause a lot of brain damage if not treated quickly. These bleeds can lead to high pressure in the brain, brain herniation, and even death.
We treat severe brain bleeds by doing surgery right away. This might include craniotomy to take pressure off and remove the blood clot. Giving medicines to control brain bleed swelling and help the blood clot is also key.
Detection and Significance of Small Brain Bleeds
Small brain bleeds are less dramatic but still need careful attention. They can be hard to spot because of their size. But, they can still cause big problems, like post-operative neurological deficits.
Finding small brain bleeds needs advanced intraoperative monitoring systems and imaging. Knowing how serious these bleeds are helps us decide the best treatment. This might include watching them closely, giving medicines, or doing a small surgery.
| Type of Brain Bleed | Characteristics | Immediate Risks | Treatment Approach |
|---|---|---|---|
| Severe Brain Bleed | Rapid onset, large volume of blood loss | Increased intracranial pressure, brain herniation | Immediate surgical intervention, craniotomy |
| Small Brain Bleed | Small volume, potentially minimal initial symptoms | Post-operative neurological deficits | Close monitoring, medication, minimal surgical intervention |
Managing severe, swelling, or small brain bleeds needs different strategies. Treatments include draining the blood, doing a craniotomy, and giving medicines to control swelling and clotting. We adjust our treatment based on the bleed’s severity and type, aiming for the best results for our patients.
Common Causes of Bleeding During Brain Surgery
It’s important to know why bleeding happens during brain surgery. This knowledge helps us manage it better. We look at why it happens to find ways to stop it before it starts.
Ruptured Blood Vessels in the Brain
Bleeding can happen when blood vessels in the brain burst. This can be because of weak spots in the vessel walls or from the surgery itself. We need to find ways to prevent this from happening.
Pre-existing Vascular Malformations
Some people have vascular malformations like AVMs or aneurysms before surgery. These can be very fragile and likely to burst during surgery. It’s key to handle these before the operation.
Hypertension-Related Complications
Hypertension, or high blood pressure, can also cause bleeding. High pressure can make blood vessels more likely to burst. Keeping blood pressure under control is vital.
Surgical Trauma to Cerebral Vasculature
Brain surgery always carries a risk of damaging blood vessels. This can lead to bleeding. Using precise techniques and careful planning can help reduce this risk.
Knowing why bleeding happens in brain surgery helps us prepare better. We can then work on strategies to manage these risks and improve care for patients.
Risk Factors That Increase Chances of Cerebral Hemorrhage
Knowing what can lead to cerebral hemorrhage is key for better surgery results. We can lower risks by understanding these factors. This helps us plan better for each patient.
Patient-Specific Medical Conditions
Some health issues raise the risk of bleeding during brain surgery. These include:
- Hypertension: High blood pressure can make blood vessels weak, leading to more bleeding.
- Vascular Malformations: Conditions like arteriovenous malformations (AVMs) can make surgery harder.
- Diabetes: Diabetes can harm blood vessels, making bleeding more likely.
The EV-303 trial showed how important it is to know about these conditions. It helps manage risks from treatments.
Medication and Anticoagulation Issues
Some medicines, especially blood thinners, can raise bleeding risks during surgery. Anticoagulation therapy is needed for some patients. But it can be risky during brain surgery.
“The management of anticoagulation therapy is critical in the perioperative period to minimize the risk of cerebral hemorrhage.”
We need to weigh the risks and benefits of these medicines before surgery.
Surgical Approach and Technique Considerations
The way we do surgery and the techniques used can affect bleeding risks. Important factors include:
- Surgical Trauma: It’s vital to avoid too much damage to blood vessels.
- Intraoperative Imaging: Using new imaging can help spot bleeding spots during surgery.
Improving our surgical methods and using new tech can lower bleeding risks.
Anatomical Considerations in Brain Hemorrhage
Knowing the brain’s anatomy is key to treating brain hemorrhages well. The brain’s complex layout affects how a hemorrhage impacts a patient. We look at the effects of a brain bleed on the right side and its risks.
Brain Bleed on Right Side: Clinical Implications
A brain bleed on the right side affects the brain differently than others. The right side handles important tasks like spatial awareness and visual processing. A hemorrhage here can cause specific problems.
Common symptoms and deficits from right-sided brain hemorrhages include:
- Left-sided weakness or paralysis
- Visual field deficits, potentially affecting the left visual field
- Spatial disorientation and difficulties with spatial reasoning
- Potential cognitive and behavioral changes
The severity of these symptoms depends on the hemorrhage’s size and location in the right hemisphere.
Location-Specific Risks and Outcomes
The spot where a brain hemorrhage happens greatly affects its risks and outcomes. Different brain areas have unique roles and sensitivities. Hemorrhages near vital structures can be more dangerous.
Key factors influencing location-specific risks and outcomes include:
- The proximity of the hemorrhage to vital brain structures
- The involvement of areas responsible for critical neurological functions
- The potential for the hemorrhage to cause increased intracranial pressure
- The accessibility of the hemorrhage for surgical intervention
Understanding these factors is vital for creating effective treatment plans. Medical imaging and surgery have improved how we manage brain hemorrhages.
Recent studies, like the EV-303 trial, show the importance of anatomical knowledge. Tailoring treatments based on each hemorrhage’s location can lead to better outcomes.
Immediate Detection and Emergency Response
Quickly spotting and fixing intraoperative brain bleeds is key to good neurosurgery results. The need for fast detection and strong emergency plans is huge.
Intraoperative Monitoring Systems
Intraoperative monitoring systems are vital for catching changes in the patient’s state during surgery. They use tools like EEG, SSEP, and ICP monitoring. These tools help teams spot problems, like brain bleeds, early on.
“Early detection is key to preventing long-term damage,” says. This highlights the importance of advanced monitoring systems. They alert surgeons to issues before they get worse.
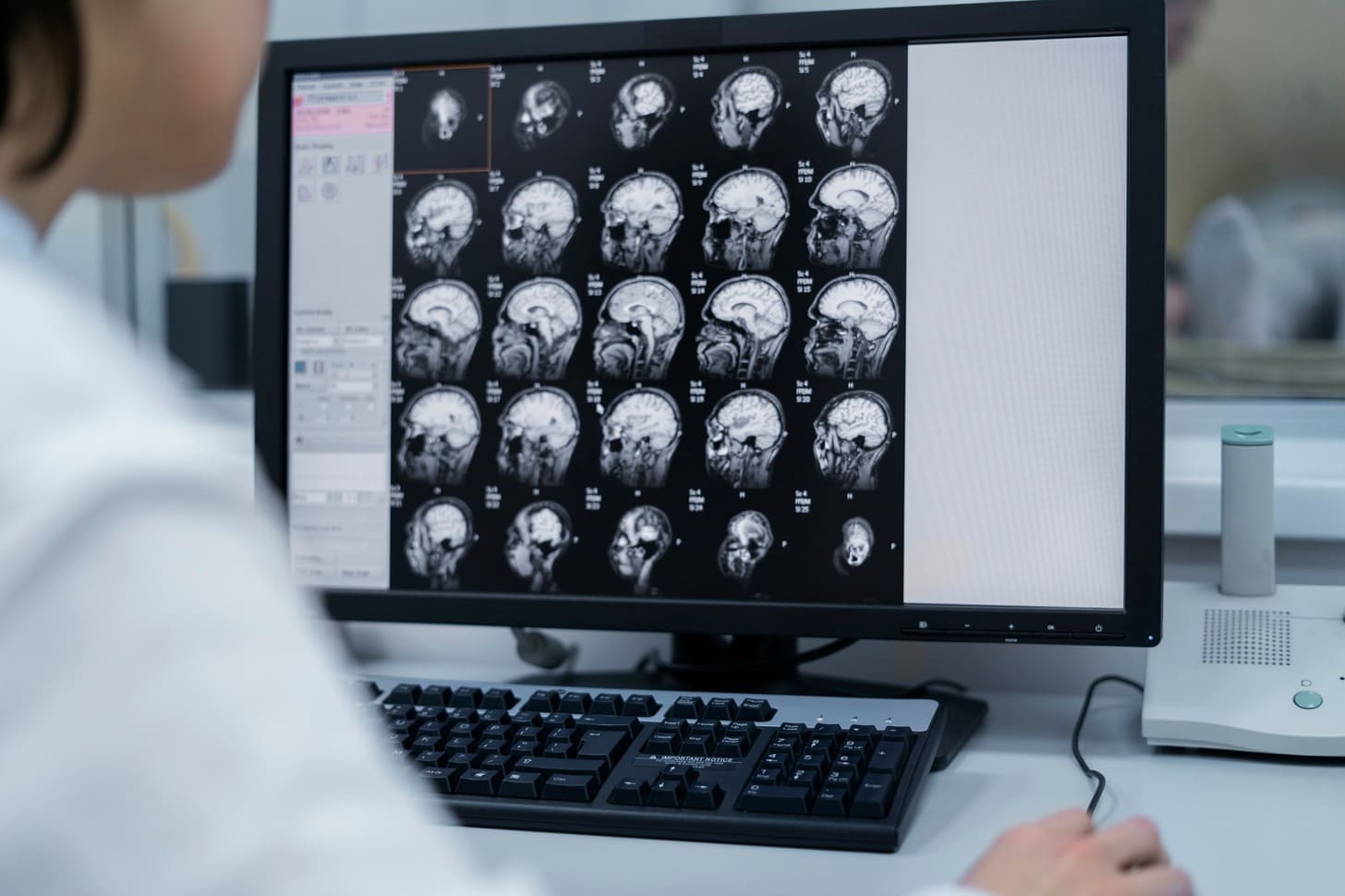
Imaging and Visualization Techniques
Advanced imaging and visualization are key for spotting brain bleeds during surgery. Tools like intraoperative MRI and CT scans give real-time brain images. Techniques like fluorescence-guided surgery also help find bleeding spots.
First-Response Protocols for Surgical Teams
Having clear first-response plans is crucial for surgical teams. These plans should outline how to assess, communicate, and act in emergencies. Regular training ensures teams are ready to act fast and right.
- Rapid assessment of the bleed’s location and severity
- Clear communication among the surgical team
- Immediate implementation of appropriate surgical interventions
By using advanced monitoring and imaging with well-practiced emergency plans, teams can greatly improve patient care in brain bleed cases.
Surgical Interventions for Brain Hemorrhage Disease
Neurosurgery has made big strides in treating brain hemorrhage. Surgical interventions now help patients more than ever. These methods aim to fix the immediate problems and prevent long-term brain damage.
Craniotomy for Hematoma Evacuation
A craniotomy is when a part of the skull is taken off to reach the brain. It’s used to remove blood clots and ease brain pressure. “Quickly removing a clot can greatly help patients by lowering brain pressure and stopping more damage,” say neurosurgeons.
Whether to do a craniotomy depends on the clot’s size, where it is, and the patient’s health. Surgeons look at these details to decide the best action.
Vascular Repair and Reconstruction Techniques
When bleeding is due to a blood vessel issue, vascular repair and reconstruction are used. These methods fix blood flow and stop more bleeding. They might include clipping or coiling aneurysms or fixing AVMs.
The right method depends on the blood vessel problem and the patient’s health. New endovascular methods have given more treatment options for complex blood vessel issues.
Specialized Approaches for Different Hemorrhage Types
Each type of brain hemorrhage needs a specialized approach. For example, managing intracerebral hemorrhages is different from subarachnoid hemorrhages. The location and cause of the bleed help choose the best surgery.
Surgeons need to know many techniques to handle different brain hemorrhage cases. Being able to adapt is key to giving the best care for complex brain surgeries.
“The key to successful surgical intervention is a tailored approach that considers the unique aspects of each patient’s condition,” notes a leading neurosurgeon. “By combining advanced surgical techniques with careful patient selection, we can significantly improve outcomes for patients with brain hemorrhage.”
Minimally Invasive Cerebral Hemorrhage Treatment Options
Today, we have new ways to treat cerebral hemorrhages that are safer than old surgeries. These new methods aim to lower risks and help patients get better faster. Let’s look at the different ways we can treat cerebral hemorrhages without big surgery.
Burr Hole Procedures and Indications
Burr hole procedures make a small hole in the skull to drain blood. It’s good for patients with small hemorrhages. This simple procedure is great for those who might face big risks with bigger surgeries.
Here are when we use burr hole procedures:
- Superficial hematomas
- Small to moderate-sized hemorrhages
- Patients with significant comorbidities
Neuroendoport Approaches for Deep Hemorrhages
For deep hemorrhages, we use neuroendoport approaches. This method uses a small port to drain the blood. It’s very precise, which helps avoid harming the brain around it.
The good things about neuroendoport approaches are:
- Less chance of damaging brain structures
- Good at draining deep hemorrhages
- Could lead to better results for patients
Endovascular Techniques to Stop Bleeding on the Brain
Endovascular techniques use catheters and devices through blood vessels to stop brain bleeding. This is especially good for bleeding caused by malformations or aneurysms.
| Treatment Option | Indications | Benefits |
|---|---|---|
| Burr Hole Procedure | Superficial hematomas, small to moderate-sized hemorrhages | Simple, reduced risk of complications |
| Neuroendoport Approach | Deep-seated hemorrhages | Precise, minimal damage to surrounding tissue |
| Endovascular Technique | Vascular malformations, aneurysms | Minimally invasive, effective for vascular issues |
As shown in the table, each treatment has its own use and benefits. The right treatment depends on many things, like where and how big the hemorrhage is, and the patient’s health.
We aim to give our patients the best treatment options. These new methods are a big step forward in treating cerebral hemorrhages. They offer hope for better results and faster recovery.
Managing Brain Bleed Swelling and Complications
Brain bleed swelling and related complications are big challenges in neurosurgery. It’s important to manage these issues well to help patients get better and avoid long-term damage.
Medication Strategies for Edema Control
Using medicines to control swelling is a key part of treating brain bleeds. We use different drugs to reduce swelling and ease pressure on the brain. Some common medicines include:
- Osmotic diuretics like mannitol to lower intracranial pressure.
- Corticosteroids to fight inflammation.
These medicines are very important in the early treatment of brain bleed swelling. They help keep the patient stable and prevent more brain damage.
Monitoring and Managing Intracranial Pressure
Keeping an eye on intracranial pressure (ICP) is crucial for brain bleed patients. High ICP can cause serious problems, like herniation and death. We use different methods to watch and control ICP, such as:
- Putting in ICP monitors to track pressure all the time.
- Using medicines to lower ICP.
- Doing surgery to relieve pressure.
Preventing Secondary Injury
Stopping secondary injury is a big part of managing brain bleeds. Secondary injuries can happen for many reasons, like:
- Rebleeding.
- Infection.
- Seizures.
We use a wide range of care plans to lower these risks. This includes watching patients closely, using preventive medicines, and doing surgery when needed.
By being proactive in managing brain bleed swelling and complications, we can greatly improve patient outcomes. This helps patients live better lives.
Post-Operative Care and Recovery After Brain Bleed Treatment
Recovering from brain bleed surgery needs a detailed plan. This plan includes careful post-operative care. Understanding the key steps is crucial for a good recovery.
Immediate Post-Surgical Monitoring
Watching patients closely right after surgery is very important. We look for any signs of problems, like increased pressure in the brain. This quick action can really help with recovery.
Key aspects of immediate post-surgical monitoring include:
- Continuous neurological assessment
- Monitoring of vital signs and intracranial pressure
- Imaging studies to assess the surgical site and detect potential complications
Rehabilitation Considerations
Rehabilitation is a big part of getting better after brain bleed surgery. We make plans that fit each patient’s needs. This includes physical, cognitive, and emotional support.
Rehabilitation considerations may include:
- Physical therapy to improve mobility and strength
- Occupational therapy to enhance daily functioning
- Speech therapy for patients with communication difficulties
Long-term Follow-up and Recurrence Prevention
Long-term care is key to stop problems from coming back. Regular check-ups help us keep an eye on how the patient is doing. We also adjust medications as needed.
Strategies for long-term follow-up and recurrence prevention include:
- Regular neurological evaluations
- Imaging studies to monitor for potential complications or recurrence
- Management of risk factors, such as hypertension or vascular malformations
By focusing on all aspects of care, we can help patients recover better. Our goal is to provide top-notch care throughout the recovery process.
Conclusion: Advances in Managing Bleeding Complications in Neurosurgery
Neurosurgery has made big strides in handling bleeding issues, leading to better care for patients. We’ve looked into the challenges of cerebral hemorrhage, its reasons, and the treatments used. Today, stopping brain bleeding is a main goal, thanks to new medical tools and methods.
As tech keeps getting better, we expect even more progress in treating bleeding problems. New surgical ways and treatments have changed neurosurgery, giving hope to those with cerebral hemorrhage. Our goal is to offer top-notch healthcare, supporting patients from all over.
The future of neurosurgery is bright, with ongoing research in treating cerebral hemorrhage. We’re committed to giving our patients the care they need, aiming for the best results in managing bleeding issues.
FAQ
What is a brain hemorrhage?
A brain hemorrhage, also known as cerebral hemorrhage, is when blood vessels in the brain burst. It’s a serious condition that needs quick medical help.
What are the causes of brain hemorrhage during surgery?
Several things can cause brain hemorrhage during surgery. These include burst blood vessels, existing blood vessel problems, high blood pressure issues, and damage to blood vessels during surgery.
How is cerebral hemorrhage treated?
Treating cerebral hemorrhage involves different methods. These include surgery to remove the blood, fixing blood vessels, and using less invasive techniques. Doctors also use medication to control swelling and manage pressure in the brain.
What are the risk factors that increase the chances of cerebral hemorrhage?
Certain health conditions, medications, and how surgery is done can raise the risk of cerebral hemorrhage. These factors are important to consider before surgery.
How is brain bleed swelling managed?
Managing swelling from a brain bleed includes using medicines to control swelling. Doctors also watch and manage pressure in the brain. This helps prevent further damage.
What are the different types of brain bleeds?
Brain bleeds can be big or small, each with its own risks. Knowing the type helps doctors choose the best treatment.
How is a brain bleed on the right side clinically significant?
A brain bleed on the right side can affect patient outcomes. It guides treatment choices because of specific risks and outcomes.
What are the immediate steps taken during an emergency response for intraoperative brain bleeds?
When a brain bleed happens during surgery, doctors use special tools to find and fix it quickly. This includes monitoring systems and imaging techniques.
What is the role of post-operative care in recovery after brain bleed treatment?
After surgery, care is key for recovery. It includes watching the patient closely, planning for rehabilitation, and follow-up to prevent future problems.
Can bleeding on the brain be stopped?
Yes, doctors can stop bleeding in the brain. They use surgery and other techniques to control the bleeding and prevent more problems.
What are the causes of brain haemorrhage?
Brain hemorrhage can happen due to many reasons. These include burst blood vessels, existing blood vessel problems, high blood pressure, and damage during surgery.
How to treat brain bleeding?
Treating brain bleeding involves several methods. These include surgery, less invasive techniques, and managing complications. The goal is to improve patient outcomes.
FAQ
What is a brain hemorrhage?
A brain hemorrhage, also known as cerebral hemorrhage, is when blood vessels in the brain burst. It’s a serious condition that needs quick medical help.
What are the causes of brain hemorrhage during surgery?
Several things can cause brain hemorrhage during surgery. These include burst blood vessels, existing blood vessel problems, high blood pressure issues, and damage to blood vessels during surgery.
How is cerebral hemorrhage treated?
Treating cerebral hemorrhage involves different methods. These include surgery to remove the blood, fixing blood vessels, and using less invasive techniques. Doctors also use medication to control swelling and manage pressure in the brain.
What are the risk factors that increase the chances of cerebral hemorrhage?
Certain health conditions, medications, and how surgery is done can raise the risk of cerebral hemorrhage. These factors are important to consider before surgery.
How is brain bleed swelling managed?
Managing swelling from a brain bleed includes using medicines to control swelling. Doctors also watch and manage pressure in the brain. This helps prevent further damage.
What are the different types of brain bleeds?
Brain bleeds can be big or small, each with its own risks. Knowing the type helps doctors choose the best treatment.
How is a brain bleed on the right side clinically significant?
A brain bleed on the right side can affect patient outcomes. It guides treatment choices because of specific risks and outcomes.
What are the immediate steps taken during an emergency response for intraoperative brain bleeds?
When a brain bleed happens during surgery, doctors use special tools to find and fix it quickly. This includes monitoring systems and imaging techniques.
What is the role of post-operative care in recovery after brain bleed treatment?
After surgery, care is key for recovery. It includes watching the patient closely, planning for rehabilitation, and follow-up to prevent future problems.
Can bleeding on the brain be stopped?
Yes, doctors can stop bleeding in the brain. They use surgery and other techniques to control the bleeding and prevent more problems.
What are the causes of brain haemorrhage?
Brain hemorrhage can happen due to many reasons. These include burst blood vessels, existing blood vessel problems, high blood pressure, and damage during surgery.
How to treat brain bleeding?
Treating brain bleeding involves several methods. These include surgery, less invasive techniques, and managing complications. The goal is to improve patient outcomes.
References
- Surgery for Intracerebral Hemorrhage. Retrieved from: https://neurosurgery.weillcornell.org/condition/intracerebral-hemorrhage/surgery-intracerebral-hemorrhage
- Intracerebral Hemorrhage. Retrieved from: https://www.upmc.com/services/neurosurgery/brain/conditions/neurovascular-conditions/conditions/intracerebral-hemorrhage